Abstract
Background
Colonoscopy is a mainstay to detect premalignant neoplastic lesions in the colon. Real-time Artificial Intelligence (AI)-aided colonoscopy purportedly improves the polyp detection rate, especially for small flat lesions. The aim of this study is to evaluate the performance of real-time AI-aided colonoscopy in the detection of colonic polyps.
Methods
A prospective single institution cohort study was conducted in Singapore. All real-time AI-aided colonoscopies, regardless of indication, performed by specialist-grade endoscopists were anonymously recorded from July to September 2021 and reviewed by 2 independent authors (FHK, JL). Sustained detection of an area by the program was regarded as a “hit”. Histology for the polypectomies were reviewed to determine adenoma detection rate (ADR). Individual endoscopist’s performance with AI were compared against their baseline performance without AI endoscopy.
Results
A total of 24 (82.8%) endoscopists participated with 18 (62.1%) performing ≥ 5 AI-aided colonoscopies. Of the 18, 72.2% (n = 13) were general surgeons. During that 3-months period, 487 “hits” encountered in 298 colonoscopies. Polypectomies were performed for 51.3% and 68.4% of these polypectomies were adenomas on histology. The post-intervention median ADR was 30.4% was higher than the median baseline polypectomy rate of 24.3% (p = 0.02). Of the adenomas excised, 14 (5.6%) were sessile serrated adenomas. Of those who performed ≥ 5 AI-aided colonoscopies, 13 (72.2%) had an improvement of ADR compared to their polypectomy rate before the introduction of AI, of which 2 of them had significant improvement.
Conclusions
Real-time AI-aided colonoscopy have the potential to improved ADR even for experienced endoscopists and would therefore, improve the quality of colonoscopy.
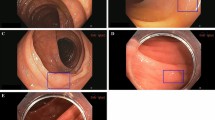
Graphical abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Periodic colonoscopy assessment has been recognised as the modality of choice to assess the colon for polyps by numerous endoscopic society guidelines [1,2,3,4,5]. Society like the American and European Society for Gastrointestinal Endoscopy (ASGE and ESGE) acknowledges the diagnostic and therapeutic ability afforded by colonoscopy, allowing the endoscopists to not only identify colonic lesions but also to excise premalignant lesions in the same setting, potentially eradicate the progression to malignancy [1, 3, 4, 6, 7].
Along with advanced endoscopic excisional techniques like endoscopic submucosal dissection, the identification and characterisation of colonic polyps are difficult skillsets to acquire [8]. Mastering these skillsets require a combination of studying endoscopic atlases and hands-on experience, the latter of which inevitably requires time [9, 10]. Identification of the polyps during colonoscopy requires a combination of meticulous mucosal exposure, inspection and recognition of vascular-pit patterns and mucosal fold distortion [8,9,10]. Invariably, all these are both physically and mentally demanding on the endoscopists during the short span of time of the colonoscopy. Cumulating these demands for all the endoscopic procedures the endoscopists must perform in each session, the task at hand is nothing short of challenging.
Artificial intelligence (AI) aims to aid the endoscopists to reduce the complexity of colonoscopy. AI, first mentioned in the 1950s, has greatly improve after the turn of the millennium, especially after the incorporation of deep learning algorithms [11,12,13,14,15,16,17,18,19]. AI has increasingly been incorporated into various aspect of healthcare. Applications of AI include managing population health, accelerating drug discovery especially during the COVID-19 pandemic and improving diagnostics like in radiology and histopathology proves that AI can successfully be integrated with the rigors and demands of healthcare [20]. In the last 5 years, there have been programs by various companies which allow real-time, computer-aid detection (CADe) of polyps during colonoscopy [21, 22]. However, at the time of writing, there have yet to be any evidence on the improvement AI-aided colonoscopy has on individual endoscopist. In addition, details on the rate of identification of sessile serrated adenomas (SSA), which are notoriously difficult to identify, by these AI programs are still lacking.
The aim of this study is to report the performance of the GI Genius™ Intelligent Endoscopy Module (US-DG-2000309 © 2021 Medtronic), a real-time CADe of polyps program, to detect adenomatous lesion, including SSA. The secondary aim of this study is also to evaluate, collectively and individually, how polyp and adenoma detection rates (ADR) were affected by the real-time CADe of polyps program.
Methodology
After Institutional Review Board approval was obtained, an investigator-initiated, prospective cohort study was performed in a single referral centre in Singapore, from 1 July 2021 to 30 Sept 2021. This coincided with the trial period of a real-time AI-assisted colonoscopy device (GI Genius™ Intelligent Endoscopy Module, US-DG-2000309 © 2021 Medtronic) made available to the endoscopy unit of the institution. The device was paired with the pre-existing Olympus EVIS EXERA III 190 Video endoscopy system (Olympus Medical System Corp., Shinjuku Monolith, Shinjuku-ku, Tokyo, Japan) in the institution’s Endoscopy Centre.
All colonoscopy, regardless of indication to represent the realistic performance of the AI device, that were performed in the rooms fitted with the AI module were included into the study. These colonoscopies were performed in the usual fashion by specialist-grade endoscopists (gastroenterologists or general surgeons) as per the institution’s usual practice. The videos of these colonoscopies were recorded and retrospectively reviewed by two experienced endoscopists who have had at least 10 years of colonoscopy experienced (FHK and JL).
During the video review, each persistent green box highlighting a mucosal abnormality was defined as a “hit”, complete polyp removals, be it whole or in a piecemeal fashion, either by using forceps or snares, were defined as a “polypectomy”. The ratio of polypectomies to hit rate was calculated. The nature of all polypectomies performed during the trial period was compared with their respective histopathological report and adenomatous lesions were classified as an “adenoma”. In addition to the adenoma detection rate (ADR), the ratio of the number of colonoscopies with adenoma detected to the total number of colonoscopies was also calculated. The number of sessile serrated adenomas (SSA) excised and confirmed histologically were also recorded.
The number of AI-guided colonoscopies performed per endoscopists were recorded and their performances were compared to each endoscopist’s baseline polypectomy rate based on the last 3 years hospital audit performance. The baseline adenoma detection rate for each endoscopists was not available. To determine the effect of real-time CADe, the changes between the ADR during the study was compared against each endoscopist’s baseline polypectomy rate, where the baseline ADR was deemed to be equal or less than the baseline polypectomy rate.
All statistical data were handled with Stata v. 17.0 software (Stata Corporation LLC, College Station, USA). Categorical data were presented as proportions or rates and the Z-test was used as the test for difference. Continuous variables were treated using their median value with inter-quartile ranges described, Mann–Whitney U test was performed for the test of difference between continuous variables. A p-value of ≤ 0.05 was considered to be statistically significant. To account for the familiarisation time with the CADe of polyp program, only endoscopists who had performed at least 5 procedures using the system in the 3-month period were analysed for their individual performance.
Results
Over a 3-month period, 298 recorded colonoscopies were performed with the real-time CADe of polyp program in our institution. A total of 18 of the 29 (62.1%) specialist-grade endoscopists, 50.0% (5/10) of the gastroenterologists and 68.4% (13/19) of the general surgeons, clocked at least 5 procedures using the system. Table 1 provides further details of the endoscopists involved in the study.
After video review by 2 independent endoscopists, there were 487 “hits” picked up in the 298 colonoscopies performed. Polypectomies were performed for 51.3% of the “hits” and the 68.4% of the polypectomies performed was histologically proven to be adenomatous lesions. Out of the 250 polyps removed, 14 (5.6%) of which were found to be sessile serrated adenomas on histology. Table 2 provides details of the outcome of the AI-aided colonoscopies.
The post-intervention collective ADR was 30.4% was higher than the baseline polypectomy rate of 24.3% (p = 0.02). Of the 18 endoscopists who had performed at least 5 AI-aid colonoscopies during the study period, 13 of them (72.2%) had an individual ADR rate that was higher than that of their baseline polypectomy rate without CADe of polyp. Of those who improved, 2 of them experienced significant improvement in ADR. The median improvement was 8.5% (IQR: − 2.8 to 17.8). Of note, most of the endoscopists (7/8, 87.5%) who had performed 10 or more AI-aided colonoscopies showed improvement of their ADR as compared to their baseline polypectomy rate without AI. Table 3 details the breakdown of the individual endoscopists’ performance with and without the AI technology.
Discussion
Our single institution experience revealed that with the incorporation of the real-time CADe of polyps program resulted in a median 8.5% (IQR: − 0.03 to 17.8%) improvement in individual endoscopist’s ADR from their baseline polypectomy rate. This potentially means that the true ADR improvement after the introduction of AI technology is greater than that. Of note, 5.6% (n = 14) of the polypectomies (n = 250) performed during the study period was found to be SSA on histology. Based on existing endoscopy literature, where CADe of polyps program was not used, this rate is already higher than the usual expected SSA rate of 2–3% [23, 24]. These results highlighted that pairing real-time AI technology with colonoscopy does help experienced endoscopists identify more adenomatous lesions and improves the detection of notoriously difficult lesions to identify with the naked eye, improving the quality of colonoscopy. This is consistent with other publication utilising other real-time AI-aided polyp detection program of different brands, providing assurance that AI has a part to play in endoscopic assessment of the colon [25, 26].
A recent meta-analysis highlighted that the CADe of polyp had a sensitivity of 95% (95% CI 0.95–0.98) [26]. In our experience, of the 18 endoscopist who had at least 10 procedures done with AI program, the median ADR was 28.5% (IQR 23.0–40.0). Such high sensitivity modality can potentially help reduce the variation of quality which is highly user dependent. The reduction of variability of quality would ultimately benefit the patients coming for colonoscopy and gives them good confidence regardless of the endoscopists [25, 27,28,29]. This is especially important for endoscopists with lower procedural volume (i.e., “part-time” endoscopists) to help reduce their variability and maintain high standards of colonoscopic evaluation for their patients. From the training angle, consultant endoscopists may then have more reassurance to allow trainee endoscopists perform colonoscopy on their behalf under direct or oversight supervision [30]. From the trainees point-of-view, being able to perform more endoscopies would also potentially allow a quicker ascend for these trainees to attain competence [8].
As alluded to earlier, polyp detection depends on 2 main factors, identification of mucosal abnormalities and adequate colonic mucosal exposure [8,9,10]. Real-time CADe of polyps helps to mitigate the learning curve of the endoscopist to identify mucosal abnormalities, however, the endoscopists would still have to expose adequate mucosal for the AI technology to work. With the AI program, endoscopists can then focus on honing their skills to perform an optimal mucosal exposure for polyp identification. Upon the detection of a possible polyp by the real-time AI program, endoscopists would still need to be well-versed with polyp characterisation to identify which “hits” requires to be excised and which “hits” are false positives. As one gets more comfortable with the AI-aided programme, one would expect to get better at characterisation of polyps, and reduce the false positive polypectomies which are not without its risks of bleeding or perforation. Another factor that may affect polyp detection rate is the quality of the bowel preparation [31, 32]. This can be mitigated by the adherence to evidence-based recommendation of split preparation with one or more bowel preparation agents. Suffice to conclude, the role of the endoscopists still remains vital even if AI technology is used and AI will, therefore, not be able to replace the requirement of good technical skills during colonoscopy.
One of the limitations of this study is the short duration and limited sample size. However, the size of the study population here is comparable with similar studies in literature. The study unique point would be to evaluate the performance of the CADe of polyps device collectively, as an institutional experience, and provide a breakdown for individual endoscopist’s performance, the latter being absent in numerous other similar studies. We also presented the performance of 18 specialist-grade endoscopists performance in this study and anonymised video recordings of all colonoscopy were reviewed by 2 independent specialist-grade endoscopists. This may provide a fair and objective representation of the variability of performance across the different users. The heterogeneous recruited patient population may result in some bias, however, the authors felt that the recruitment of all colonoscopies performed in our unit within the study duration provided generalisable and realistic assessment of the AI technology in our every day practice.
To our knowledge, this is only the second independent review of the GI Genius™ Intelligent Endoscopy Module (US-DG-2000309 © 2021 Medtronic) [33]. This module, which provides real-time CADe of polyps, is “brand agnostic”, compatible with most existing endoscopy stacks, from all companies, that is use across the world. In our unit, we paired the module up with the Olympus EVIS EXERA III 190 Video endoscopy system (Olympus Medical System Corp., Shinjuku Monolith, Shinjuku-ku, Tokyo, Japan). By providing the review of this system, it provides an opportunity to critically review an AI program that can potentially be paired up with currently existing endoscopy stakes across the world and have a far-reaching impact on the adoption of AI in colonoscopy. The GI Genius™ Intelligent Endoscopy Module does not consist of a continual machine learning algorithm, thus, upgrades of technology are possible through software update at regular intervals by Medtronic.
Without a doubt, AI technology is a useful tool in today’s world of healthcare and health service delivery. Embracing a technology that works and continue to improve would be important not just to provide better quality care for patients, but also ease the demands and safeguards the interests on the healthcare provider. Endoscopy surveillance guidelines recommends a scope to be performed up to 10 years later after a normal colonoscopy, that to many is an awfully long time later and post-colonoscopy colorectal cancer development is the main reason why many endoscopists may favor to repeat a scope earlier than recommended [34]. Now, with the assistance from AI and paired with a skilled endoscopists, one can be more certain to then comply better with the recommended guidelines.
Moving forward, future studies using real-time AI-guided CADe should focus on evaluating the utility of CADe in education for endoscopy. Evaluating the learning curve of novice endoscopist in the characterisation and identification with and without CADe in comparison with experience endoscopists may introduce a different dimension on the utilisation of CADe and a paradigm shift to how endoscopy can be taught.
Conclusion
Our single centre experience with a real-time AI-aided CADe of polyps during colonoscopy has showed a significantly improved collective ADR rate compared to baseline and a higher-than-expected SSA detection rate. Individually, there was also an ADR improvement by most endoscopist. Therefore, real-time AI-aided colonoscopy have the potential to improved ADR even for experienced endoscopists and would therefore, improve the quality of colonoscopy.
References
Abu-Freha N, Katz LH, Kariv R, Vainer E, Laish I, Gluck N et al (2021) Post-polypectomy surveillance colonoscopy: comparison of the updated guidelines. Unit Eur Gastroenterol J 9(6):681–687
Atkin W, Dadswell E, Wooldrage K, Kralj-Hans I, von Wagner C, Edwards R et al (2013) Computed tomographic colonography versus colonoscopy for investigation of patients with symptoms suggestive of colorectal cancer (SIGGAR): a multicentre randomised trial. Lancet 381(9873):1194–1202
Bisschops R, East JE, Hassan C, Hazewinkel Y, Kaminski MF, Neumann H et al (2019) Advanced imaging for detection and differentiation of colorectal neoplasia: European Society of Gastrointestinal Endoscopy (ESGE) guideline—update 2019. Endoscopy 51(12):1155–1179
Jorgensen B, Knudtson J (2015) Stop cancer colon. Colorectal cancer screening--updated guidelines. S D Med; Spec No:82-7.
Kahi CJ, Boland CR, Dominitz JA, Giardiello FM, Johnson DA, Kaltenbach T, et al (2016) Colonoscopy surveillance after colorectal cancer resection: recommendations of the US Multi-Society Task Force on colorectal cancer. Am J Gastroenterol 111(3):337–346 (quiz 47)
Hassan C, Wysocki PT, Fuccio L, Seufferlein T, Dinis-Ribeiro M, Brandao C et al (2019) Endoscopic surveillance after surgical or endoscopic resection for colorectal cancer: European Society of Gastrointestinal Endoscopy (ESGE) and European Society of Digestive Oncology (ESDO) guideline. Endoscopy 51(3):266–277
Kaltenbach T, Anderson JC, Burke CA, Dominitz JA, Gupta S, Lieberman D et al (2020) Endoscopic removal of colorectal lesions-recommendations by the US Multi-Society Task Force on colorectal cancer. Gastroenterology 158(4):1095–1129
Chan DKH, Wong RKM, Yeoh KG, Tan KK (2018) Accredited residents perform colonoscopy to the same high standards as consultants. Surg Endosc 32(3):1377–1381
Hill A, Horswill MS, Plooy AM, Watson MO, Rowlands LN, Wallis GM et al (2017) Assessment of colorectal polyp recognition skill: development and validation of an objective test. Surg Endosc 31(6):2426–2436
Yoon JY, Cha JM (2016) Can we measure the learning curve of colonoscopy using polyp detection rate? Clin Endosc 49(1):6–7
Ahmad OF, Gonzalez-Bueno Puyal J, Brandao P, Kader R, Abbasi F, Hussein M et al (2021) Performance of artificial intelligence for detection of subtle and advanced colorectal neoplasia. Dig Endosc 34:862–869
Alagappan M, Brown JRG, Mori Y, Berzin TM (2018) Artificial intelligence in gastrointestinal endoscopy: the future is almost here. World J Gastrointest Endosc 10(10):239–249
Azer SA (2019) Challenges facing the detection of colonic polyps: what can deep learning do? Medicina (Kaunas) 55(8):473
Becq A, Chandnani M, Bharadwaj S, Baran B, Ernest-Suarez K, Gabr M et al (2020) Effectiveness of a deep-learning polyp detection system in prospectively collected colonoscopy videos with variable bowel preparation quality. J Clin Gastroenterol 54(6):554–557
Glissen Brown JR, Mansour NM, Wang P, Chuchuca MA, Minchenberg SB, Chandnani M et al (2021) Deep learning computer-aided polyp detection reduces adenoma miss rate: a United States multi-center randomized tandem colonoscopy study (CADeT-CS Trial). Clin Gastroenterol Hepatol 20:1499–1507
Roth HR, Lu L, Liu J, Yao J, Seff A, Cherry K et al (2016) Improving computer-aided detection using convolutional neural networks and random view aggregation. IEEE Trans Med Imaging 35(5):1170–1181
Wang P, Liu X, Berzin TM, Glissen Brown JR, Liu P, Zhou C et al (2020) Effect of a deep-learning computer-aided detection system on adenoma detection during colonoscopy (CADe-DB trial): a double-blind randomised study. Lancet Gastroenterol Hepatol 5(4):343–351
Yamada M, Saito Y, Imaoka H, Saiko M, Yamada S, Kondo H et al (2019) Development of a real-time endoscopic image diagnosis support system using deep learning technology in colonoscopy. Sci Rep 9(1):14465
Zhao SB, Yang W, Wang SL, Pan P, Wang RD, Chang X et al (2021) Establishment and validation of a computer-assisted colonic polyp localization system based on deep learning. World J Gastroenterol 27(31):5232–5246
Georgiou KE, Georgiou E, Satava RM (2021) 5G use in healthcare: the future is present. JSLS. https://doi.org/10.4293/JSLS.2021.00064
Milluzzo SM, Cesaro P, Grazioli LM, Olivari N, Spada C (2021) Artificial intelligence in lower gastrointestinal endoscopy: the current status and future perspective. Clin Endosc 54(3):329–339
Repici A, Spadaccini M, Antonelli G, Correale L, Maselli R, Galtieri PA et al (2021) Artificial intelligence and colonoscopy experience: lessons from two randomised trials. Gut 71:757–765
Desai M, Anderson JC, Kaminski M, Thoguluva Chandrasekar V, Fathallah J, Hassan C et al (2021) Sessile serrated lesion detection rates during average risk screening colonoscopy: a systematic review and meta-analysis of the published literature. Endosc Int Open 9(4):E610–E620
Sonnenberg A, Turner KO, Genta RM (2022) Trends of colonic neoplasia in US outpatient endoscopy centers. Dig Dis Sci. https://doi.org/10.1007/s10620-021-07358-8
Ashat M, Klair JS, Singh D, Murali AR, Krishnamoorthi R (2021) Impact of real-time use of artificial intelligence in improving adenoma detection during colonoscopy: a systematic review and meta-analysis. Endosc Int Open 9(4):E513–E521
Huang D, Shen J, Hong J, Zhang Y, Dai S, Du N et al (2021) Effect of artificial intelligence-aided colonoscopy for adenoma and polyp detection: a meta-analysis of randomized clinical trials. Int J Colorectal Dis 37:495–506
Antonelli G, Badalamenti M, Hassan C, Repici A (2021) Impact of artificial intelligence on colorectal polyp detection. Best Pract Res Clin Gastroenterol 52–53:101713
Antonelli G, Gkolfakis P, Tziatzios G, Papanikolaou IS, Triantafyllou K, Hassan C (2020) Artificial intelligence-aided colonoscopy: recent developments and future perspectives. World J Gastroenterol 26(47):7436–7443
Lee J, Wallace MB (2021) State of the art: the impact of artificial intelligence in endoscopy 2020. Curr Gastroenterol Rep 23(5):7
Yoshida N, Inoue K, Tomita Y, Kobayashi R, Hashimoto H, Sugino S et al (2021) An analysis about the function of a new artificial intelligence, CAD EYE with the lesion recognition and diagnosis for colorectal polyps in clinical practice. Int J Colorectal Dis 36(10):2237–2245
Hassan C, East J, Radaelli F, Spada C, Benamouzig R, Bisschops R et al (2019) Bowel preparation for colonoscopy: European Society of Gastrointestinal Endoscopy (ESGE) guideline—update 2019. Endoscopy 51(8):775–794
Menees SB, Elliott E, Govani S, Anastassiades C, Judd S, Urganus A et al (2014) The impact of bowel cleansing on follow-up recommendations in average-risk patients with a normal colonoscopy. Am J Gastroenterol 109(2):148–154
Spadaccini M, Marco A, Franchellucci G, Sharma P, Hassan C, Repici A (2022) Discovering the first FDA-approved computer-aided polyp detection system. Future Oncol 18:1405–1412
Koh FH, Chan DKH, Ng J, Tan KK (2019) Adherence to surveillance guidelines following colonic polypectomy is abysmal. J Gastrointest Oncol 10(2):166–170
Acknowledgment
SKH Endoscopy Centre members: Fung-Joon Foo, Winson J. Tan, Sharmini S. Sivarajah, Leonard M. L. Ho, Jia-Lin Ng, Frederick H. Koh, Cheryl Chong, Darius Aw, Juinn-Haur Kam, Alvin YH Tan, Choon-Chieh Tan, Baldwin P. M. Yeung, Wai-Keong Wong, Bin-Chet Toh, Jasmine Ladlad, Jason Barco, Koy-Min Chue, Faith Leong, Christopher Kong, Cui-Li Lin, Eng-Kiong Teo, Yi-Kang Ng, Tze-Tong Tey, Marianne A. De-Roza, Jonathan Lum, Xiaoke Li, Jinliang Li, Nazeemah B. Mohd-Nor, Siok-Peng Ng.
Funding
No funding was provided for this study. However, the GI Genius™ Intelligent Endoscopy Module (US-DG-2000309 © 2021 Medtronic) was provided free to the institution during the study period as a form a loan for trial.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Disclosures
Drs Frederick H Koh, Jasmine Ladlad, Eng-Kiong Teo, Cui-Li Lin, Fung-Joon Foo and co-authors within SKH Endoscopy Centre have no conflicts of interest or financial ties to disclose. The GI Genius™ Intelligent Endoscopy Module (US-DG-2000309 © 2021 Medtronic) was provided free to the institution during the study period as a form a loan for trial.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The members of SKH Endoscopy Centre are listed in Acknowledgements.
Rights and permissions
About this article
Cite this article
Koh, F.H., Ladlad, J., SKH Endoscopy Centre. et al. Real-time artificial intelligence (AI)-aided endoscopy improves adenoma detection rates even in experienced endoscopists: a cohort study in Singapore. Surg Endosc 37, 165–171 (2023). https://doi.org/10.1007/s00464-022-09470-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-022-09470-w