Abstract
Background
The present paper aims at evaluating the potential benefits of high-energy devices (HEDs) in the Italian surgical practice, defining the comparative efficacy and safety profiles, as well as the potential economic and organizational advantages for hospitals and patients, with respect to standard monopolar or bipolar devices.
Methods
A Health Technology Assessment was conducted in 2021 assuming the hospital perspective, comparing HEDs and standard monopolar/bipolar devices, within eleven surgical settings: appendectomy, hepatic resections, colorectal resections, cholecystectomy, splenectomy, hemorrhoidectomy, thyroidectomy, esophago-gastrectomy, breast surgery, adrenalectomy, and pancreatectomy. The nine EUnetHTA Core Model dimensions were deployed considering a multi-methods approach. Both qualitative and quantitative methods were used: (1) a systematic literature review for the definition of the comparative efficacy and safety data; (2) administration of qualitative questionnaires, completed by 23 healthcare professionals (according to 7-item Likert scale, ranging from − 3 to + 3); and (3) health-economics tools, useful for the economic evaluation of the clinical pathway and budget impact analysis, and for the definition of the organizational and accessibility advantages, in terms of time or procedures’ savings.
Results
The literature declared a decrease in operating time and length of stay in using HEDs in most surgical settings. While HEDs would lead to a marginal investment for the conduction of 178,619 surgeries on annual basis, their routinely implementation would generate significant organizational savings. A decrease equal to − 5.25/−9.02% of operating room time and to − 5.03/−30.73% of length of stay emerged. An advantage in accessibility to surgery could be hypothesized in a 9% of increase, due to the gaining in operatory slots. Professionals’ perceptions crystallized and confirmed literature evidence, declaring a better safety and effectiveness profile. An improvement in both patients and caregivers’ quality-of-life emerged.
Conclusions
The results have demonstrated the strategic relevance related to HEDs introduction, their economic sustainability, and feasibility, as well as the potentialities in process improvement.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Surgical practice has undergone major refinements with corresponding improvements in post-operative outcomes over the years. Standard monopolar and bipolar energy devices are currently widely used due to their inexpensive nature and reusability.
In the attempt to have better performance in the surgical practice, such as better vessel sealing, coagulation, and transection as well as an efficient tissue dissection, technological solutions such as energy devices are some of the important innovations that have contributed to these improvements. Since the nineties, more and more operations have become feasible by means of the so-called “key-hole surgery.” The attempt of being less invasive has gone together with the difficulties of doing the same dissections and gestures typical of open surgery through an indirect approach to the viscera. This has typically regarded hemostasis, as putting clamps or sutures was more difficult in laparoscopic surgery. Thus, the introduction of vessel-sealing devices has given an important incentive to minimal invasiveness in surgery. Moreover they have contributed to an easier, teachable, and faster way of dissecting tissues, also in open surgery.
Based on this, in the last 30 years, surgeons have become progressively persuaded by the usefulness of the so-called “High-energy devices” (HEDs) in surgical practice, as alternative medical devices to standard monopolar or bipolar devices. This has become particularly evident together with the increasing rate of surgeries made by minimally invasive approaches [1].
Three different types of vessel-sealing devices have gained importance, starting with ultrasonic shears and electrothermal coagulation up to latest mixed ultrasound-radiofrequency instruments.
Scientific evidence, throughout the years, has ascertained the efficacy of HEDs in achieving a better dissection and hemostasis, faster operating times, safer procedures, and shorter hospitalizations if compared to traditional instruments like monopolar or bipolar scalpels, hooks, scissors, and forceps, including a Cochrane systematic review in 2011 concerning colectomies [2] and a rapid Health Technology Assessment (HTA) on ultrasonic devices conducted in Italy in 2014, endorsed by Ministry of Health [3].
However, HEDs are associated to a higher acquisition cost with respect to standard medical devices, thus, being responsible of a significant part of the entire cost of surgical procedure. Despite the above economic concern, the use of HEDs has become a standard, in most general surgical practices. A recent survey structured and promoted by the Italian Society of Endoscopic Surgery (SICE), demonstrated this widespread use [4]. However, today the choice to use HED or traditional monopolar or bipolar devices, is mainly based on the surgeon’s preferences [4].
Moving on from these premises, given the lack of a standardized use of such HEDs in the Italian clinical practice, the deep investigation of the impacts of their higher implementation in surgery, is strictly required by means of a Health Technology Assessment (HTA) approach comparing HEDs with traditional medical devices currently used.
As for any new technology, the deep analysis of efficacy and safety issues, economic, ethical, social, legal, and organizational dimensions could support physicians and health providers in the decision making, by combining evidence-based results of multiple systematic reviews with a multimodal evaluation, also comprehending quantitative analysis to demonstrate both the economic and organizational sustainability in the standardized use of HEDs within different surgical settings [5, 6].
For the coverage of such knowledge gap, the SICE—Italian Society of Endoscopic Surgery—(affiliated with the EAES—European Association for Endoscopic Surgery) directory created a multi-disciplinary team (composed of surgeons selected by SICE, HTA experts, and healthcare sector researchers from Carlo Cattaneo—LIUC University, managerial engineers from Milan Politecnico and the AIIC—Italian Association of Clinical Engineers—methodology experts and statisticians from Mario Negri Institute of Research), with the aim to produce a scientific report, based on an HTA approach and trying to provide an answer to the following policy question: “Which are the main advantages, with reference to different domains typical of HTA evaluation, in adopting high-energy devices in comparison to the standard surgical equipment (bipolar and monopolar devices), for hospitals and patients?”
Methods
For the achievement of the above research activity objective, a Health Technology Assessment (HTA) analysis, grounded on the EUnetHTA Core Model was conducted, thus, being the reference framework useful to bring together evidence and other relevant and reliable information for hospital managers to guide good investment decisions [7]. IRB approval and written consent were not needed.
The HTA assumed the hospital point of view, with the aim to defining the different advantages regarding the use of HEDs (with respect to standard monopolar or bipolar devices) within the following eleven surgical settings: appendectomy, hepatic resections, colorectal resections, cholecystectomy, splenectomy, hemorrhoidectomy, thyroidectomy, esophago-gastrectomy, breast surgery, adrenalectomy, and pancreatectomy.
As suggested by the EUnetHTA Core Model and due to the multi-dimensional and multi-disciplinary nature of an HTA, several aspects were deeply analyzed: (1) health problems, in terms of definition of number of eligible patients undergoing a surgical procedure within the above-mentioned eleven settings, according to a 12-month time horizon; (2) description of the investigated technologies, by analyzing their technical characteristics; (3) safety aspects, in terms of potential development of any surgical complications or adverse events; (4) efficacy aspects, in terms of capability of the technology to reduce the operating time; (5) economic and financial dimension, for understanding the impact of the technologies on the hospital internal processes, as well as their economic sustainability and affordability; (6) organizational impact, thus, defining both the organizational investments with regard to the innovative technologies introduction (in terms of meetings, learning curve, and training), as well as the healthcare professional intention to use HEDs; (7) social aspects, evaluating potential advantages for the patients’ clinical pathway, thus, also quantifying their productivity loss related to the surgery; (8) equity impact, in terms of accessibility to the new technologies in specific hospitals’ context and the definition of the potential capabilities of hospitals to take in charge a higher number of patients; and (9) legal aspects, thus, definition potential normative or laws that may obstacle HEDs adoption in the clinical practice.
For the deployment of the above HTA dimensions, a multi-method approach was used [8, 9]. In particular, the above dimensions were assessed, by means of a literature review for the collection of comparative advantages, health-economics tools that are useful for the economic assessment of the patients’ clinical pathway undergoing surgery with HEDs or standard medical devices, and for conducting budget impact analyses, as well as for evaluating the organizational and accessibility advantages, in terms of time or procedures savings. Furthermore, a qualitative questionnaire was also developed and administered to surgeons to retrieve their perceptions, concerning HEDs’ utilization.
According to the above methodological approach, efficacy and safety issues were evaluated with 11 different systematic reviews of the existing literature and outcomes following Cochrane methods for conducting reviews [10]. Metanalyses were conducted whenever possible (by outcome and when at least 2 RCTs were eligible). The research questions were turned in search for major scientific databases with specific attention on population, intervention, control, and outcomes (PICO) [11] and run-on PubMed, Embase, Cochrane Library. For each surgical setting, details of search questions, PICOs, the whole screening process, and reasons for exclusion are reported in Appendix.
Titles and abstracts were screened by two independent surgeons with potential doubts solved by a consensus, and one methodologist when needed. Screening process was reported according to the PRISMA flow-chart model [12]. Quality of observational studies was assessed with Newcastle–Ottawa Scale (NOS) [13]. Risk of bias assessment for RCTs and forest plots were made with the Cochrane methodology and tools [10]. Primary outcomes were operating time (considered as an indirect driver of efficacy), bleeding, and intra-operative and post-operative complications (including surgical site infections—SSIs—and fistulas). Secondary outcomes were length of stay (LOS), established as time to discharge from operation, quality of life (including patients’ reported outcomes), costs (when available), pre-operative restraints (depending on the investigated setting), and exposition to surgical smoke (considered as a safety item for the operators, especially important in pandemic COVID times). Other outcomes were considered, stratified in reason of the surgical setting analyzed.
The economic dimension was deployed with an activity-based costing analysis [14] and a budget impact analysis [15], both assuming the hospital perspective, within a 12-month time horizon. At first, the patients’ clinical pathway was economically valorized, considering the eleven settings, concerning the use of either HEDs or standard medical devices. The following hospital costs, representing the input data of the economic evaluation, were considered: (1) human resources involved; (2) laboratory and radiologic exams, performed before and after the surgical procedure, in accordance with the length of stay; (3) disposable devices for patients’ and healthcare professionals working in the operating room; (4) instruments’ kits; (5) medical devices used (HED or standard devices); and (6) drugs and any other medications administered to patients during surgery or hospitalization. Only direct costs were accordingly investigated, and the total cost for each patient was calculated by multiplying the quantity of resources consumed by their unit cost. In addition, general and fixed hospital costs were integrated, consisting of all those costs different from labor factors, consumables, and equipment usage, being necessary to taking in charge patients because they provide the logistic and infrastructure support, in the measure of 20% of direct costs [16].
In the definition of the two different clinical pathways, within the eleven surgical settings, the main drivers for differential costs have been stated in the reduction of both the operating room occupation and the overall hospital stay.
Once having defined the costs per patient, with the inclusion of the potential adverse events and complications management that may occur after surgery, a budget impact analysis was implemented to verify the financial sustainability of HEDs higher and standardized use within the investigated eleven surgical settings. In particular, the baseline scenario (AS IS Scenario) where surgeries were performed according to the current HEDs or standard devices implementations was compared to two different innovative scenarios (TO BE Scenario): (1) Innovative Scenario 1, where a higher use of HEDs were assumed, according to experts’ opinions; (2) Innovative Scenario 2, where a complete replacement rate was assumed, in terms of HEDs use for all the eligible patients requiring surgery (i.e., Best-case Scenario). Table 1 depicts the specific market shares implemented concerning the presence or absence of HED’s utilization, within the eleven surgical settings.
Furthermore, a qualitative questionnaire was administered to 23 junior and senior surgeons to examine their perceptions on equity, social, legal, and organizational aspects, considering a comparative approach of HED and standard devices, in accordance with a 7-item Likert scale, ranging from − 3 to + 3 [17] and based on the specific items derived from EUnetHTA Core Model [6]. The above qualitative method was useful to collect a wide range of ideas and opinions that individuals carry out about issues and topics, as well as divulge viewpoint differences among stakeholders’ groups [18, 19]. In fact, for under discovered research areas, qualitative methods attempt to fill in gaps that are left unexposed by survey-based research, as well as literature evidence [20]. Based on the collections of healthcare professionals’ perceptions, all the dimensions were accordingly assessed, thus, giving important and comprehensive information, concerning multiple aspects of innovative medical technologies to be adopted in clinical practice.
In conclusion, the assessment of the above dimensions was integrated with a prioritization phase and a multi-criteria decision analysis [21], thus, simulating the technological appraisal phase and defining the technology presenting a higher added value for hospitals.
Focusing on statistical methods, economic and perceptions’ data were first analyzed, considering descriptive statistics. Differences among technologies (standard monopolars/bipolars and HEDs) were evaluated, according to a significance level lower than 0.05 (p value), thus, using the Independent Sample T test, after having verified the normality nature of the different variables.
All the analyses were performed using the Statistical Package for Social Science of IBM SPSS (Version 22).
Results
Results from the HTA dimensions’ assessment
Health problem relevance in the different settings
As previously mentioned, the analysis considered the possibility to optimize HEDs utilization in the following eleven surgical settings: appendectomy, hepatic resections, colorectal resections, cholecystectomy, splenectomy, hemorrhoidectomy, thyroidectomy, esophago-gastrectomy, breast surgery, adrenalectomy, and pancreatectomy. The definition of the target population requiring a surgery, and thus ,potentially eligible to HEDs use, derived from the Italian “SDO Report” for the year 2019 [22], indicating the conduction of 178,619 surgeries within a 12-month time horizon considering the above-mentioned settings.
Table 2 detailed the rate of different operations inside each setting that was set concerning the case-mix of the questioned pool of surgeons (range from maximum to minimum coming from different realities of the Italian national health system) integrated and mixed with data coming from the Italian “SDO Report” (2019 DRG national reports).
The hypothesis under the HTA analysis proposed, considered that all the hospitals could conduct surgical procedures in all the above-mentioned eleven settings.
Technologies under assessment comparison
Several high-energy vessel-sealing systems have been introduced in the Italian market in the past years. All instruments need a dedicated external generator to provide electrical power and allow settings of functional parameters. Ultrasonic devices are based on mechanical ultrasonic vibrations produced by a high-frequency vibrating stem paired with an articulated inert plier; such devices allow coagulation and cutting of vessels usually up to 7 mm in diameter, with documented minimal lateral thermal damage. Radiofrequency units use high-frequency electrical current to generate the thermic effect responsible of tissue denaturation and consequent vessel sealing. Such systems need a subsequent mechanical action—usually via a manually activated blade—to cut in between the previously sealed tissue. Some forceps available in the market and used in radiofrequency sealing, provide cutting via an automated movement of the blade, although none uses radiofrequency to fulfill the cutting phase. There are also so-called combined systems which couple ultrasonic and radiofrequency energies in the same instrument.
Different dimensions and lengths of the forceps are used either for laparoscopic or open surgery, and most of the devices are for single patients’ use. Some reusable radiofrequency HEDs are available on the market, and they can be reprocessed for a limited number of times. Among these, only few are equipped with the cutting mechanism. In most cases the generator is loaned for use, while single-use handpieces are subject to specific acquisition contracts. An evaluation of differences in performance, safety, general characteristics, and maintenance services are summarized in Table 3.
Evidence from the systematic literature review: efficacy and safety profiles
-
Appendectomy: The initial literature search revealed a total of 484 records, and one study fully matched the aim of this systematic review and was included in qualitative synthesis [23]. The retrospective cohort study was conducted on 1178 patients in a military hospital (460 treated with Endo Clip, 372 with Harmonic Scalpel—HS–, and 346 with the monopolar device). The three different groups did not report any differences in terms of age, gender, and body max index (BMI). As for primary outcomes, Lee and colleagues analyzed operating time and complications [23]; whereas, for secondary outcomes analyzed time of discharge, conversion to open surgery, and costs, no results regarding exposition to smoke nor quality of life were reported. A reduction of the operating time (OT) emerged in patients treated with Harmonic Scalpel compared to monopolar device. No significant differences in other primary and secondary outcomes have been reported, apart from costs, which were higher for HS. According to the NOS scale, the quality of the study was low mainly because it was conducted in a military hospital, so that the main biases were the selection of patients, the assessment of the outcome (the study was not blinded), and the length of follow-up (discharge time, short follow-up).
-
Colorectal surgery: The initial literature search revealed a total of 209 records identified through database searching, but only 7 studies fully matched the aim of this systematic review and were included in the final sample and relative analysis. Out of the 7 included studies, 4 were RCTs, and it was possible to perform quantitative synthesis [24,25,26,27]; the other 3 records were observational, two retrospective, and one prospective study [28,29,30]. In general terms, HEDs do not add substantial advantages in comparison to traditional energy devices in terms of primary (operative time, intra- and post-operation complications, intra-operatory blood loss) or secondary outcomes (time to discharge, conversion to open surgery). All RCTs and non-RCTs, except for Hubner et al. [24], analyzed the operation time and time of discharge. All the included studies, except for Scabini et al. [29], had intra-operative blood loss and post-operative complications as outcomes, while only Morino et al., Targarona et al., and Allaix et al. evaluated the intra-operative complications [25, 26, 28]. The RCTs of Hubner et al. and Targarona et al. were the only two that analyzed the costs of the different devices [24, 26]. Morino et al., Targarona et al., and Allaix et al. were the only three studies that evaluated the conversion from laparoscopic to open surgery [25, 26, 28]. According to the RCTs risk of bias (RoB), all the included RCTs were unclear for performance and detection biases, while 75% of them were at low risk for allocation concealment, attrition, and reporting biases; none of them had high risk of bias. These results, along with the absence of report analyzing the relevant clinical outcomes, such as quality of life and surgical smoke, do not allow to declare HED utilization as gold standard in colorectal surgery.
-
Cholecystectomy: The initial literature search revealed a total of 252 records identified through database searching. 19 papers corresponding to 18 studies fully matched the aim of this systematic review and were included in the final sample. Of the 18 included studies, 5 were observational, two retrospective and three prospective study [31,32,33,34,35], 11 were RCTs, and it was possible to perform quantitative synthesis [36,37,38,39,40,41,42,43,44,45,46]; only one was a systematic review [47]. Some of the included studies highlighted the substantial advantages of HEDs in comparison to traditional energy devices, in terms of operative time and blood loss, or the secondary outcome time to discharge. All the included studies (RCTs and non-RCTs) assessed the operative time outcome and reported significant differences in favor of the HED against monopolar or bipolar devices. Maybe the shorter HED operative time and the reduced exposition to pneumoperitoneo, lead to a shorter post-operatory pain, VAS score, nausea, and vomiting. Only three RCTs [37, 41, 47] and two non-RCTs [31, 35] analyzed blood loss and all these studies agreed on the HEDs superiority compared to monopolar and bipolar devices. Nevertheless, none of the patients treated in these studies, except for Kandil et al. [35], required a blood transfusion. 7 RCTs [36,37,38, 41, 43, 45, 46] and 2 non-RCTs [32, 34] reported a reduction in terms of time to discharge when patients were treated with HEDs; however, this reduction was not statistically meaningful, except for Tempe et al. [45]. No relevant difference has been found in the analysis of intra- and post-operative complications, even then not always fully described. Considering economic outcome, only Tempé et al. [45] found a cost advantage in using HED due to a difference in hospital stay, not confirmed in other studies. No significant difference has been found on conversion to open surgery. Data on post-operative pain (regarding quality of life) were reported by single RCTs, proving a significant reduction in pain perceiving when using HEDs, an effect which ends after 48 h. No information was reported in regard of surgical smokes and pre-operative restrains. According to the RCTs RoB, only four RCTs were evaluate as at low risk of bias [36, 39, 41, 47]. High risk of bias has been encountered in the random sequence generation and blinding (both performance and detection).
-
Haemorrhoidectomy: The initial literature search revealed a total of 66 records identified through database searching, 6 studies fully matched the aim of this systematic review and were included in the final sample and relative analysis. Of them 4 were RCTs [48,49,50,51] eligible for qualitative and quantitative analysis, and 2 were systematic reviews [52, 53]. Results of all the primary outcomes (post-operative pain, blood loss, operative time, and intra- and post- operative complication) analyzed by the 4 RCTs demonstrated superiority of the HEDs on monopolar or bipolar devices. Two RCTs were at a low risk of bias in two of the four RCTs [48, 51] and a high risk of bias in the other two RCTs [49, 50].
-
Liver resections: The initial literature search revealed a total of 504 records identified through database searching, 7 studies fully matched the aim of this systematic review and were included in the final sample and relative analysis. Of them, 5 were observational studies (2 prospective and 3 retrospective) [54,55,56,57,58] and 2 RCTs [59, 60]. All the primary outcomes (blood loss, operative time, and intra- and post-operative complication) analyzed by the RCTs were in favor of the HEDs compared to crush clamping. All the included studies, both RCTs and non-RCTs, reported a significant risk reduction in terms of blood loss (during transection) and biliary fistulas. Both the RCTs, plus the observational study Sakomato et al., found that transection time and speed of transection were shorter when patients were treated with HEDs [54, 59, 60]. The observational studies from Galizia et al., Guo and Li, found that operative time was shorter when using the HEDs compared to crush clamping [55, 56, 58]. In regards of the secondary outcomes, no significant differences have been reported in terms of length of stay (LOS) and surgical site infections (SSIs). Data coming from the two RCTs confirmed a significant lowering of complications (biliary fistula). Also, no significant differences have been found concerning SSIs and post-operative blood loss. Both primary and secondary outcomes were analyzed for partial transections and major transections. Moreover, a potential bias of the two RCTs, is the heterogeneity in the treatment, with regards specifically the vessel diameter (Ichida et al. < 2 mm vs. Gotohda < 5 mm) [59, 60]. Nevertheless, HED technology seems to be superior also when applied on vessels with bigger diameter. According to The Newcastle–Ottawa Scale (NOS), all the observational studies had a high risk of bias in terms of exposure category, and a low risk of bias for the other categories.
-
Splenectomy: The initial literature search revealed a total of 136 records identified through database searching, 3 RCTs [61,62,63] all comparing radiofrequency devices versus standard coagulation fully matched the aim of this systematic review and were included in the final sample and relative analysis. The primary outcome (referring to post-operative complications) was evaluated by all the three included RCTs, while operative time and intra-operative blood losses were evaluated by Shabaahang et al. and Amirkazem et al. [61, 62]. Data from the metanalyses of the three studies show a significant reduction in OT and intra-operative bleeding, while no significance has been found regarding post-operative complications. Only one study [63] evaluates post-operative pain with a VAS scale, and LOS finding no differences for both secondary outcomes. A low risk of bias emerged for all the evaluated items, considering evidence reported by Amirkazem et al. and Yao et al. [62, 63]. On the contrary, Shabaahang et al. revealed a high risk of bias for “blinding outcome assessment” and an unclear risk for all the other categories [61].
-
Pancreatic resection: The initial literature search revealed a total of 135 records identified through database searching, 1 RCT [64] and 2 observational studies [65, 66] fully matched the aim of this systematic review and were included in the final sample and relative analysis. All the three studies analyzed the primary outcomes bleeding, operative time, and post-operative complications, as well as for the time of discharge and intra-operative blood loss secondary outcomes. The RCT [64] and the observational study of Wu et al. [66] also evaluated the occurrence of post-operative pancreatic fistula and costs. The three studies reported that the use of HEDs do not significantly change pancreatic surgery pre-operatory outcomes, which appears to be equivalent to the outcomes obtained with conventional techniques. The three studies had a low risk of bias.
-
Thyroidectomy: The initial literature search revealed a total of 250 records identified through database searching, 20 RCTs [67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86] and 17 observational studies [87,88,89,90,91,92,93,94,95,96,97,98,99,100,101] fully matched the aim of this systematic review and were included in the final sample and relative analysis. As for efficacy parameters, 20/20 RCTs and 15/17 observational (8 prospective and 7 retrospective) studies analyzed operative time, and all agreed upon a reduction in surgical time when using HEDs. Only the observational study of Cipolla et al., did not highlight any difference in reducing operative time while using HED [90]. A meta-analysis confirmed a significant reduction of operative time. 10/20 RCTs and 14/17 observational studies (7 prospective and 7 retrospective) evaluated intra-operative bleeding which was significantly reduced in patients treated with HEDs. The RCTs of Koh et al. [70], the observational studies Cipolla et al. [90] and Kuboki et al. [94] not highlighted any difference in reducing intra-operative bleedings while using HEDs. For secondary outcomes, length of hospital stays and costs, were the two parameters analyzed in the included studies. From the evaluation of the length of stay in 13/20 RCT and 13/17 observational studies (7 prospective and 6 retrospective), only in 3 RCTs was found a reduction of this outcome, the other studies did not highlight any clear impact while using HEDs. On the contrary, all the observational studies have experienced a significant reduction in the length of hospital stay. Costs were, differently from other settings, well studied in 25 studies, and, even if data were not comparable, all evidenced an increase in cost due to HEDs.
-
Breast surgery: The initial literature search revealed a total of 184 records identified through database searching, 24 RCTs [102,103,104,105,106,107,108,109,110,111,112,113,114,115,116,117,118,119,120,121,122,123,124,125] fully matched the aim of this systematic review and were included in the final sample and relative analysis. All the included RCTs reported the primary outcomes of operative time, blood loss and intra- and post-operatory complications. Three studies highlighted a statistically significant reduction in terms of operative time, using HEDs [105, 106, 119], while the other 15 studies, focused on the use of HEDs during mastectomy, highlighted a modest reduction in terms of operative time. 12/24 RCTs reported a statistically significant reduction of intra-operative bleeding using HEDs. All the included studies reported a moderate reduction of intra- and post-operative complications following the use of HEDs. All the 24 included RCTs reported information regarding the secondary outcomes of length of hospital stay, post-operative pain and their effects on the quality of life finding no statistically significant differences while using HEDs. None of the included studies reported information in terms of surgical smokes and costs. Kontos et al. was the only study reporting some information on HEDs costs, but cost analysis was done in 2008 when HEDs diffusion in the market was still low [114].
-
Adrenalectomy: The initial literature search revealed a total of 100 records identified through database searching, only 2 observational retrospective studies [126, 127] fully matched the aim of the review and were included in the final sample and relative analysis. Both studies regarded laparoscopic adrenalectomy. Overall, the two studies included 256 patients (165 in one study and 91 in the second one), of them 100 patients in the HED group and 156 in the monopolar/bipolar group. Significant differences were confirmed in both studies regarding a lower OT with HEDs. No statistical differences were noticed in conversions to laparotomy, complications or bleedings. One study evidenced that, in terms of costs, the use of HEDs was cost saving (70–105$) as there was a reduced use of vascular clips [126]. All observational studies were at low risk of bias for all items assessed.
Economic and financial dimension
Table 4 reports the cost per patient related to the clinical pathway performed in the different eleven surgical settings, valorized based on the use of standard monopolar/bipolar devices, or HEDs, and considering the development of adverse events and complications. An economic advantage per patients is reported in most surgical settings, with the solely exception of cholecystectomy, colorectal and esophago-gastric surgeries, where a slight investment emerged. In the comparison between the weighted average costs, considering the different case-mix, the use of HEDs is related to an overall modification of cost per patients ranging from + 0.81 to − 3.14%.
In addition, a budget impact analysis (BIA) was implemented to define HEDs economic affordability and sustainability in the clinical practice. Given the economic evaluation previously mentioned, as well as the different scenarios under assessment, HEDs introduction would lead to a marginal investment ranging from + 0.43% to + 0.78%, with the possibility to report a higher economic saving if surgeries are performed in accordance with the distribution rate from the Italian “SDO Report” (2019) [22], for the conduction of 178,619 surgeries within a 12-month time horizon (Table 5).
Organizational dimension
From an organizational point of view, as for the economic dimension deployment, literature declared a decrease in both OT and LOS in using HED within specific surgical settings.
According to 178,619 surgeries, and assuming the same scenarios as the BIA, Table 6 reports that HEDs would generate significant organizational savings, ranging from a minimum of 5.25% and a maximum of 9.02% in terms of release of operating room time. Based on the above an advantage in accessibility to surgery can be hypothesized in a 9% of increase, due to the gaining in operatory slots derived from the implementation of new technologies.
The same trend emerged considering the improvement of the overall LOS: a standardized use of HEDs would lead to a decrease in LOS, ranging from a minimum of 5.03% to a maximum of 30.73%.
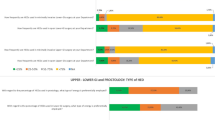
Results from the qualitative assessment
The analysis of the qualitative perceptions of the healthcare professionals involved (Table 7) (considering a 7-item Likert Scale, ranging from − 3 to + 3), reported no differences between traditional devices and HEDs, from an equity perspective (0.41 vs. 0.55, p value > 0.05). A negative impact emerged considering HED’s accessibility (0.43 vs. 1.57, p value = 0.011), since their acquisition is not yet standardized, given the problem in the diffusion of HEDs, particularly between hub and spoke hospitals. However, these innovative devices could enhance the overall access to care given a potential clinical pathway optimization, due to an improvement in both the adverse events management (0.65 vs. − 0.04, p value = 0.007) and in the operating room occupancy time (0.91 vs. 0.09, p value = 0.012). In assuming the patients’ point of view, the surgeons reported a preference for HEDs in comparison with traditional monopolar and bipolar devices (0.70 vs. 0.20, p value = 0.048). The introduction of the HEDs would improve patients’ quality of life (1.17 vs. 0.35, p value = 0.005) and satisfaction (1.09 vs. 0.22, p value = 0.002), thus, being strictly related to a faster recovery time (1.13 vs. 0.30, p value = 0.005) and a better post-operative condition (1.22 vs. 0.26, p value = 0.001).
An analysis of the legal implications reported that the two technologies under assessment could be considered super-imposable in their measurement (p value > 0.05), even if additional legal efforts are required regarding the regulation of HEDs acquisition.
Focusing on the organizational dimension, no significant differences have been evidenced for the organizational point of view between the technologies being assessed (p value = 0.068), even if in a short-term time-horizon training courses are required when introducing HEDs, devoted to both surgeons and nurses. On the other hand, professionals’ perceptions crystallized that HEDs could optimize the length of stay (p value < 0.05), timing of operations (p value < 0.05), and consequently occupation of the operating theaters. Reduction of morbidity could improve the overall organizational clinical pathway, in terms of hospital management of a patient requiring a specific surgery (p value = 0.006). The reduction of the operating times might have the consequence, in the opinion of surgeons, of freeing spaces and reducing the waiting lists.
Results from the appraisal phase
The final phase of the analysis required the implementation of a multi-criteria decision approach (MCDA), to define a final score, useful for an evidence-based policy-making appraisal [10].
In determining which aspect of the HTA dimensions was more important, all the surgeons tended to perceive safety and efficacy, followed by technical relevance and economic impacts as the most relevant. Junior surgeons are more prone to consider economical and legal issues important, while seniors agree on technical relevance and organizational impact to be more significant.
Results from the MCDA (Table 8) revealed that HEDs could represent the preferable medical devices to be used during surgery, having acquired a higher score than the comparator (0.51 vs. 0.43), when available in the clinical practice.
Discussion and conclusions
The results of the study generate an interesting scientific contribution, thus, covering an important knowledge gap, regarding the use of HEDs, within specific surgical settings, suggesting their consolidated use in the clinical practice.
In this full HTA report, both the assessment and the appraisal phases have confirmed that the introduction of HEDs in surgery is a valid alternative to standard monopolar and bipolar instruments in general surgical practice. Evidence-based information has proved a higher efficacy and safety of HEDs, even if this superiority is not to be extended to all the surgical procedures and settings. In this view, due to the lack of standardized suggestions and the related difficulties to have informed decision about merits of any energy devices. In fact, the efficiency of any energy source depends on seal time, lateral thermal spread, burst pressure, and smoke production.
However, from an economic perspective, the introduction of HEDs can lower the overall process costs, by freeing up economical and organizational resources for the hospital, thus, representing a sustainable choice of overall improvement and optimization of resources. This can potentially reduce the waiting lists which remain a critical item, especially during the current COVID-19 pandemic. This is strictly dependent from the organizational setting of each hospital, particularly its case-mix, and the organizational capability of the system, or its ability to take advantages of freed resources. Relevant advantages emerged in considering the patients’ and the society point of view, in terms of reduction of productivity losses due to hospital stay, with important out-of-pocket expenditure savings ranging from a minimum of 4.74% to a maximum of 10.71%. On the other hand, surgeons’ point of view suggests initially to re-invest these resources in training healthcare professionals to maximize the advantages of the new technology by using it properly.
The present paper presents two main limitations. On the one hand, this HTA has the defect of having analyzed the perception of this specific and highly technical item only through questionnaires targeted on surgeons and technology experts. It would be interesting to test the perception of such a diffuse technology also in other figures of the healthcare system, like associations of patients, healthcare providers, and managers, to strengthen the validity of the results. On the other hand, the analysis did not consider the use of HEDs within robotic surgery, thus, opening a further development of study. The reason why robotic surgery was not taken into account relies on the fact that, as described in other evidence, robotics is not fully recognized and utilized in all the surgical settings under assessment, at least in the Italian setting [128]. This is why the attention was focused on minimally invasive and open surgeries. Also, nowadays, the introduction and development of different robotic platforms, not all of them, at present, with a standardized HED included, makes the analysis too difficult due to the high confounding biases.
In conclusion, the routine use of HEDs can be considered proper and sustainable, in a balance between costs and outcomes, suggesting a responsible use of such innovative devices, thus, improving surgical outcomes and guarantying, at the same time, cost savings and patients’ satisfaction.
References
Pucher PH, Mackenzie H, Tucker V, Mercer SJ (2021) A national propensity score-matched analysis of emergency laparoscopic versus open abdominal surgery. Br J Surg 108:934–940
Tou S, Malik AI, Wexner SD, Nelson RL (2011) Energy source instruments for laparoscopic colectomy. Cochrane Datab Syst Rev 5:1
Migliore A, Corio M, Perrini MR, Rivoiro C, Jefferson T (2014) Ultrasonic energy devices for surgery: rapid HTA report. Agenas, Agenzia Nazionale Per i Servizi Sanitari Regionali
Botteri E, Podda M, Arezzo A, Vettoretto N, Sartori A, Agrusa A, Allaix ME, Anania G, Brachet Contul R, Caracino V, Cassinotti E, Cuccurullo D, D’Ambrosio G, Milone M, Muttillo I, Petz WL, Pisano M, Guerrieri M, Silecchia G, Agresta F (2021) Current status on the adoption of high energy devices in Italy: an Italian Society for Endoscopic Surgery and New Technologies (SICE) national survey. Surg Endosc 35:6201–6211
EuroScan International Network (2014) A toolkit for the identification and assessment of new and emerging health technologies. EuroScan International Network
European Network for Health Technology Assessment (EUnetHTA) (2016) The HTA core model, version 2.13.0
Sampietro-Colom L, Lach K, Pasternack I, Wasserfallen JB, Cicchetti A, Marchetti M, Kidholm K, Arentz-Hansen H, Rosenmöller M, Wild C, Kahveci R (2015) Guiding principles for good practices in hospital-based health technology assessment units. Int J Technol Assess Health Care 31:457–465
Creswell JW (2015) A concise introduction to mixed methods research. Sage, Thousand Oaks
O’ Cathain A, Murphy E, Nicholl J, (2008) The quality of mixed methods studies in health services research. J Health Serv Res Policy 13:92–98
Higgins JPT, Green S (2008) Cochrane handbook for systematic reviews of interventions. Wiley, New York
Schardt C, Adams MB, Owens T, Keitz S, Fontelo P (2007) Utilization of the PICO framework to improve searching PubMed for clinical questions. BMC Med Inform Decis Mak 7:16
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol 62:e1–e34
Stang A (2010) Critical evaluation of the Newcastle–Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol 25:603–605
Bruggeman W, Everaert P (2009) Time-driven activity-based costing: exploring the underlying model. Cost Manag 21:16–20
Mauskopf JA, Sullivan SD, Annemans L, Caro J, Mullins CD, Nuijten M, Orlewska E, Watkins J, Trueman P (2007) Principles of good practice for budget impact analysis: report of the ISPOR task force on good research practices-budget impact analysis. Value Health 10:336–347
Adduce A, Lorenzoni L (2004) Metodologia e primi risultati di un’indagine ministeriale sui costi delle prestazioni di ricovero ospedaliero. Politiche Sanitarie 5:158–172
Mitton C, Dionne F, Damji R, Campbell D, Bryan S (2011) Difficult decisions in times of constraint: criteria based resource allocation in the vancouver coastal health authority. BMC Health Serv Res 11:169
Kitzinger J (1995) Qualitative research: introducing focus groups. BMJ 311:299–302
Berg B (2009) Qualitative research methods for the social sciences. Allyn & Bacon, New York, pp 101–157
Jansen H (2010) The logic of qualitative survey research and its position in the field of social research methods. Forum Qual Soc Res 11:1
Thokala P (2016) Multiple criteria decision analysis for health care decision making—an introduction, report 1 of the ISPOR MCDA emerging good practices task force. Value Health 19:1–13
Ministero Della Salute (2020) Rapporto annuale sull’attività di ricovero ospedaliero
Lee JS, Hong TH (2014) Comparison of various methods of mesoappendix dissection in laparoscopic appendectomy. J Laparoendosc Adv Surg Tech A 24:28–31
Hubner M, Demartines N, Muller S, Dindo D, Clavien PA, Hahnloser D (2008) Prospective randomized study of monopolar scissors, bipolar vessel sealer and ultrasonic shears in laparoscopic colorectal surgery. Br J Surg 95:1098–1104
Morino M, Rimonda R, Allaix ME, Giraudo G, Garrone C (2005) Ultrasonic versus standard electric dissection in laparoscopic colorectal surgery: a prospective randomized clinical trial. Ann Surg 242:897–901
Targarona EM, Balague C, Marin J, Neto RB, Martinez C, Garriga J, Trias M (2005) Energy sources for laparoscopic colectomy: a prospective randomized comparison of conventional electrosurgery, bipolar computer-controlled electrosurgery and ultrasonic dissection. Operative outcome and costs analysis. Surg Innov 12:339–344
Zhou BJ, Song WQ, Yan QH, Cai JH, Wang FA, Liu J, Zhang GJ, Duan GQ, Zhang ZX (2008) Ultrasonically activated scalpel versus monopolar electrocautery shovel in laparoscopic total mesorectal excision for rectal cancer. World J Gastroenterol 14:4065–4069
Allaix ME, Furnée EJ, Arezzo A, Mistrangelo M, Morino M (2016) Energy sources for laparoscopic colorectal surgery: Is one better than the others? J Laparoendosc Adv Surg Tech A 26:264–269
Scabini S, Rimini E, Romairone E, Scordamaglia R, Boaretto R, Pertile D, Ferrando V (2008) Total mesorectal excision with radiofrequency in rectal cancer. Minerva Chir 63:289–292
Cui R, Yu MH, Chen JJ, Qin J, Yue B, Luo Y, Huang YZ, Zhou H, Zhong M (2019) Monopolar electrosurgical scissors versus harmonic scalpel in robotic anterior resection of rectal cancer: a retrospective cohort study. J Laparoendosc Adv Surg Tech A 29:880–885
Zanghì A, Cavallaro A, Di Mattia P, Di Vita M, Cardì F, Piccolo G, Barbera G, Fisichella R, Spartà D, Cappellani A (2014) Laparoscopic cholecystectomy: ultrasonic energy versus monopolar electrosurgical energy. Eur Rev Med Pharmacol Sci 18:54–59
Gelmini R, Franzoni C, Zona S, Andreotti A, Saviano M (2010) Laparoscopic cholecystectomy with harmonic scalpel. JSLS 14:14–19
Bulus H, Basar O, Tas A, Yavuz A, Akkoca M, Coskun A, Coban S, Tuna Y, Erbis H, Koklu S (2013) Evaluation of three instruments for laparoscopic cholecystectomy: harmonic scalpel, bipolar vessel sealer, and conventional technique. Minerva Chir 68:537–542
Redwan AA (2010) Single-working-instrument, double-trocar, clipless cholecystectomy using harmonic scalpel: a feasible, safe, and less invasive technique. J Laparoendosc Adv Surg Tech A 20:597–603
Kandil T, El Nakeeb A, El Hefnawy E (2010) Comparative study between clipless laparoscopic cholecystectomy by harmonic scalpel versus conventional method: a prospective randomized study. J Gastrointest Surg 14:323–328
Cengiz Y, Dalenbäck J, Edlund G, Israelsson LA, Jänes A, Möller M, Thorell A (2010) Improved outcome after laparoscopic cholecystectomy with ultrasonic dissection: a randomized multicenter trial. Surg Endosc 24:624–630
El Nakeeb A, Askar W, El Lithy R, Farid M (2010) Clipless laparoscopic cholecystectomy using the harmonic scalpel for cirrhotic patients: a prospective randomized study. Surg Endosc 24:2536–2541
Jain SK, Tanwar R, Kaza RCM, Agarwal PN (2011) A prospective, randomized study of comparison of clipless cholecystectomy with conventional laparoscopic cholecystectomy. J Laparoendosc Adv Surg Tech A 21:203–208
Janssen IM, Swank DJ, Boonstra O, Knipscheer BC, Klinkenbijl JH, van Goor H (2003) Randomized clinical trial of ultrasonic versus electrocautery dissection of the gallbladder in laparoscopic cholecystectomy. Br J Surg 90:799–803
Mahabaleshwar V, Kaman L, Iqbal J, Singh R (2012) Monopolar electrocautery versus ultrasonic dissection of the gallbladder from the gallbladder bed in laparoscopic cholecystectomy: a randomized controlled trial. Can J Surg 55:307–311
Liao G, Wen S, Xie X, Wu Q (2016) Harmonic scalpel versus monopolar electrocauterization in cholecystectomy. JSLS 20:e2016.00037
Bessa SS, Al-Fayoumi TA, Katri KM, Awad AT (2008) Clipless laparoscopic cholecystectomy by ultrasonic dissection. J Laparoendosc Adv Surg Tech A 18:593–598
Wetter LA, Payne JH, Kirshenbaum G, Podoll EF, Bachinsky T, Way LW (1992) The ultrasonic dissector facilitates laparoscopic cholecystectomy. Arch Surg 127:1195–1198
Rajnish K, Sureshkumar S, Ali MS, Vijayakumaret C, Sudharsanan S, Palanivel C (2018) Harmonic scalpel-assisted laparoscopic cholecystectomy vs. conventional laparoscopic cholecystectomy—a non-randomized control trial. Cureus 10:e2084
Tempé F, Jänes A, Cengiz Y (2013) Cost analysis comparing ultrasonic fundus-first and conventional laparoscopic cholecystectomy using electrocautery. Surg Endosc 27:2856–2859
Cengiz Y, Jänes A, Grehn A, Israelsson LA (2005) Randomized trial of traditional dissection with electrocautery versus ultrasonic fundus-first dissection in patients undergoing laparoscopic cholecystectomy. Br J Surg 92:810–813
Catena F, Di Saverio S, Ansaloni L, Coccolini F, Sartelli M, Vallicelli C, Cucchi M, Tarasconi A, Catena R, De’ Angelis G, Abongwa HK, Lazzareschi D, Pinna A (2014) The HAC trial (harmonic for acute cholecystitis): a randomized, double-blind, controlled trial comparing the use of harmonic scalpel to monopolar diathermy for laparoscopic cholecystectomy in cases of acute cholecystitis. World J Emerg Surg 9(1):53
Sakr MF (2010) LigaSure versus Milligan–Morgan hemorrhoidectomy: a prospective randomized clinical trial. Tech Coloproctol 14:13–17
Abo-hashem AA, Sarhan A, Aly AM (2010) Harmonic Scalpel compared with bipolar electro-cautery hemorrhoidectomy: a randomized controlled trial. Int J Surg 8:243–247
Bulus H, Tas A, Coskun A, Kucukazman M (2014) Evaluation of two hemorrhoidectomy techniques: harmonic scalpel and Ferguson’s with electrocautery. Asian J Surg 37:20–23
Shahmoradi MK, Mehri J, Taheri HR (2020) Comparison of hemorrhoidectomy using harmonic scalpel and electrocautery: a randomized controlled trial. Int J Surg Open 27:39–42
Nienhuijs SW, de Hingh IH (2010) Pain after conventional versus Ligasure haemorrhoidectomy. A meta-analysis. Int J Surg 8:269–273
Milito G, Cadeddu F, Muzi MG, Nigro C, Farinon AM (2010) Haemorrhoidectomy with Ligasure vs. conventional excisional techniques: meta-analysis of randomized controlled trials. Colorectal Dis 12:85–93
Sakamoto Y, Yamamoto J, Kokudo N, Seki M, Kosuge T, Yamaguchi T, Muto T, Makuuchi M (2004) Bloodless liver resection using the monopolar floating ball plus ligasure diathermy: preliminary results of 16 liver resections. World J Surg 28:166–172
Galizia G, Castellano P, Pinto M, Zamboli A, Orditura M, De Vita F, Pignatelli C, Lieto E (2012) Radiofrequency-assisted liver resection with a comb-shaped bipolar device versus clamp crushing: a clinical study. Surg Innov 19:407–414
Guo JY, Li DW, Liao R, Huang P, Kong XB, Wang JM, Wang HL, Luo SQ, Yan X, Du CY (2014) Outcomes of simple saline-coupled bipolar electrocautery for hepatic resection. World J Gastroenterol 20:8638–8645
Nanashima A, Tobinaga S, Abo T, Nonaka T, Sawai T, Nagayasu T (2010) Usefulness of the combination procedure of crash clamping and vessel sealing for hepatic resection. J Surg Oncol 102:179–183
Li W, Jiang L, Zhou X, Liu L, Lu X, Wang S (2016) Application of a clamp method combined with bipolar coagulation for anatomical hepatectomy in the treatment of hepatic carcinoma. J BUON 21:645–649
Gotohda N, Yamanaka T, Saiura A, Uesaka K, Hashimoto M, Konishi M, Shimada K (2015) Impact of energy devices during liver parenchymal transection: a multicenter randomized controlled trial. World J Surg 39:1543–1549
Ichida A, Hasegawa K, Takayama T, Kudo H, Sakamoto Y, Yamazaki S, Midorikawa Y, Higaki T, Matsuyama Y, Kokudo N (2016) Randomized clinical trial comparing two vessel-sealing devices with crush clamping during liver transection. Br J Surg 103:1795–1803
Shabahang H, Maddah G, Tavassoli A, Jangjoo A, Alvandipour M, Abdollahi A, Noorshafiee S (2012) Laparoscopic splenectomy: Ligasure or clip ligation? Surg Laparosc Endosc Percutan Tech 22:136–138
Amirkazem VS, Malihe K (2017) Randomized clinical trial of ligasure™ versus conventional splenectomy for injured spleen in blunt abdominal trauma. Int J Surg 38:48–51
Yao HS, Wang WJ, Wang Q, Gao WC, Xiang HG, Hu ZQ, Gao JD, Chen XY, Wang WM (2011) Randomized clinical trial of vessel sealing system (LigaSure) in esophagogastric devascularization and splenectomy in patients with portal hypertension. Am J Surg 202:82–90
Uzunoglu FG, Stehr A, Fink JA, Vettorazzi E, Koenig A, Gawad KA, Vashist YK, Kutup A, Mann O, Gavazzi F, Zerbi A, Bassi C, Dervenis C, Montorsi M, Bockhorn M, Izbicki JR (2012) Ultrasonic dissection versus conventional dissection techniques in pancreatic surgery: a randomized multicentre study. Ann Surg 256:675–679
Matsumoto T, Ishio T, Sasaki A, Aramaki M, Bandoh T, Kawano K, Yoshida T, Kitano S (2002) Pancreatic resection with ultrasonically activated scalpel: preliminary observations. Hepatogastroenterology 49:635–638
Wu CH, Chen CH, Ho TW, Shih MC, Wu JM, Kuo TC, Yang CY, Tien YW (2021) Pancreatic neck transection using a harmonic scalpel increases risk of biochemical leak but not postoperative pancreatic fistula after pancreaticoduodenectomy. HPB (Oxford) 23:301–308
Sista F, Schietroma M, Ruscitti C, De Santis G, De Vita F, Carlei F, Amicucci G (2012) New ultrasonic dissector versus conventional hemostasis in thyroid surgery: a randomized prospective study. J Laparoendosc Adv Surg Tech A 22:220–224
Minni A, Rosati D, Cavaliere C, De Carlo A, Illuminati G, Scarano Catanzaro V, Bodoni M (2016) Study on the use of focus harmonic scalpel in thyroidectomies: Is it useful also in preserving voice function? Eur Rev Med Pharmacol Sci 20:3544–3551
Su L, Li J, Tang X, Sang J (2016) Therapeutic effects of bipolar coagulation forceps on open thyroid surgery. Rev Invest Clin 68:256–261
Koh YW, Park JH, Lee SW, Choi EC (2008) The harmonic scalpel technique without supplementary ligation in total thyroidectomy with central neck dissection: a prospective randomized study. Ann Surg 247:945–949
Kilic M, Keskek M, Ertan T, Yoldas O, Bilgin A, Koc M (2007) A prospective randomized trial comparing the harmonic scalpel with conventional knot tying in thyroidectomy. Adv Ther 24:632–638
Lombardi CP, Raffaelli M, Cicchetti A, Marchetti M, De Crea C, Di Bidino R, Oragano L, Bellantone R (2008) The use of “harmonic scalpel” versus “knot tying” for conventional “open” thyroidectomy: results of a prospective randomized study. Langenbecks Arch Surg 393:627–631
Witzel K, von Rahden BH, Stein HJ (2009) The effect of ultrasound dissection in thyroid surgery. Eur Surg Res 43:241–244
Basurto-Kuba EOP, Robles-Estrada M, Hurtado-López LM, Oca-Duran EDM, Campos-Castillo C, Zaldivar-Ramirez FR, Pulido-Cejudo A (2017) Safety and cost-effectiveness in thyroidectomy using the HARMONIC scalpel compared to traditional hemostasis: a controlled clinical assay. Surg Technol Int 30:141–147
Yildirim O, Umit T, Ebru M, Bulent U, Belma K, Betul B, Mete D, Omer C (2008) Ultrasonic harmonic scalpel in total thyroidectomies. Adv Ther 25:260–265
Duan YF, Xue W, Zhu F, Sun DL (2013) FOCUS harmonic scalpel compared to conventional hemostasis in open total thyroidectomy—a prospective randomized study. J Otolaryngol Head Neck Surg 42(1):62
Ferri E, Armato E, Spinato G, Spinato R (2011) Focus harmonic scalpel compared to conventional haemostasis in open total thyroidectomy: a prospective randomized trial. Int J Otolaryngol 2011:357195
Konturek A, Barczyński M, Stopa M, Nowak W (2012) Total thyroidectomy for non-toxic multinodular goiter with versus without the use of harmonic FOCUS dissecting shears—a prospective randomized study. Wideochir Inne Tech Maloinwazyjne 7:268–274
Papavramidis TS, Sapalidis K, Michalopoulos N, Triantafillopoulou K, Gkoutzamanis G, Kesisoglou I, Papavramidis ST (2010) UltraCision harmonic scalpel versus clamp-and-tie total thyroidectomy: a clinical trial. Head Neck 32:723–727
Miccoli P, Materazzi G, Miccoli M, Frustaci G, Fosso A, Berti P (2010) Evaluation of a new ultrasonic device in thyroid surgery: comparative randomized study. Am J Surg 199:736–740
Cordón C, Fajardo R, Ramírez J, Herrera MF (2005) A randomized, prospective, parallel group study comparing the harmonic scalpel to electrocautery in thyroidectomy. Surgery 137:337–341
Hallgrimsson P, Lovén L, Westerdahl J, Bergenfelz A (2008) Use of the harmonic scalpel versus conventional haemostatic techniques in patients with Grave disease undergoing total thyroidectomy: a prospective randomised controlled trial. Langenbecks Arch Surg 393:675–680
Cannizzaro MA, Lo Bianco S, Borzì L, Cavallaro A, Buffone A (2014) The use of FOCUS Harmonic scalpel compared to conventional haemostasis (knot and tie ligation) for thyroid surgery: a prospective randomized study. Springerplus 3:639
Mourad M, Rulli F, Robert A, Scholtes JL, De Meyer M, De Pauw L (2011) Randomized clinical trial on harmonic focus shears versus clamp-and-tie technique for total thyroidectomy. Am J Surg 202:168–174
Kowalski LP, Sanabria A, Vartanian JG, Lima RA, de Mendonca UB, dos Santos CR, Boldrini D Jr, de Mello LE, Pinto FP, Lehn CN, Correa LA, Dedivitis RA, Guimarães AV, Pedruzzi PA, Ramos GH, Gonçalves AJ, Suehara AB, Kanda JL, Capuzzo Rde C, de Oliveira JC, Curado MP, de Góis Filho JF, Fukuyama E, Beserra IM Jr, de Carvalho Neto PB, Carvalho AL (2012) Total thyroidectomy with ultrasonic scalpel: a multicenter, randomized controlled trial. Head Neck 34:805–812
Chavez KV, Barajas EM, Ramírez J, Pantoja JP, Sierra M, Velázquez-Fernandez D, Herrera MF (2017) Comparative analysis between a bipolar vessel sealing and cutting device and the tie and suture technique in thyroidectomy: a randomized clinical trial. Surgery 161:477–484
Bhettani MK, Rehman M, Khan MS, Altaf HN, Hakeem Khan K, Farooqui F, Amir M, Altaf OS (2019) Safety and cost-effectiveness of LigaSure® in total thyroidectomy in comparison with conventional suture tie technique. Cureus 11:e6368
Maeda H, Kutomi G, Satomi F, Shima H, Mori M, Takemasa I (2018) Comparison of surgical outcomes and complications between the harmonic FOCUS and conventional surgery for open thyroidectomy. Mol Clin Oncol 8:553–556
Al-Dhahiry JK, Hameed HM (2015) Total thyroidectomy: conventional suture ligation technique versus sutureless techniques using harmonic scalpel or maxium. Ann Med Surg (Lond) 5:29–34
Cipolla C, Graceffa G, Sandonato L, Fricano S, Vieni S, Latteri MA (2008) LigaSure in total thyroidectomy. Surg Today 38:495–498
Barbaros U, Erbil Y, Bozbora A, Deveci U, Aksakal N, Dinççağ A, Ozarmağan S (2006) The use of LigaSure in patients with hyperthyroidism. Langenbecks Arch Surg 391:575–579
Franko J, Kish KJ, Pezzi CM, Pak H, Kukora JS (2006) Safely increasing the efficiency of thyroidectomy using a new bipolar electrosealing device (LigaSure) versus conventional clamp-and-tie technique. Am Surg 72:132–136
Kirdak T, Korun N, Ozguc H (2005) Use of ligasure in thyroidectomy procedures: results of a prospective comparative study. World J Surg 29:771–774
Kuboki A, Nakayama T, Konno W, Goto K, Nakajima I, Kanaya H, Hirabayashi H, Haruna S (2013) New technique using an energy-based device versus conventional technique in open thyroidectomy. Auris Nasus Larynx 40:558–562
Petrakis IE, Kogerakis NE, Lasithiotakis KG, Vrachassotakis N, Chalkiadakis GE (2004) LigaSure versus clamp-and-tie thyroidectomy for benign nodular disease. Head Neck 26:903–909
Manouras A, Markogiannakis H, Koutras AS, Antonakis PT, Drimousis P, Lagoudianakis EE, Kekis P, Genetzakis M, Koutsoumanis K, Bramis I (2008) Thyroid surgery: comparison between the electrothermal bipolar vessel sealing system, harmonic scalpel, and classic suture ligation. Am J Surg 195:48–52
Shen WT, Baumbusch MA, Kebebew E, Duh QY (2005) Use of the electrothermal vessel sealing system versus standard vessel ligation in thyroidectomy. Asian J Surg 28:86–89
Alesina PF, Rolfs T, Walz MK (2010) Bipolar thermofusion vessel sealing system (TVS) versus conventional vessel ligation (CVL) in thyroid surgery-results of a prospective study. Langenbecks Arch Surg 395:115–119
Cakabay B, Sevinç MM, Gömceli I, Yenidogan E, Ulkü A, Koç S (2009) LigaSure versus clamp-and-tie in thyroidectomy: a single-center experience. Adv Ther 26:1035–1041
Hahn CH, Trolle W, Sørensen CH (2015) Harmonic focus in thyroidectomy for substernal goiter. Auris Nasus Larynx 42:311–317
Chang LY, O’Neill C, Suliburk J, Sidhu S, Delbridge L, Sywak M (2011) Sutureless total thyroidectomy: a safe and cost-effective alternative. ANZ J Surg 81:510–514
Anlar B, Karaman N, Dogan L, Ozaslan C, Atalay C, Altinok M (2013) The effect of harmonic scalpel, electrocautery, and scalpel use on early wound complications after modified radical mastectomy. Eur Surg Acta Chirurgica Austr 45:286–290
Archana A, Sureshkumar S, Vijayakumar C, Palanivel C (2018) Comparing the harmonic scalpel with electrocautery in reducing postoperative flap necrosis and seroma formation after modified radical mastectomy in carcinoma breast patients: a double-blind prospective randomized control trail. Cureus 10:e2476
Böhm D, Kubitza A, Lebrecht A, Schmidt M, Gerhold-Ay A, Battista M, Stewen K, Solbach C, Kölbl H (2012) Prospective randomized comparison of conventional instruments and the harmonic focus(®) device in breast-conserving therapy for primary breast cancer. Eur J Surg Oncol 38:118–124
Cortadellas T, Córdoba O, Espinosa-Bravo M, Mendoza-Santin C, Rodríguez-Fernández J, Esgueva A, Alvarez-Vinuesa M, Rubio IT, Xercavins J (2011) Electrothermal bipolar vessel sealing system in axillary dissection: a prospective randomized clinical study. Int J Surg 9:636–640
Deori A, Gupta N, Gupta AK, Yelamanchi R, Agrawal H, Durga CK (2021) A prospective randomised controlled study comparing ultrasonic dissector with electrocautery for axillary dissection in patients of carcinoma breast. MJMS 28:97–104
Dogan L, Gulcelik MA, Yuksel M, Uyar O, Erdogan O, Reis E (2012) The effect of plasmakinetic cautery on wound healing and complications in mastectomy. Eur J Surg Oncol 38:807–808
Faisal M, Fathy H, Shaban H, Abuelela ST, Marie A, Khaled I (2018) A novel technique of harmonic tissue dissection reduces seroma formation after modified radical mastectomy compared to conventional electrocautery: a single-blind randomized controlled trial. Patient Saf Surg 12:8
He Q, Zhuang D, Zheng L, Fan Z, Zhou P, Zhu J, Lv Z, Chai J, Cao L (2012) Harmonic focus versus electrocautery in axillary lymph node dissection for breast cancer: a randomized clinical study. Clin Breast Cancer 12:454–458
Iovino F, Auriemma PP, Ferraraccio F, Antoniol G, Barbarisi A (2012) Preventing seroma formation after axillary dissection for breast cancer: a randomized clinical trial. Am J Surg 203:708–714
Khan S, Khan S, Chawla T, Murtaza G (2014) Harmonic scalpel versus electrocautery dissection in modified radical mastectomy: a randomized controlled trial. Ann Surg Oncol 21:808–814
Kozomara D, Galić G, Brekalo Z, Sutalo N, Kvesić A, Soljić M (2010) A randomised two-way comparison of mastectomy performed using harmonic scalpel or monopolar diathermy. Coll Antropol 34:105–112
Lo Russo M, Amanti C, Lombardi A (2010) Axillary dissection using a new ultrasonic device. Eur J Cancer 8:137
Kontos M, Kothari A, Hamed H (2008) Effect of harmonic scalpel on seroma formation following surgery for breast cancer: a prospective randomized study. J BUON 13:223–230
Lumachi F, Basso SM, Santeufemia DA, Bonamini M, Chiara GB (2013) Ultrasonic dissection system technology in breast cancer: a case–control study in a large cohort of patients requiring axillary dissection. Breast Cancer Res Treat 142:399–404
Manjunath S, Ramesh RS, Goel V (2014) Ultrasonic shears versus electrocautery in axillary dissection for breast cancer—a randomized controlled trial. Indian J Surg Oncol 5:95–98
Meretoja TJ, von Smitten KA, Kuokkanen HO, Suominen SH, Jahkola TA (2008) Complications of skin-sparing mastectomy followed by immediate breast reconstruction: a prospective randomized study comparing high-frequency radiosurgery with conventional diathermy. Ann Plast Surg 60:24–28
Mittal P, Kumar A, Kaur S, Pandove PK, Singla RL, Singh J (2017) A comparative study of the use of harmonic scalpel versus unipolar cautery in modified radical mastectomy. Niger J Surg 23:20–25
Mori T, Abe H, Kawai Y, Murakami K, Akabori H, Yamaguchi T, Sonoda H, Shimizu T, Shiomi H, Kubota Y, Naka S, Murata S, Yamamoto H, Umeda T, Tani T (2013) Prospective, randomized trial comparing harmonic scalpel and electrocautery in breast surgery. J Clin Oncol 31:e12014
Rohaizak M, Khan FJ, Jasmin JS, Mohd Latar NH, Abdullah SS (2013) Ultracision versus electrocautery in performing modified radical mastectomy and axillary lymph node dissection for breast cancer: a prospective randomized control trial. Med J Malaysia 68:204–207
Nawaz A, Waqar S, Khan A, Mansoor R, Butt UI, Ayyaz M (2015) Harmonic scalpel versus electrocautery in axillary dissection in carcinoma breast. JCPSP 25:870–873
Salama AMF, Nawar AM, Zayed ME, Essa MS (2012) Evaluation of ultrasonic axillary dissection in preservation of intercostobrachial nerve and lymphatic sealing in breast cancer patients: randomized controlled trial. Ann Med Surg 60:255–260
Shanmugam S, Govindasamy G, Hussain SA, Prasanna Srinivasa Rao H (2017) Axillary dissection for breast cancer using electrocautery versus ultrasonic dissectors: a prospective randomized study. Indian J Cancer 54:543–546
Tukenmez M, Agcaoglu O, Aksakal N, Destek S, Cabioglu N, Barbaros U, Erbil Y, Bozbora A, Dinccag A, Ozmen V, Muslumanoglu M, Igci A (2014) The use of Ligasure vessel sealing system in axillary dissection; effect on seroma formation. Chirurgia (Bucur) 109:620–625
Yilmaz KB, Dogan L, Nalbant H, Akinci M, Karaman N, Ozaslan C (2011) Comparing scalpel, electrocautery and ultrasonic dissector effects: the impact on wound complications and pro-inflammatory cytokine levels in wound fluid from mastectomy patients. J Breast Cancer 14:58–63
Valeri A, Borrelli A, Presenti L, Lucchese M, Manca G, Tonelli P, Bergamini C, Borrelli D (2002) The influence of new technologies on laparoseopic adrenalectomy. Surg Endosc 16:1274–1279
Solaini L, Arru L, Merigo G, Tomasoni M, Gheza F, Tiberio GA (2013) Advanced sealing and dissecting devices in laparoscopic adrenal surgery. JSLS 17:622–626
Vettoretto N, Foglia E, Ferrario L, Gerardi C, Molteni B et al (2020) Could fluorescence-guided surgery be an efficient and sustainable option? A SICE (Italian Society of Endoscopic Surgery) health technology assessment summary. Surg Endosc 34:3270–3284
Acknowledgements
HTA-HED Collaborative Group:
Antonino Agrusa (Policlinico Giaccone di Palermo), Gabriele Anania (AOU di Ferrara), Alberto Arezzo (Università degli Studi di Torino), Gian Luca Baiocchi (Università di Brescia, ASST Cremona), Paolo Bianchi (ASST Santi Paolo e Carlo), Carlo Bergamini (AOU Careggi di Firenze), Graziano Ceccarelli (Ospedale di Foligno), Giancarlo D’Ambrosio (Policlinico Umberto I di Roma), Mario Guerrieri (AOU Ospedale Riuniti di Ancona), Andrea Lucchi (AUSL Romagna), Irnerio Muttillo (Azienda Complesso Ospedaliero San Filippo Neri), Wanda Petz (Divisione di Chirurgia dell’Apparato Digerente, IEO di Milano) e Gianfranco Silecchia (Dipartimento di Scienze Medico-Chirurgiche e Medicina Traslazionale, Facoltà di Medicina e Psicologia, Università Sapienza di Roma).
Funding
No funding obtained for this research paper.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Disclosures
Doctors Nereo Vettoretto, Emanuela Foglia, Chiara Gerardi, Emanuele Lettieri, Umberto Nocco, Emanuele Botteri, Umberto Bracale, Valerio Caracino, Francesco Maria Carrano, Elisa Cassinotti, Marco Giovenzana, Beatrice Giuliani, Angelo Iossa, Marco Milone, Giulia Montori, Roberto Peltrini, Giacomo Piatto, Mauro Podda, Alberto Sartori, Eleonora Allocati, Lucrezia Ferrario, Federica Asperti, Letizia Songia, Silvio Garattini, and Ferdinando Agresta have no conflicts of interest of financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
A list of the HTA-HED Collaborative Group authors and their affiliations appears at the acknowledgements.
Supplementary Information
Below is the link to the electronic supplementary material.

Fig. S1
: Adrenalectomy PRISMA. (JPG 66 KB)

Fig. S2
: Appendectomy PRISMA. (JPG 57 KB)

Fig. S3
: Breast surgery PRISMA. (JPG 57 KB)

Fig. S4
: Cholecystectomy PRISMA. (JPG 43 KB)

Fig. S5
: Colorectal surgery PRISMA. (JPG 46 KB)

Fig. S6
: Esophago-gastric surgery PRISMA. (JPG 95 KB)

Fig. S7
: Haemorrhoidectomy PRISMA. (JPG 61 KB)

Fig. S8
: Liver surgery PRISMA. (JPG 63 KB)

Fig. S9
: Pancreasectomy PRISMA. (JPG 59 KB)

Fig. S10
: Splenectomy PRISMA. (JPG 121 KB)

Fig. S11
: Thiroydectomy-parathiroidectomy PRISMA. (JPG 134 KB)
Table S1
: Adrenalectomy PICO and search strategy. (DOC 33 KB)
Table S2
: Appendectomy PICO and search strategy. (DOC 47 KB)
Table S3
: Breast surgery PICO and search strategy. (DOC 34 KB)
Table S4
: Cholecystectomy PICO and search strategy. (DOC 33 KB)
Table S5
: Colorectal surgery PICO and search strategy. (DOC 33 KB)
Table S6
: Esophago-gastric surgery PICO and search strategy. (DOC 33 KB)
Table S7
: Haemorrhoidectomy PICO and search strategy. (DOC 32 KB)
Table S8
: Liver surgery PICO and search strategy. (DOC 34 KB)
Table S9
: Pancreasectomy PICO and search strategy. (DOC 33 KB)
Table S10
: Splenectomy PICO and search strategy. (DOC 33 KB)
Table S11
: Thiroydectomy-parathiroydectomy PICO and search strategy. (DOC 33 KB)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Vettoretto, N., Foglia, E., Gerardi, C. et al. High-energy devices in different surgical settings: lessons learnt from a full health technology assessment report developed by SICE (Società Italiana di Chirurgia Endoscopica). Surg Endosc 37, 2548–2565 (2023). https://doi.org/10.1007/s00464-022-09734-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-022-09734-5