Abstract
Background
Despite advances in diagnostic imaging capabilities, little information exists concerning the impact of physical dimensions of a paraesophageal hernia (PEH) on intraoperative decision making. The authors hypothesized that computerized volumetric analysis and multidimensional visualization to measure hiatal defect area (HDA) and intrathoracic hernia sac volume (HSV) would correlate to operative findings and required surgical techniques performed.
Methods
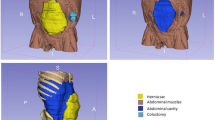
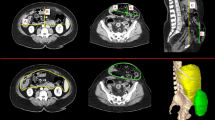
Using volumetric analysis software (Aquarius iNtuition, TeraRecon, Inc), HDA and HSV were measured in PEH patients with preoperative computerized tomography (CT) scans, and used to predict the likelihood of intraoperative variables. Multidimensional rotation of images enabled visualization of the entire hiatal defect in a plane mimicking the surgeon’s view during repair. The intrathoracic hernia sac was outlined producing volume measurements based on a summation of exact dimensions.
Results
A total of 213 PEHR patients had preoperative CT imaging, with 14.1% performed emergently. Primary cruroplasty was performed in 89.2%, salvage gastropexy in 10.3%, and diaphragmatic relaxing incisions in 4.2%. Median HDA was 25.7 cm2 (IQR17.8–35.6 cm2); median HSV was 365.0 cm3 (IQR150.0–611.0 cm3). Incremental 5 cm2 increase in HDA was associated with greater likelihood of presenting emergently (OR 1.27; 95%CI 1.124–1.428, p = 0.0001), incarceration (OR 1.27; 1.074–1.499, p = 0.005), gastric volvulus (OR 1.13; 1.021–1.248, p = 0.02), and requiring either relaxing incision (OR 1.43; 1.203–1.709, p < 0.0001) or salvage gastropexy (OR 1.13; 1.001–1.274, p = 0.04). Similarly, HSV increases of 100 cm3 were associated with 23% greater likelihood of emergent repair (CI 1.121–1.353, p < 0.0001), and were more likely to require a relaxing incision (OR 1.18; 1.043–1.339, p = 0.009) or salvage gastropexy (1.19; 1.083–1.312, p = 0.0003).
Conclusions
Utilization of CT volumetric measurements is a valuable adjunct in preoperative planning, allowing the surgeon to anticipate complexity of repair and operative approach, as incremental increases in HSV by 100 cm3 and HDA by 5 cm2 are more likely to require complex techniques or bailout procedures and/or present emergently.


Similar content being viewed by others
References
Landreneau RJ, Johnson JA, Marshall JB, Hazelrigg SR, Boley TM, Curtis JJ (1992) Clinical spectrum of paraesophageal herniation. Dig Dis Sci 37:537–544. https://doi.org/10.1007/BF01307577
Sihag S, Rattner DW (2016) Management of complicated and strangulated hiatal hernias. Acute Care Surg Handb 2:65–90
Bawahab M, Mitchell P, Church N, Debru E (2009) Management of acute paraesophageal hernia. Surg Endosc 23:255–259. https://doi.org/10.1007/s00464-008-0190-8
Demeester SR (2013) Laparoscopic paraesophageal hernia repair: critical steps and adjunct techniques to minimize recurrence. Surg Laparosc Endosc Percutan Tech 23:429–435
Zaman JA, Lidor AO (2016) The optimal approach to symptomatic paraesophageal hernia repair: important technical considerations. Curr Gastroenterol Rep 18(10):53. https://doi.org/10.1007/s11894-016-0529-6
Soper NJ, Dunnegan D (1999) Anatomic fundoplication failure after laparoscopic antireflux surgery. Ann Surg 229:669–677. https://doi.org/10.1097/00000658-199905000-00009
Carlson MA, Frantzides CT (2001) Complications and results of primary minimally invasive antireflux procedures: a review of 10,735 reported cases. J Am Coll Surg 193:428–439. https://doi.org/10.1016/S1072-7515(01)00992-9
Balague C, Trias M, Garriga J, Targarona EM, Martinez C (2007) The massive hiatal hernia: dealing with the defect. Surg Innov 11:161–169. https://doi.org/10.1177/107155170401100305
Bradley DD, Louie BE, Farivar AS, Wilshire CL, Baik PU, Aye RW (2015) Assessment and reduction of diaphragmatic tension during hiatal hernia repair. Surg Endosc 29:796–804. https://doi.org/10.1007/s00464-014-3744-y
Greene CL, Demeester SR, Zehetner J, Worrell SG, Oh DS, Hagen JA (2013) Diaphragmatic relaxing incisions during laparoscopic paraesophageal hernia repair. Surg Endosc 27:4532–4538. https://doi.org/10.1007/s00464-013-3107-0
Crespin OM, Yates RB, Martin AV, Pellegrini CA, Oelschlager BK (2016) The use of crural relaxing incisions with biologic mesh reinforcement during laparoscopic repair of complex hiatal hernias. Surg Endosc 30:2179–2185. https://doi.org/10.1007/s00464-015-4522-1
Swanstrom LL, Marcus DR, Galloway GQ (1996) Laparoscopic collis gastroplasty is the treatment of choice for the shortened esophagus. Am J Surg 171:477–481. https://doi.org/10.1016/S0002-9610(96)00008-6
Alicuben ET, Worrell SG, DeMeester SR (2014) Impact of crural relaxing incisions, collis gastroplasty, and non–cross-linked human dermal mesh crural reinforcement on early hiatal hernia recurrence rates. J Am Coll Surg 219:988–992. https://doi.org/10.1016/j.jamcollsurg.2014.07.937
Kercher KW, Matthews BD, Ponsky JL, Goldstein SL, Yavorski RT, Sing RF, Heniford BT (2001) Minimally invasive management of paraesophageal herniation in the high-risk surgical patient. Am J Surg 182:510–514
Yates RB, Hinojosa MW, Wright AS, Pellegrini CA, Oelschlager BK (2015) Laparoscopic gastropexy relieves symptoms of obstructed gastric volvulus in highoperative risk patients. Am J Surg 209:875–880. https://doi.org/10.1016/j.amjsurg.2014.12.024
Altorki NK, Yankelevitz D, Skinner DB (1998) Massive hiatal hernias: the anatomic basis of repair. J Thorac Cardiovasc Surg 115:828–835. https://doi.org/10.1016/S0022-5223(98)70363-0
Pierre AF, Luketich JD, Fernando HC, Christie NA, Buenaventura PO, Litle VR, Schauer PR, Pearson FG, Demeester SR (2002) Results of laparoscopic repair of giant paraesophageal hernias: 200 consecutive patients. Ann Thorac Surg 74:1909–1916. https://doi.org/10.1016/S0003-4975(02)04088-2
Antonoff MB, D’Cunha J, Andrade RS, Maddaus MA (2012) Giant paraesophageal hernia repair: technical pearls. J Thorac Cardiovasc Surg 144:S67–S70. https://doi.org/10.1016/j.jtcvs.2012.03.065
Mitiek MO, Andrade RS (2010) Giant hiatal hernia. Ann Thorac Surg 89:S2168–S2173. https://doi.org/10.1016/j.athoracsur.2010.03.022
Weitzendorfer M, Köhler G, Antoniou SA, Pallwein-Prettner L, Manzenreiter L, Schredl P, Emmanuel K, Koch OO (2017) Preoperative diagnosis of hiatal hernia: barium swallow X-ray, high-resolution manometry, or endoscopy? Eur Surg 49:210–217. https://doi.org/10.1007/s10353-017-0492-y
Batirel HF, Uygur-Bayramicli O, Giral A, Ekici B, Bekiroglu N, Yildizeli B, Yüksel M (2009) The size of the esophageal hiatus in gastroesophageal reflux pathophysiology: outcome of intraoperative measurements. J Gastrointest Surg 14:38–44. https://doi.org/10.1007/s11605-009-1047-8
Koch OO, Asche KU, Berger J, Weber E, Granderath FA, Pointner R (2011) Influence of the size of the hiatus on the rate of reherniation after laparoscopic fundoplication and refundopilication with mesh hiatoplasty. Surg Endosc 25:1024–1030. https://doi.org/10.1007/s00464-010-1308-3
Granderath FA (2007) Measurement of the esophageal hiatus by calculation of the hiatal surface area (HSA). Why, when and how? Surg Endosc 21:2224–2225. https://doi.org/10.1007/s00464-007-9348-z
Smith-Bindman R (2010) Is computed tomography safe? N Engl J Med 363:1–4. https://doi.org/10.1056/NEJMp1002530
Callen PW, Filly RA, Korobkin M (1978) Computed tomographic evaluation of the diaphragmatic crura. Radiology 126:413–416
Eren S, Çiriş F (2005) Diaphragmatic hernia: diagnostic approaches with review of the literature. Eur J Radiol 54:448–459. https://doi.org/10.1016/j.ejrad.2004.09.008
Sandstrom CK, Stern EJ (2011) Diaphragmatic hernias: a spectrum of radiographic appearances. Curr Probl Diagn Radiol 40:95–115. https://doi.org/10.1067/j.cpradiol.2009.11.001
Sodhi KS, Virmani V, Sandhu MS, Khandelwal N (2015) Multi detector CT imaging of abdominal and diaphragmatic hernias: pictorial essay. Indian J Surg 77:104–110. https://doi.org/10.1007/s12262-012-0736-9
Mastrangelo MJ, Stich J, Hoskins JD, Witzke W, George I, Garrison J, Nicholls M, Park AE (2002) Advancements in immersive virtual reality as a tool for preoperative planning for laparoscopic surgery. Stud Health Technol Inform 85:274–279
Kavic SM, Segan RD, George IM, Turner PL, Roth JS, Park A (2006) Classification of hiatal hernias using dynamic three-dimensional reconstruction. Surg Innov 13:49–52. https://doi.org/10.1177/155335060601300108
Ouyang W, Dass C, Zhao H, Kim C, Criner G (2016) Multiplanar MDCT measurement of esophageal hiatus surface area: association with hiatal hernia and GERD. Surg Endosc 30:2465–2472. https://doi.org/10.1007/s00464-015-4499-9
Koch OO, Schurich M, Antoniou SA, Spaun G, Kaindlstorfer A, Pointner R, Swanstrom LL (2014) Predictability of hiatal hernia/defect size: is there a correlation between pre- and intraoperative findings? Hernia 18:883–888. https://doi.org/10.1007/s10029-012-1033-z
Granderath FA, Schweiger UM, Pointner R (2007) Laparoscopic antireflux surgery: tailoring the hiatal closure to the size of hiatal surface area. Surg Endosc 21:542–548. https://doi.org/10.1007/s00464-006-9041-7
Grubnik VV, Malynovskyy AV (2013) Laparoscopic repair of hiatal hernias: new classification supported by long-term results. Surg Endosc 27:4337–4346. https://doi.org/10.1007/s00464-013-3069-2
Huntington TR (1997) Laparoscopic mesh repair of the esophageal hiatus. J Am Coll Surg 184:399–400
Oelschlager BK, Pellegrini CA, Hunter JG, Brunt ML, Soper NJ, Sheppard BC, Polissar NL, Neradilek MB, Mitsumori LM, Rohrmann CA, Swanstrom LL (2011) Biologic prosthesis to prevent recurrence after laparoscopic paraesophageal hernia repair: long-term follow-up from a multicenter, prospective, randomized trial. J Am Coll Surg 213:461–468. https://doi.org/10.1016/j.jamcollsurg.2011.05.017
Oelschlager BK, Pellegrini CA, Hunter J, Soper N, Brunt M, Sheppard B, Jobe B, Polissar N, Mitsumori L, Nelson J, Swanstrom L (2006) Biologic prosthesis reduces recurrence after laparoscopic paraesophageal hernia repair: a multicenter, prospective, randomized trial. Ann Surg 244:481–488. https://doi.org/10.1097/01.sla.0000237759.42831.03
Granderath FA, Granderath UM, Pointner R (2008) Laparoscopic revisional fundoplication with circular hiatal mesh prosthesis: the long-term results. World J Surg 32:999–1007. https://doi.org/10.1007/s00268-008-9558-0
Pfluke JM, Parker M, Bowers SP, Asbuni HJ, Daniel Smith C (2012) Use of mesh for hiatal hernia repair: a survey of SAGES members. Surg Endosc 26:1843–1848. https://doi.org/10.1007/s00464-012-2150-6
Funding
This research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Dr. Heniford is on the speaker’s bureau for Allergan and on the advisory committee for W.L. Gore. Dr. Augenstein has speaker’s fees for W.L. Gore, Allergan and is a consultant for Acelity and Intuitive. Dr. Colavita has speaker’s fees for Allergan. The remainder of the authors, Drs. Kao, Ross, Otero, Maloney, and Prasad have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kao, A.M., Ross, S.W., Otero, J. et al. Use of computed tomography volumetric measurements to predict operative techniques in paraesophageal hernia repair. Surg Endosc 34, 1785–1794 (2020). https://doi.org/10.1007/s00464-019-06930-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-019-06930-8