Abstract
Background
The optimal treatment for patients with perforated gastric ulcer (PGU) remains controversial. This study therefore investigated the treatment status for this disease in clinical practice.
Methods
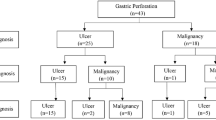
We retrospectively reviewed 183 patients with PGU from 1998 to 2007 across 15 institutions, and analyzed patient characteristics and short- and long-term outcomes according to treatments received.
Results
Of the 183 patients, 57 who were treated conservatively had less abdominal tenderness, lower levels of serum C-reactive protein, and shorter time to presentation than the 126 patients who underwent emergency surgery. There was no significant difference in baseline characteristics between the 41 successful patients and 16 failed patients in the conservative treatment group; however, the latter had a longer average hospital stay. Eighty-three of the emergency surgery patients who underwent gastrectomy had longer surgical times, greater blood loss, and shorter time to resumption of diet than the 57 patients undergoing stomach-preserving surgery; however, there was no significant difference in postoperative complications and hospital stay between these groups. Of 91 patients who received stomach-preserving treatment, only three had treatment failure in the long-term follow-up period.
Conclusion
Strictly selected patients should be initially considered for conservative treatment. The short-term outcomes of stomach-preserving surgery are comparable to gastrectomy; however, further evaluation of the long-term outcomes of stomach-preserving treatment is required.

Similar content being viewed by others
References
Bae S, Shim KN, Kim N, Kang JM, Kim DS, Kim KM, Cho YK, Jung SW. Incidence and short-term mortality from perforated peptic ulcer in Korea: a population-based study. J Epidemiol 2012; 22(6): 508–516.
Hermansson M, Ekedahl A, Ranstam J, Zilling T. Decreasing incidence of peptic ulcer complications after the introduction of the proton pump inhibitors, a study of the Swedish population from 1974–2002. BMC Gastroenterology 2009; 9: 25.
Lassen A, Hallas J, Schaffalitzky de Muckadell OB. Complicated and uncomplicated peptic ulcer in a Danish country 1993–2002: a population-based cohort study. Am J Gastroenterol 2006; 101(5): 945–953.
Svanes C. Trends in perforated peptic ulcer: incidence, etiology, treatment, and prognosis. World J Surg 2000; 24(3): 277–283.
Bertleff MJ, Lange JF. Perforated peptic ulcer disease: a review of history and treatment. Dig Surg 2010; 27(3): 161–169.
Thorsen K, Glomsaker TB, von Meer A, Soreide K, Soreide JA. Trends in diagnosis and surgical management of patients with perforated peptic ulcer. J Gastrointest Surg 2011; 15(8): 1329–1335.
Hemmer PH, de Schipper JS, van Etten B, Pierie JP, Bonenkamp JJ, de Graaf PW, Karsten TM. Results of surgery for perforated gastroduodenal ulcers in a dutch population. Dig Surg 2001; 28: 360–366.
Thorsen K, Søreide JA, Kvaløy JT, Glomsaker T, Søreide K. Epidemiology of perforated peptic ulcer: Age- and gender- adjusted analysis of incidence and mortality. World J Gastroenterol 2013; 19(3): 347–354.
Hodnett RM, Gonzalez F, Lee WC, Nance FC, Deboisblanc R. The need for definitive therapy in the management of perforated gastric ulcer: review of 202 cases. Ann Surg 1989; 209(1): 36–39.
Horowitz J, Kukora JS, Ritchie WP Jr. All perforated ulcers are not alike. Ann Surg 1989; 209(6): 693–699.
Lanng C, Palnaes Hansen C, Christensen A, Thagaard CS, Lassen M, Klaerke A, Tonnesen H, Ostgaard SE. Perforated gastric ulcer. Br J Surg 1988; 75(8): 758–759.
The Japanese Society of Gastroenteology. Evidence-based clinical practice guidelines for peptic ulcer disease (in Japanese). Tokyo: Nankodo, 2009.
Crofts TJ, Park KG, Steele RJ, Chung SS, Li AK. A randomized trial of nonoperative treatment for perforated peptic ulcer. N Engl J Med 1989; 320(15): 970–973.
Kuwabara K, Matsuda S, Fusimi K Ishikawa KB, Horiguchi H, Fujimori K. Reappraising the surgical approach on the perforated gastroduodenal ulcer: should gastric resection be abandoned? J Clin Med Res 2011; 3(5):213–222.
Noguiera C, Silva AS, Santos JN, Silva AG, Ferreira J, Matos E, Vilaca H. Perforated peptic ulcer: main factors of morbidity and mortality. World J Surg 2003; 27(7): 782–787.
Rodriguez-Sanjuan JC, Fernandez-Santiago R, Garcia RA, Trugeda S, Seco I, la de Torre F, Naranjo A, Gomez-Fleitas M. Perforated peptic ulcer treated by simple closure and Helicobacter pylori eradication. World J Surg 2005; 29(7): 849–852.
Kate V, Ananthakrishnan N, Nadrinath S. Effect of Helicobacter pylori eradication on the ulcer recurrence rate after simple closure of perforated duodenal ulcer: retrospective and prospective randomized controlled studies. Br J Surg 2001; 88: 1054–1058.
Ng EK, Lam YH, Sung JJ, Yung MY, To KF, Chan AC, Lee DW, Law BK, Lau JY, Ling TK, Lau WY, Chung SC. Eradication of Helicobacter pylori prevents recurrence of ulcer after simple closure of duodenal ulcer perforation: randomized controlled trial. Ann Surg 2000; 231(2): 153–158.
Sanabria A, Villegas MI, Morales Uribe CH. Laparoscopic repair for perforated peptic ulcer disease. Cochrane Database Syst Rev 2013; 2:CD004778.
Lunevicus R, Morkevicius M. Systematic review comparing laparoscopic and open repair for perforated peptic ulcer. Br J Surg 2005; 92(10): 1195–1207.
Siu WT, Leong HT, Law BK, Chau CH, Li AC, Fung KH, Tai YP, Li MK. Laparoscopic repair for perforated peptic ulcer: a randomized controlled trial. Ann Surg 2002; 235(3): 313–319.
Siu WT, Chau CH, Law BK, Tang CN, Ha PY, Li MK. Routine use of laparoscopic repair for perforated peptic ulcer. Br J Surg 2004; 91(4): 481–484.
Acknowledgments
We thank Drs. S. Shimoda (Shibata Hospital), N. Shimakage (Nagaoka Red Cross Hospital), K. Sato (Sado General Hospital), M. Hasegawa (Niigata Prefectural Central Hospital), H. Okamoto (Yoshida Hospital), K. Miyashita (Tsubame Rosai Hospital), T. Tada (Tachikawa General Hospital), K. Ueki (Kashiwazaki General Hospital and Medical Center), O. Sato (Shinrakuen Hospital), M. Ohtake (Niigata Saiseikai Sanjo Hospital), A. Nashimoto (Niigata Cancer Center Hospital), S. Tanaka (Niigata Prefectural Koide Hospital), T. Tomiyama (Toyosaka Hospital), and M. Sasagawa (Nanbugo General Hospital) for assistance with the data collection.
There are no sources of funding and/or publication about this manuscript.
Author information
Authors and Affiliations
Corresponding author
Additional information
This paper is not based on a previous communication to a society or meeting.
Rights and permissions
About this article
Cite this article
Tanaka, R., Kosugi, Si., Sakamoto, K. et al. Treatment for Perforated Gastric Ulcer: a Multi-institutional Retrospective Review. J Gastrointest Surg 17, 2074–2081 (2013). https://doi.org/10.1007/s11605-013-2362-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-013-2362-7