Abstract
Background
Trocar site hernia (TSH) is often underestimated after minimally invasive surgery. Scarce information is available about the incidence of TSH in patients undergoing laparoscopic hernioplasty. We aimed to evaluate the incidence and risk factors of umbilical TSH after laparoscopic TAPP hernioplasty in patients with and without an associated umbilical hernia.
Methods
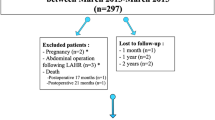
A retrospective analysis of a prospectively collected database of all patients who underwent laparoscopic inguinal TAPP repair during 2013–2018 was performed. After TAPP repair, the umbilical fascia was closed either by a figure-of-eight stitch with absorbable suture (G1) or by umbilical hernioplasty if it was present (G2). Multivariate logistic regression analysis was used to determine the TSH risk factors. Comparative evaluation regarding demographics, and operative and postoperative variables was performed.
Results
A total of 535 laparoscopic TAPP repairs were included. There were 359 (67.1%) patients in G1 and 176 in G2 (32.9%). Surgical site infection was higher in G2 (G1: 0.6% vs G2: 5.7%, p = 0.001). Overall TSH rate was 3.9% after a mean follow-up of 20 (12–41) months. Performing a concomitant umbilical repair significantly increased the risk of umbilical TSH (G1: 2.2% vs G2: 7.4%, p = 0.004). TSH rates in G2 were similar in patients with simple suture or mesh repairs (p = 0.88). Rectus abdominis diastasis (OR 37.8, 95% CI:8.22–174.0, p < 0.001) and inguinal recurrence (OR 13.5, 95% CI:2.04–89.5, p = 0.007) were independent risk factors for TSH.
Conclusion
Although trocar site hernia after laparoscopic TAPP repair has a low incidence, its risk is significantly increased in patients with a concomitant umbilical hernia repair, rectus abdominis diastasis, and/or inguinal recurrence.
Similar content being viewed by others
References
Rutkow IM (2003) Demographic and socioeconomic aspects of hernia repair in the United States in 2003. Surg Clin North Am 83:1045–1051
Abbas AE, Abd Ellatif ME, Noaman N (2012) Patient-perspective quality of life after laparoscopic and open hernia repair a controlled randomized trial. Surg Endosc 26(9):2465–2470
Perez AJ, Strassle PD, Sadava EE, Gaber C, Schlottmann F (2020) Nationwide analysis of inpatient laparoscopic versus open inguinal hernia repair. J Laparoendosc Adv Surg Tech 30(3):292–298
The HerniaSurge Group (2018) International guidelines for groin hernia management. Hernia 22:1–165
Helgstrand F, Rosenberg J, Bisgaard T (2011) Trocar site hernia after laparoscopic surgery: a qualitative systematic review. Hernia 15:113–121
Schmedt CG, Leibl BJ, Daubler P, Bittner R (2001) Access-related complications–an analysis of 6023 consecutive laparoscopic hernia repairs. Min Invas Ther & Allied Technol 10:23–30
Comajuncosas J, Vallverdú H, Orbeal R, Parés D (2011) Trocar site incisional hernia in laparoscopic surgery. Cirugía Española (English Edition) 89(2):72–76
Helgstrand F, Rosenberg J, Bisgaard T (2010) Trocar site hernia after laparoscopic surgery: a qualitative systematic review. Hernia 15(2):113–121
Schmedt C-G, Leibl BJ, Däubler P, Bittner R (2001) Access-related complications–an analysis of 6023 consecutive laparoscopic hernia repairs. Minim Invasive Ther Allied Technol 10(1):23–30
Hussain A, Mahmood H, Singhal T, Balakrishnan S, Nicholls J, El-Hasani S (2009) Long-term study of port-site incisional hernia after laparoscopic procedures. JSLS 13:346–434
Tonouchi H, Ohmori Y, Kobayashi M, Kusunoki M (2004) Trocar site hernia. Arch Surg 139(11):1248–1256
Wells A, Germanos GJ, Salemi JL, Mikhail E (2019) Laparoscopic surgeons’ perspectives on risk factors for and prophylaxis of trocar site hernias: a multispecialty national survey. JSLS. https://doi.org/10.4293/JSLS.2019.00013
Leibl BJ, Schmedt CG, Schwarz J, Kraft K, Bittner R (1999) Laparoscopic surgery complications associated with trocar tip design: review of literature and own results. J Laparoendosc Adv Surg Tech 9:135–140
Peña ME, Dreifuss NH, Schlottmann F, Sadava EE (2019) Could long-term follow-up modify the outcomes after laparoscopic TAPP? a 5-year retrospective cohort study. Hernia 23(4):693–698
Nofal MN, Yousef AJ, Hamdan FF, Oudat AH (2020) Characteristics of trocar site hernia after laparoscopic cholecystectomy. Scientific Reports 10:2868
Karampinis I, Lion E, Hetjens S, Vassilev G, Galata C, Reissfelder C, Otto M (2020) Trocar site HERnias after bariatric laparoscopic surgery (HERBALS): a prospective cohort study. Obes Surg 30(5):1820–1826
Lago J, Serralta D, García A, Martín J, Sanz M, Pérez MD, Turégano F (2011) Randomized prospective trial on the occurrence of laparoscopic trocar site hernias. J Laparoendosc Adv Surg Tech 21(9):775–779
Sadava EE, Kerman Cabo J, Carballo FH, Bun ME, Rotholtz NA (2014) Incisional hernia after laparoscopic colorectal surgery. Is there any factor associated? Surg Endosc. 28(12):3421–3424
Swank HA, Mulder IM, la Chapelle CF, Reitsma JB, Lange JF, Bemelman WA (2011) Systematic review of trocar-site hernia. Br J Surg 99(3):315–323
Köhler G, Luketina R-R, Emmanuel K (2014) Sutured repair of primary small umbilical and epigastric hernias: concomitant rectus diastasis is a significant risk factor for recurrence. World J Surg 39(1):121–126
Ranney B (1990) Diastasis recti and umbilical hernia causes, recognition and repair. S D J Med 43(10):5–8
Hay J-M, Boudet M-J, Fingerhut A, Pourcher J, Hennet H, Habib E, Flamant Y (1995) Shouldice inguinal hernia repair in the male adult. Ann Surg 222(6):719–727
Klinge U, Junge K, Mertens PR (2004) Herniosis: a biological approach. Hernia 8(4):300–301
Antoniou SA, Antoniou GA, Koch OO, Pointner R, Granderath FA (2013) Blunt versus bladed trocars in laparoscopic surgery: a systematic review and meta-analysis of randomized trials. Surg Endosc 27(7):2312–2320
Azurin DJ, Go LS, Arroyo LR, Kirkland ML (1995) Trocar site herniation following laparoscopic cholecystectomy and the significance of an incidental preexisting umbilical hernia. Am Surg. Aug 61(8):718–720
Kaufmann R, Halm JA, Eker HH, Klitsie PJ, Nieuwenhuizen J, van Geldere D, Simons MP, van der Harst E, van 'tRiet M, van der Holt B, Kleinrensink GJ, Jeekel J, Lange JF (2018) Mesh Versus Suture Repair of Umbilical Hernia in Adults: A Randomised, Double-Blind, Controlled. Multicentre Trial. Lancet. 391(10123):860–869
Acknowledgements
None.
Author information
Authors and Affiliations
Contributions
CBH, NHD, FS, and EES involved in conception and design of the work; acquisition, analysis, and interpretation of data for the work; and drafting and revising of the manuscript.
Corresponding author
Ethics declarations
Disclosures
Camila Bras Harriott, Nicolas H. Dreifuss, Francisco Schlottmann, and Emmanuel E. Sadava have no conflict of interest or financial ties to disclose. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Harriott, C.B., Dreifuss, N.H., Schlottmann, F. et al. Incidence and risk factors for umbilical trocar site hernia after laparoscopic TAPP repair. A single high-volume center experience. Surg Endosc 35, 5167–5172 (2021). https://doi.org/10.1007/s00464-020-08007-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-020-08007-3