Abstract
Background
In Canada, bariatric surgery continues to remain the most effective treatment for severe obesity and its comorbidities. As the number of bariatric surgeries continues to grow, the need for consensus guidelines for optimal perioperative care is imperative. In colorectal surgery, enhanced recovery after surgery (ERAS) protocols were created for this purpose. The objective of this review is to develop evidence-based ERAS guidelines for bariatric surgery.
Methods
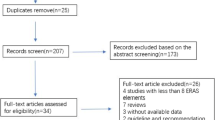
A literature search of the MEDLINE database was performed using ERAS-specific search terms. Recently published articles with a focus on randomized controlled trials, systematic reviews, and meta-analyses were included. Quality of evidence and recommendations were evaluated using the GRADE assessment system.
Results
Canadian bariatric surgeons from six provinces and ten bariatric centers performed a review of the evidence surrounding ERAS in bariatric surgery and created consensus guidelines for 14 essential ERAS elements. Our main recommendations were (1) to encourage participation in a presurgical weight loss program; (2) to abstain from tobacco and excessive alcohol; (3) low-calorie liquid diet for at least 2 weeks prior to surgery; (4) to avoid preanesthetic anxiolytics and long-acting opioids; (5) unfractionated or low-molecular-weight heparin prior to surgery; (6) antibiotic prophylaxis with cefazolin ± metronidazole; (7) reduced opioids during surgery; (8) surgeon preference regarding intraoperative leak testing; (9) nasogastric intubation needed only for Veress access; (10) to avoid abdominal drains and urinary catheters; (11) to prevent ileus by discontinuing intravenous fluids early; (12) postoperative analgesia with acetaminophen, short-term NSAIDS, and minimal opioids; (13) to resume full fluid diet on first postoperative day; (14) early telephone follow-up with full clinic follow-up at 3–4 weeks.
Conclusions
The purpose of addressing these ERAS elements is to develop guidelines that can be implemented and practiced clinically. ERAS is an excellent model that improves surgical efficiency and acts as a common perioperative pathway. In the interim, this multimodal bariatric perioperative guideline serves as a common consensus point for Canadian bariatric surgeons.
Similar content being viewed by others
References
Twells LK, Gregory DM, Reddigan J, Midodzi WK (2014) Current and predicted prevalence of obesity in Canada: a trend analysis. C Open 2:E18–E26. https://doi.org/10.9778/cmajo.20130016
Sjöström L (2013) Review of the key results from the Swedish obese subjects (SOS) trial—a prospective controlled intervention study of bariatric surgery. J Intern Med 273:219–234. https://doi.org/10.1111/joim.12012
Padwal RS, Chang H-J, Klarenbach S, Sharma AM, Majumdar SR (2012) Characteristics of the population eligible for and receiving publicly funded bariatric surgery in Canada. Int J Equity Health 11:54. https://doi.org/10.1186/1475-9276-11-54
Canadian Institute for Health Information (2014) Bariatric Surgery in Canada. Can Inst Heal Inf
Chang SH, Stoll CRT, Song J, Varela JE, Eagon CJ, Colditz GA (2014) The effectiveness and risks of bariatric surgery an updated systematic review and meta-analysis, 2003–2012. JAMA Surg 149:275–287. https://doi.org/10.1001/jamasurg.2013.3654
Chen SY, Stem M, Schweitzer MA, Magnuson TH, Lidor AO (2015) Assessment of postdischarge complications after bariatric surgery: a National surgical quality improvement Program analysis. Surgery 158:777–786. https://doi.org/10.1016/j.surg.2015.04.028
Muller S, Zalunardo MP, Hubner M, Clavien PA, Demartines N (2009) A fast-track program reduces complications and length of hospital stay after open colonic surgery. Gastroenterology 136:842–847.e1. https://doi.org/10.1053/j.gastro.2008.10.030
Šerclová Z, Dytrych P, Marvan J, Nová K, Hankeová Z, Ryska O, Šlégrová Z, Burešová L, Trávníková L, Antoš F (2009) Fast-track in open intestinal surgery: Prospective randomized study (Clinical Trials Gov Identifier no. NCT00123456). Clin Nutr 28:618–624. https://doi.org/10.1016/j.clnu.2009.05.009
Khoo CK, Vickery CJ, Forsyth N, Vinall NS, Eyre-Brook IA (2007) A prospective randomized controlled trial of multimodal perioperative management protocol in patients undergoing elective colorectal resection for cancer. Ann Surg 245:867–872. https://doi.org/10.1097/01.sla.0000259219.08209.36
Wind J, Hofland J, Preckel B, Hollmann MW, Bossuyt PMM, Gouma DJ, Van Berge Henegouwen MI, Fuhring JW, Dejong CHC, Van Dam RM, Cuesta MA, Noordhuis A, De Jong D, Van Zalingen E, Engel AF, Goei TH, De Stoppelaar IE, Van Tets WF, Van Wagensveld BA, Swart A, Van Den Elsen MJLJ, Gerhards MF, De Wit LT, Siepel MAM, Van Geloven AAW, Juttmann JW, Clevers W, Bemelman WA (2006) Perioperative strategy in colonic surgery; LAparoscopy and/or FAst track multimodal management versus standard care (LAFA trial). BMC Surg 6:1–8. https://doi.org/10.1186/1471-2482-6-16
Basse L, Raskov HH, Hjort Jakobsen D, Sonne E, Billesbølle P, Hendel HW, Rosenberg J, Kehlet H (2002) Accelerated postoperative recovery programme after colonic resection improves physical performance, pulmonary function and body composition. Br J Surg 89:446–453. https://doi.org/10.1046/j.0007-1323.2001.02044.x
Basse L, Jacobsen DH, Billesbolle P (2000) A clinical pathway to accelerated recovery afther colonic resection. Ann Surg 232:51
Thorell A, MacCormick AD, Awad S, Reynolds N, Roulin D, Demartines N, Vignaud M, Alvarez A, Singh PM, Lobo DN (2016) Guidelines for perioperative care in bariatric surgery: enhanced recovery after surgery (ERAS) society recommendations. World J Surg 40:2065–2083. https://doi.org/10.1007/s00268-016-3492-3
Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, Schünemann HJ (2009) GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. Br Med J 9:8–11. https://doi.org/10.1136/bmj.39489.470347.AD
Elliott JA, Patel VM, Kirresh A, Ashrafian H, Le Roux CW, Olbers T, Athanasiou T, Zacharakis E (2013) Fast-track laparoscopic bariatric surgery: a systematic review. Updates Surg 65:85–94. https://doi.org/10.1007/s13304-012-0195-7
Valkenet K, van de Port IGL, Dronkers JJ, De Vries WR, Lindeman E, Backx FJG (2011) The effects of preoperative exercise therapy on postoperative outcome: a systematic review. Clin Rehabil 25:99–111. https://doi.org/10.1177/0269215510380830
Lemanu DP, Singh PP, MacCormick AD, Arroll B, Hill AG (2013) Effect of preoperative exercise on cardiorespiratory function and recovery after surgery: a systematic review. World J Surg 37:711–720. https://doi.org/10.1007/s00268-012-1886-4
Buchwald H, Avidor Y, Braunwald E, Al E (2004) Bariatric surgery: a systematic review and meta-analysis. JAMA 292:1724–1737
Cassie S, Menezes C, Birch DW, Shi X, Karmali S (2011) Effect of preoperative weight loss in bariatric surgical patients: a systematic review. Surg Obes Relat Dis 7:760–767. https://doi.org/10.1016/j.soard.2011.08.011
Gerber P, Anderin C, Thorell A (2015) Weight loss prior to bariatric surgery: an updated review of the literature. Scand J Surg 104:33–39. https://doi.org/10.1177/1457496914553149
Anderin C, Gustafsson UO, Heijbel N, Thorell A (2015) Weight loss before bariatric surgery and postoperative complications: data from the scandinavian obesity registry (SOReg). Ann Surg 261:909–913. https://doi.org/10.1097/SLA.0000000000000839
Mills E, Eyawo O, Lockhart I, Kelly S, Wu P, Ebbert JO (2011) Smoking cessation reduces postoperative complications: a systematic review and meta-analysis. Am J Med 124:144–154. https://doi.org/10.1016/j.amjmed.2010.09.013
Spaniolas K, Yang J, Crowley S, Yin D, Docimo S, Bates AT, Pryor AD (2018) Association of long-term anastomotic ulceration after Roux-en-Y gastric bypass with tobacco smoking. JAMA Surg 153(9):20–22
Coblijn UK, Lagarde SM, de Castro SMM, Kuiken SD, van Wagensveld BA (2015) Symptomatic marginal ulcer disease after Roux-en-Y gastric bypass: incidence, risk factors and management. Obes Surg 25:805–811. https://doi.org/10.1007/s11695-014-1482-9
Paci E, Pigini D, Bauleo L, Ancona C, Forastiere F, Tranfo G (2018) Urinary cotinine concentration and self-reported smoking status in 1075 subjects living in central Italy. Int J Environ Res Public Health 15(4):804
Butt P, Beirness D, Gliksman L, Paradis C, Stockwell T (2011) Alcohol and health in Canada: A summary of evidence and guidelines for low-risk drinking
Nath B, Li Y, Carroll JE, Szabo G, Tseng JF, Shah SA (2010) Alcohol exposure as a risk factor for adverse outcomes in elective surgery. J Gastrointest Surg 14:1732–1741. https://doi.org/10.1007/s11605-010-1350-4
PleckaÖstlund M, Backman O, Marsk R, Stockeld D, Lagergren J, Rasmussen F, Nas̈lund E (2013) Increased admission for alcohol dependence after gastric bypass surgery compared with restrictive bariatric surgery. JAMA Surg 148:374–377. https://doi.org/10.1001/jamasurg.2013
Rummell CM, Heinberg LJ (2014) Assessing marijuana use in bariatric surgery candidates: should It be a contraindication? Obes Surg 24:1764–1770. https://doi.org/10.1007/s11695-014-1315-x
Raebel MA, Newcomer SR, Reifler LM, Boudreau D, Elliott TE, DeBar L, Ahmed A, Pawloski PA, Fisher D, Donahoo WT, Bayliss EA (2013) Chronic use of opioid medications before and after bariatric surgery. JAMA 310:1369–1376. https://doi.org/10.1001/jama.2013.278344
Scarborough JE, Mantyh CR, Sun Z, Migaly J (2015) Combined mechanical and oral antibiotic bowel preparation reduces incisional surgical site infection and anastomotic leak rates after elective colorectal resection: an analysis of colectomy-targeted ACS NSQIP. Ann Surg 262:331–337. https://doi.org/10.1097/SLA.0000000000001041
Walter J, Ley R (2011) The human gut microbiome: ecology and recent evolutionary changes. Annu Rev Microbiol 65:411–429. https://doi.org/10.1146/annurev-micro-090110-102830
van Wissen J, Bakker N, Doodeman HJ, Jansma EP, Bonjer HJ, Houdijk APJ (2016) Preoperative methods to reduce liver volume in bariatric surgery: a systematic review. Obes Surg 26:251–256. https://doi.org/10.1007/s11695-015-1769-5
Holderbaum M, Casagrande DS, Sussenbach S, Buss C (2018) Effects of very low calorie diets on liver size and weight loss in the preoperative period of bariatric surgery: a systematic review. Surg Obes Relat Dis 14:237–244. https://doi.org/10.1016/j.soard.2017.09.531
Van Nieuwenhove Y, Dambrauskas Z, Campillo-Soto A, Van Dielen F, Wiezer R, Janssen I, Kramer M, Thorell A (2011) Preoperative very low-calorie diet and operative outcome after laparoscopic gastric bypass: a randomized multicenter study. Arch Surg 146:1300–1305. https://doi.org/10.1001/archsurg.2011.273
Lambert E, Carey S (2016) Practice guideline recommendations on perioperative fasting: a systematic review. J Parenter Enter Nutr 40:1158–1165. https://doi.org/10.1177/0148607114567713
Scott MJ, Baldini G, Fearon KCH, Feldheiser A, Feldman LS, Gan TJ, Ljungqvist O (2015) Enhanced recovery after surgery (ERAS) for gastrointestinal surgery, part 1: pathophysiological considerations. Acta Anaesthesiol Scand 59(10):1212–1231
Feldheiser A, Aziz O, Baldini G, Cox BPBW, Fearon KCH, Feldman LS, Gan TJ (2015) Enhanced recovery after surgery (ERAS) for gastrointestinal surgery, part 2: consensus statement for anaesthesia practice. Acta Anaesthesiol scand 60(3):289–334
Izrailtyan I, Qiu J, Overdyk FJ, Erslon M, Gan TJ (2018) Risk factors for cardiopulmonary and respiratory arrest in medical and surgical hospital patients on opioid analgesics and sedatives. PLoS ONE 13(3):e0194553
Walker KJ, Smith AF (2009) Premedication for anxiety in adult day surgery (Review). Cochrane Database Syst Rev 7(4):CD002192
Mansour MA, Ahmed AA (2013) Nonopioid versus opioid based general anesthesia technique for bariatric surgery : a randomized double—blind study. Saudi J Anaesth 7(4):387
Srinivasa S, Kahokehr AA, Yu T (2011) Preoperative glucocorticoid use in major abdominal surgery. Ann Surg 254:183–191. https://doi.org/10.1097/SLA.0b013e3182261118
Rocha AT, Vasconcellos AG, Luz ER, No Araújo DM, Alves ES, Lopes AA (2006) Risk of venous thromboembolism and efficacy of thromboprophylaxis in hospitalized obese medical patients and in obese patients undergoing bariatric surgery. Obes Surg 16:1645–1655. https://doi.org/10.1381/096089206779319383
Overby DW, Kohn GP, Cahan MA, Galanko JA, Colton K, Moll S, Farrell TM (2009) Prevalence of thrombophilias in patients presenting for bariatric surgery. Obes Surg 19:1278–1285. https://doi.org/10.1007/s11695-009-9906-7
Critique SI (2012) Comparative effectiveness of unfractionated and low-molecular-weight heparin for prevention of venous thromboembolism following bariatric surgery. Arch Surg 147:994–998
Mismetti P, Laporte S, Darmon J-Y, Buchmuller A, Decousus H (2001) Meta-analysis of low molecular weight heparin in the prevention of venous thromboembolism in general surgery. Br J Surg 88:913–930. https://doi.org/10.1046/j.0007-1323.2001.01800.x
Dogan K, Kraaij L, Aarts EO, Koehestanie P, Hammink E (2015) Fast-track bariatric surgery improves perioperative care and logistics compared to conventional care. 25(1):28–35
Tanner J, Woodings D, Moncaster K (2008) Preoperative hair removal to reduce surgical site infection (Review). J Perioper Pract 18(6):232–243
Rabih O, Darouiche MD (2010) Chlorhexidine–alcohol versus povidone– iodine for surgical-site antisepsis. J Med 362(1):18–26
Chen X, Brathwaite CEM, Barkan A, Hall K, Chu G, Cherasard P, Wang S, Nicolau DP, Islam S, Cunha BA (2017) Optimal cefazolin prophylactic dosing for bariatric surgery : no need for higher doses or intraoperative redosing. 27(3):626–629
Bratzler DW, Houck PM, Infection S (2005) Antimicrobial prophylaxis for surgery: an advisory statement from the National Surgical Infection Prevention Project. Clin Infect Dis 189:395–404. https://doi.org/10.1016/j.amjsurg.2005.01.015
Willis AT, Fergusion IR, Jones PH, Phillips KD, Tearle PV, Fiddian RV, Graham DF, Harland DHC, Hughes DFR, Knight D, Mee WM, Pashby N, Sachdeva AK, Sutch I, Kilbey C (1977) Metronidazole in prevention and treatment of bacteroides infections in elective colonic surgery. Br Med J 6061(1):607–610
Tufanogullari B, White PF, Kianpour D, Lacour T, Griffin J, Skrivanek G (2008) Surgery : the effect on recovery outcome variables. Aneath Anal 106(6):1741–1748
Wool DB, Lemmens HJM, Brodsky JB, Solomon H, Chong KP, Morton JM (2010) intraoperative fluid replacement and postoperative creatine phosphokinase levels in laparoscopic bariatric patients. Obes Surg 20(6):698–701
Levy BF, Scott MJ, Fawcett W, Fry C, Rockall TA (2011) Randomized clinical trial of epidural, spinal or patient-controlled analgesia for patients undergoing laparoscopic colorectal surgery. Br J Surg 98(8):1068–1078
Kurz A, Sessler DI (1996) Perioperative normothermia to reduce the incidence of surgical-wound infection and shorten hospitalization. N Engl J Med 334(19):1209–1216
Birch DW, Dang JT, Switzer NJ, Manouchehri N, Shi X, Hadi G, Karmali S (2016) Heated insufflation with or without humidification for laparoscopic abdominal surgery. Cochr Database Syst Rev. https://doi.org/10.1002/14651858.cd007821.pub3
Sethi M, Zagzag J, Patel K, Magrath M, Somoza E, Parikh MS, Saunders JK, Bradley AU, Marina FS, Ren-fielding GAFCJ (2016) Intraoperative leak testing has no correlation with leak after laparoscopic sleeve gastrectomy. Surg Endosc 30:883–891. https://doi.org/10.1007/s00464-015-4286-7
Nimeri A, Ghabra S, Dehni N, Elamin D, Al Hadad M, Ibrahim M (2015) Intraoperative endoscopy decreases postoperative complications in laparoscopic Roux-en-y gastric bypass. Obes Surg 25:1711–1715. https://doi.org/10.1007/s11695-015-1604-z
Alaedeen D, Madan A, Ro CY, Khan KA, Martinez JMTD (2009) Intraoperative endoscopy and leaks after laparoscopic Roux-en-Y gastric bypass. Am Surg 75:485–488
Huerta S, Arteaga JR, Sawicki MP, Liu CD, Livingston EH, Angeles L, Nelson R, Tse B, Edwards S (2005) Assessment of routine elimination of postoperative nasogastric decompression after Roux-en- Y gastric bypass. Surgery 132(5):844–848
Nelson R, Tse B, Edwards S (2005) Systematic review of prophylactic nasogastric decompression after abdominal operations. J Surg Swiss Surg 92(6):673–680
Verma R, Rl N (2010) Prophylactic nasogastric decompression after abdominal surgery (Review). doi: 10.1002/14651858.CD004929.pub3.www.cochranelibrary.com
Agarwala N, Liu CY (2005) Safe entry techniques during laparoscopy : Left upper quadrant entry using the ninth intercostal space—a review of 918 procedures. J Mimim Invasive Gynecol 12(1):55–61
Dallal RM, Bailey L, Nahmias N (2007) Back to basics–clinical diagnosis in bariatric surgery. Routine drains and upper GI series are unnecessary. Surg Endosc 21(12):2268–2271
Rolph R, Jmn D, Alagaratnam S, Ng P, Novell R (2016) Intra-abdominal drains for the prophylaxis of anastomotic leak in elective colorectal surgery (Review). doi: 10.1002/14651858.CD002100.pub2.www.cochranelibrary.com
Radtka JF, Puleo FJ, Wang L, Cooney RN (2010) Revisional bariatric surgery: who, what, where, and when? Surg Obes Relat Dis 6:635–642. https://doi.org/10.1016/j.soard.2010.04.005
Tammela T, Kontturi M, Lukkarinen O (2009) Postoperative urinary retention : I. incidence and predisposing factors. Scand J Urol Nephrol 20(3):197–201
Ronellenfitsch U, Schwarzbach M (2012) The effect of clinical pathways for bariatric surgery on perioperative quality of care. Obes Surg 22(5):732–739
Hop WCJ, Kok NFM, Lim A, Brouwer KJ, Jeekel J (2007) Randomized clinical trial of the impact of early enteral feeding on postoperative ileus and recovery. J Surg Swiss Surg 94(5):555–561
Pearse R, Harrison DA, Macdonald N, Gillies MA, Blunt M, Ackland G, Grocott MPW, Ahern A, Griggs K, Scott R, Hinds C, Rowan K, Study O (2015) Effect of a perioperative, cardiac output–guided hemodynamic therapy algorithm on outcomes following major gastrointestinal surgery:a randomized clinical trial and systematic review. JAMA 311(21):2181–2190
Traut U, Brügger L, Kunz R, Haug K, Bucher H, Mt K, Traut U, Brügger L, Kunz R, Pauli-magnus C, Haug K, Bucher H, Koller MT (2009) Systemic prokinetic pharmacologic treatment for postoperative adynamic ileus following abdominal surgery in adults (Review) Systemic prokinetic pharmacologic treatment for postoperative adynamic ileus following abdominal surgery in adults. 4–6. https://doi.org/10.1002/14651858.cd004930.pub3.copyright
Wolff BG, Michelassi F, Gerkin TM, Techner L, Gabriel K, Du W, Wallin BA, Rothenberger DA, Van De Water JM, Dayton MT, Moody FG (2004) Alvimopan, a novel, peripherally acting μ opioid antagonist: results of a multicenter, randomized, double-blind, placebo-controlled, phase III trial of major abdominal surgery and postoperative ileus. Ann Surg 240:728–735
Delaney CP, Weese JL, Hyman NH, Bauer J, Techner L, Gabriel K, Du W, Schmidt WK, Wallin BA (2005) Phase III trial of alvimopan, a novel, peripherally acting, Mu opioid antagonist, for postoperative ileus after major abdominal surgery. Dis Colon Rectum 48:1114–1129. https://doi.org/10.1007/s10350-005-0035-7
Zingg U, Miskovic D, Pasternak I, Meyer P, Hamel CT, Metzger U (2008) Effect of bisacodyl on postoperative bowel motility in elective colorectal surgery: a prospective, randomized trial. Int J Colorectal Dis 23:1175–1183. https://doi.org/10.1007/s00384-008-0536-7
Hansen CT, Sørensen M, Møller C, Ottesen B, Kehlet H (2007) Effect of laxatives on gastrointestinal functional recovery in fast-track hysterectomy: a double-blind, placebo-controlled randomized study. Am J Obstet Gynecol 196:1–7. https://doi.org/10.1016/j.ajog.2006.10.902
Gustafsson UO, Scott MJ, Schwenk W, Demartines N, Roulin D, Francis N, McNaught CE, MacFie J, Liberman AS, Soop M, Hill A, Kennedy RH, Lobo DN, Fearon K, Ljungqvist O (2013) Guidelines for perioperative care in elective colonic surgery: enhanced recovery after surgery (ERAS®) society recommendations. World J Surg 37:259–284. https://doi.org/10.1007/s00268-012-1772-0
Delaney CP, Zutshi M, Senagore AJ, Remzi FH, Hammel J, Fazio VW (2003) Prospective, randomized, controlled trial between a pathway of controlled rehabilitation with early ambulation and diet and traditional postoperative care after laparotomy and intestinal resection. Dis Colon Rectum 46:851–859. https://doi.org/10.1007/s10350-004-6672-4
White P (2005) The changing role of non-opioid analgesic techniques in the management of postoperative pain. Anesth Analg 101(5S):S5–S22
Romsing J, Moiniche S, Dahl JB (2002) Rectal and parenteral paracetamol, and paracetamol in combination with NSAIDs, for postoperative analgesia. Br J Anaesth 88:215–226. https://doi.org/10.1093/bja/88.2.215
Gorissen KJ, Benning D, Berghmans T, Snoeijs MG, Sosef MN, Hulsewe KWE, Luyer MDP (2012) Risk of anastomotic leakage with non-steroidal anti-inflammatory drugs in colorectal surgery. Br J Surg 99:721–727. https://doi.org/10.1002/bjs.8691
Goudie TA, Allan MW, Lonsdale M, Burrow LM, Macrae WA, Grant IS (1985) Continuous subcutaneous infusion of morphine for postoperative pain relief. Anaesthesia 40:1086–1092
Rawal N, Amilon A (2001) Postoperative analgesia at home after ambulatory hand surgery: a controlled comparison of tramadol, metamizol and paracetamol. Anesth Analg 92(2):347–351
Henzi I, Walder B, Trame MR (2000) Dexamethasone for prevention of postoperative nausea and vomiting: a quantitative systematic review. Anesth Analg 1993:186–194
Lewis SJ, Andersen HK, Thomas S (2009) Early enteral nutrition within 24 h of intestinal surgery versus later commencement of feeding: a systematic review and meta-analysis. J Gastrointest Surg 13:569–575. https://doi.org/10.1007/s11605-008-0592-x
Lassen K, Kjæve J, Fetveit T, Tranø G, Sigurdsson HK, Horn A, Revhaug A (2008) Allowing normal food at will after major upper gastrointestinal surgery does not increase morbidity: a randomized multicenter trial. Ann Surg 247:721–729. https://doi.org/10.1097/SLA.0b013e31815cca68
Mattei P, Rombeau JL (2006) Review of the pathophysiology and management of postoperative ileus. World J Surg 30:1382–1391. https://doi.org/10.1007/s00268-005-0613-9
Acknowledgements
None.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
Jerry T. Dang, Vivian G. Szeto, Ahmad Elnahas, James Ellsmere, Allan Okrainec, Amy Neville, Samaad Malik, Ekua Yorke, Dennis Hong, Laurent Biertho, Timothy Jackson, and Shahzeer Karmali have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Dang, J.T., Szeto, V.G., Elnahas, A. et al. Canadian consensus statement: enhanced recovery after surgery in bariatric surgery. Surg Endosc 34, 1366–1375 (2020). https://doi.org/10.1007/s00464-019-06911-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-019-06911-x