Abstract
Introduction
Roux-En-Y gastric bypass (RYGB) is an alternative to reoperative fundoplication. The aim of this study was to expand long-term outcomes of patients undergoing RYGB after failed fundoplication and assess symptom resolution.
Methods
A single institution prospective study was performed of patients undergoing fundoplication takedown and RYGB between March 2007 and September 2016. Demographics, body mass index (BMI), preoperative symptoms, operative duration and findings, and postoperative outcomes were recorded. Data were assessed using standard statistical methods.
Results
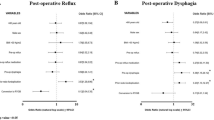
87 patients with failed antireflux surgery underwent RYGB. Median age 58 years (range 25–79 years). Median preoperative BMI 32.4 kg/m2 (range 21.6–50.6 kg/m2). Comorbidities included hypertension (48.3%) and diabetes (11.5%). Sixty-six patients had undergone 1 prior fundoplication, 18 had 2 prior fundoplications, and 3 had 3 prior fundoplications. At least one previous open antireflux procedure had been performed in 16.1% of patients. The most common recurrent symptoms were reflux (85.1%), dysphagia (36.7%), pain (35.6%), and regurgitation (29.9%). Median symptom-free interval from last antireflux surgery was 3 years (range 0–25 years). RYGB was performed laparoscopically in 47.1% of cases, robotically in 44.8% of cases, and open in 5.9%. Operative duration was longer in the robotic group (p = 0.04). During RYGB, 85.1% patients were found to have an associated hiatal hernia, 34.5% had intrathoracic migration of the fundoplication, 32.2% a slipped fundoplication onto proximal stomach, and 13.8% had wrap disruption. Median length of stay (LOS) was 4 days (range 1–33 days). Median follow-up was 35.8 months, 11 patients (12.6%) had recurrent reflux symptoms. Excess body weight loss (%EWL) was 80.4%. There was no mortality but 8 patients required reoperation during follow-up.
Conclusions
Fundoplication takedown with RYGB was successful for long-term reflux resolution. Most can be performed via a minimally invasive approach with acceptable perioperative morbidity, symptom resolution, and the additional benefit of %EWL.
Similar content being viewed by others
References
Richter JE (2003) The enormous burden of digestive diseases on our healthcare system. Curr Gastroenterol Rep 5(2):93–94
Quiroga E et al (2006) Impaired esophageal function in morbidly obese patients with gastroesophageal reflux disease: evaluation with multichannel intraluminal impedance. Surg Endosc 20(5):739–743
Fisher BL et al (1999) Obesity correlates with gastroesophageal reflux. Dig Dis Sci 44(11):2290–2294
Luketich JD et al (2002) Outcomes after minimally invasive reoperation for gastroesophageal reflux disease. Ann Thorac Surg 74(2):328–331 (discussion 331-2)
Aslam M et al (2012) Nonlinear relationship between body mass index and esophageal acid exposure in the extraesophageal manifestations of reflux. Clin Gastroenterol Hepatol 10(8):874–878
Colavita PD et al (2013) Nationwide inpatient sample: have antireflux procedures undergone regionalization? J Gastrointest Surg 17(1):6–13 (discussion p 13)
Cookson R et al (2005) Short-term cost effectiveness and long-term cost analysis comparing laparoscopic Nissen fundoplication with proton-pump inhibitor maintenance for gastro-oesophageal reflux disease. Br J Surg 92(6):700–706
Arguedas MR et al (2004) Re-examination of the cost-effectiveness of surgical versus medical therapy in patients with gastroesophageal reflux disease: the value of long-term data collection. Am J Gastroenterol 99(6):1023–1028
Houghton SG et al (2005) Is Roux-en-Y gastric bypass safe after previous antireflux surgery? Technical feasibility and postoperative symptom assessment. Surg Obes Relat Dis 1(5):475–480
Prachand VN, Alverdy JC (2010) Gastroesophageal reflux disease and severe obesity: fundoplication or bariatric surgery? World J Gastroenterol 16(30):3757–3761
Furnee EJ et al (2009) Surgical reintervention after failed antireflux surgery: a systematic review of the literature. J Gastrointest Surg 13(8):1539–1549
Dallemagne B et al (2011) Long-term results after laparoscopic reoperation for failed antireflux procedures. Br J Surg 98(11):1581–1587
Jafari MD et al (2013) Volume and outcome relationship in bariatric surgery in the laparoscopic era. Surg Endosc 27(12):4539–4546
Varban OA et al (2015) Hospital volume and outcomes for laparoscopic gastric bypass and adjustable gastric banding in the modern era. Surg Obes Relat Dis 11(2):343–349
Makris KI et al (2012) The role of short-limb Roux-en-Y reconstruction for failed antireflux surgery: a single-center 5-year experience. Surg Endosc 26(5):1279–1286
Patterson EJ et al (2003) Comparison of objective outcomes following laparoscopic Nissen fundoplication versus laparoscopic gastric bypass in the morbidly obese with heartburn. Surg Endosc 17(10):1561–1565
Nguyen SQ et al (2009) Laparoscopic Roux-en-Y gastric bypass after previous Nissen fundoplication. Surg Obes Relat Dis 5(2):280–282
Jones KB Jr et al (1991) Roux-Y Gastric Bypass: an effective anti-reflux procedure. Obes Surg 1(3):295–298
Stefanidis D et al (2012) Laparoscopic fundoplication takedown with conversion to Roux-en-Y gastric bypass leads to excellent reflux control and quality of life after fundoplication failure. Surg Endosc 26(12):3521–3527
Kim M et al (2014) Minimally invasive Roux-en-Y gastric bypass for fundoplication failure offers excellent gastroesophageal reflux control. Am Surg 80(7):696–703
Khajanchee YS et al (2007) Laparoscopic reintervention for failed antireflux surgery: subjective and objective outcomes in 176 consecutive patients. Arch Surg 142(8):785–901 (discussion 791-2).
Mittal SK et al (2013) Roux-en-Y reconstruction is superior to redo fundoplication in a subset of patients with failed antireflux surgery. Surg Endosc 27(3):927–935
Makris KI, Lee T, Mittal SK (2009) Roux-en-Y reconstruction for failed fundoplication. J Gastrointest Surg 13(12):2226–2232
Furnee EJ et al (2008) Surgical reintervention after antireflux surgery for gastroesophageal reflux disease: a prospective cohort study in 130 patients. Arch Surg 143(3):267–274 (discussion 274).
Oelschlager BK et al (2006) Medium- and long-term outcome of laparoscopic redo fundoplication. Surg Endosc 20(12):1817–1823
Lo Menzo E, Stevens N, Kligman M (2011) Laparoscopic revision of gastrojejunostomy and vagotomy for intractable marginal ulcer after revised gastric bypass. Surg Obes Relat Dis 7(5):656–658
Yamamoto SR et al (2014) Long-term outcomes of reintervention for failed fundoplication: redo fundoplication versus Roux-en-Y reconstruction. Surg Endosc 28(1):42–48
Anderson JE et al (2012) The first national examination of outcomes and trends in robotic surgery in the United States. J Am Coll Surg 215(1):107–114 (discussion 114-6).
Ballantyne GH (2002) Robotic surgery, telerobotic surgery, telepresence, and telementoring. Review of early clinical results. Surg Endosc 16(10):1389–1402
Markar SR et al (2011) Robotic vs. laparoscopic Roux-en-Y gastric bypass in morbidly obese patients: systematic review and pooled analysis. Int J Med Robot 7(4):393–400
Hagen ME et al (2012) Reducing cost of surgery by avoiding complications: the model of robotic Roux-en-Y gastric bypass. Obes Surg 22(1):52–61
Akimoto S et al (2015) Association of body mass index (BMI) with patterns of fundoplication failure: insights gained. J Gastrointest Surg 19(11):1943–1948
Ghosh SK et al (2005) The mechanical basis of impaired esophageal emptying postfundoplication. Am J Physiol Gastrointest Liver Physiol 289(1):G21–G35
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Dr. Heniford and Dr. Augenstein have been awarded surgical research and education grants from W.L. Gore and Associates, Ethicon, and LifeCell Inc. Dr. Colavita has received honoraria for speaking from W.L. Gore and Associates. Dr. Gersin has received honoraria for speaking from GI Dynamics, W.L. Gore and Mallinckrodt. Dr. Stefanidis, Dr. Coakley, Dr. Groene, Dr. Lincourt and Ms. Prasad have no conflicts of interest or financial ties to disclose.
Rights and permissions
About this article
Cite this article
Coakley, K.M., Groene, S.A., Colavita, P.D. et al. Roux-En-Y gastric bypass following failed fundoplication. Surg Endosc 32, 3517–3524 (2018). https://doi.org/10.1007/s00464-018-6072-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-018-6072-9