Abstract
Background
In colon cancer, T4 stage is still assumed to be a relative contraindication for laparoscopic surgery considering the oncological safety. The aim of this systematic review with meta-analysis was to evaluate short- and long-term oncological outcomes after laparoscopic surgery for T4 colon cancer, and to compare these with open surgery.
Methods
Using systematic review of literature, studies reporting on radicality of resection, disease-free survival (DFS), and/or overall survival (OS) after laparoscopic surgery for T4 colon cancer were identified, with or without a control group of open surgery. Pooled proportions and risk ratios were calculated using an inverse variance method.
Results
Thirteen observational cohort studies published between 2012 and 2017 were included, together consisting of 1217 patients that received laparoscopic surgery and 1357 with an open procedure. The proportion of multivisceral resections was larger in the open group in five studies. Based on 11 studies, the pooled proportion of R0 resection was 0.96 (95% CI: 0.91–0.99) and 0.96 (95% CI: 0.90–0.98) after laparoscopic and open surgery, respectively. Analysing (mainly) T4a subgroups in 6 evaluable studies revealed pooled R0 resection rates of 0.94 in both groups. No significant differences were found between laparoscopic and open surgery for any survival measure: RR 1.07 (95% CI: 0.96–1.20) for 3-year DFS, RR 1.04 (95% CI: 0.95–1.15) for 5-year DFS, RR 1.07 (95% CI: 0.99–1.14) for 3-year OS, and RR 1.05 (95% CI: 0.98–1.12) for 5-year OS.
Conclusion
Literature on laparoscopic surgery for T4 colon cancer is restricted to non-randomized comparisons with substantial allocation bias. Laparoscopic surgery for T4a tumours might be safe, whereas for T4b colon cancer requiring multivisceral resection it should be applied with caution.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Colon cancer is world-wide a highly prevalent disease [1] and approximately 15% of patients presents with a locally advanced tumour (T4 stage). Resection of T4 colon cancer can be challenging if it directly invades other organs or structures (T4b according to TNM7). This requires a multivisceral resection (MVR) that is conventionally performed using an open approach, but reports on laparoscopic MVRs are increasing.
Laparoscopic surgery for colon cancer was introduced in the late nineties. Several randomized trials showed the short-term benefits of laparoscopic colectomy as compared to open surgery [2,3,4,5]. A recent systematic review reported also long-term benefits, with lower risks of adhesion-related small bowel obstruction and incisional hernia [6]. In the multicentre randomized COLOR trial [7], the non-inferiority of laparoscopic surgery for colon cancer in terms of 3-year disease-free survival (3y DFS) was suggested. However, clinically suspected tumour invasion of adjacent structures (cT4b stage) was an exclusion criterion in the COLOR trial. With a reported conversion rate of up to 50% for the remaining T4 tumours, they proposed that an open approach could be more appropriate for T4 colon cancer.
Laparoscopic colectomy for colon cancer has become widely accepted and implemented in routine practice, but T4 stage still constitutes a relative contraindication for laparoscopic surgery. A laparoscopic approach might jeopardize radicality of the resection, with its impact on long-term oncological outcome [8]. The aim of this study was to systematically review the currently available literature on laparoscopic surgery for T4 colon cancer, with regard to short- and long-term oncological outcomes, and to compare these with open surgery.
Methods
Literature search
A systematic search was performed on the 21st of February 2017. Studies describing laparoscopic surgery for T4 colon cancer were identified using MEDLINE, EMBASE, and PubMed using the search terms as provided in Supplementary Table 1. The review protocol was developed according to the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines [9]. Two researchers independently screened titles and abstracts to select articles for full-text reading. In case of disagreement, discussion took place until consensus was reached. Relevant review articles and bibliographies of included studies were reviewed for additional relevant publications. No restrictions with respect to publication date were applied. Subsequently, two researchers performed full-text reading for the definitive selection of articles.
Study selection and quality assessment
Articles were considered eligible if containing original data on laparoscopic resection of T4 colon cancer. T4 stage referred to either clinical or pathological stage. If studies included both colon and rectal cancer without separate data on outcome measures, authors were contacted to provide data for the relevant subgroup. If these were not available, studies were excluded. Furthermore, all authors were contacted to provide separate outcome data for the pT4a and pT4b subgroups.
Radicality of resection, postoperative morbidity and long-term oncological survival outcomes were considered the main study outcomes. Studies that did not report on at least one of the main outcome measures were excluded. Both comparative (laparoscopic versus open surgery) and non-comparative studies were eligible. Case reports and studies with less than 10 patients were excluded. The quality of the included articles was independently assessed by two authors using the nine-point Newcastle–Ottawa Scale [10].
Data extraction
General study characteristics (i.e. study design, in/exclusion criteria), baseline patient and tumour characteristics, operative characteristics (setting, need for conversion, MVR), and data on multimodality treatment (i.e. systemic therapy) were extracted from the included studies. Outcome measures included postoperative complications (<30 days, not further predefined), postoperative mortality, radicality of resection, disease-free survival (DFS), and overall survival (OS). In case of comparative studies, relevant data were also extracted for the subgroup that received open surgery for T4 colon cancer. If available, data on oncological outcomes were retrieved for T4a and T4b stages separately. Data extraction was performed by two researchers independently.
Statistical analyses
Pooled averages were calculated for perioperative outcome measures. Pooled proportions with 95% confidence intervals (95%CI) were calculated using an inverse variance method (random effects model) in RStudio version 3.2.3 (R Foundation for Statistical Computing, Vienna, Austria 2016). For the purpose of comparing laparoscopic with open surgery, risk ratios were calculated with corresponding 95% confidence intervals (CI) using an inverse variance method (random effects model). The I 2 statistic was calculated in order to evaluate heterogeneity of the included studies. Meta-analyses were performed using Review Manager 5.3 (The Nordic Cochrane Centre, The Cochrane Collaboration, Copenhagen, Denmark 2014). A p value of less than 0.05 was considered statistically significant.
Results
Included studies
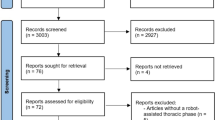
A total of 2689 hits were identified by searching MEDLINE, EMBASE, and Pubmed. The further selection process is displayed in Supplementary Fig. 1 and led to 56 articles eligible for full-text reading. Finally, 13 studies (23%) were included, all published between 2012 and 2017 (Table 1) [11,12,13,14,15,16,17,18,19,20,21,22,23]. There were no randomized controlled trials. Twelve studies were comparative observational cohort studies, including three studies applying matching or weighting. De’Angelis [11] used propensity score matching including the following variables in the regression model: age, sex, ASA score, surgical procedure, tumour location, tumoural and nodal stage, tumour size, MVR, and year of surgery. Elnahas [13] used inverse probability of treatment weighting (IPTW) creating a propensity score that represents the probability a patient was approached with laparoscopic resection, including age, sex, BMI, high ASA (>2), renal failure, chronic obstructive pulmonary disease (COPD), congestive heart failure (CHF), bleeding disorder, preoperative chemotherapy, metastasis, nodal disease, rectosigmoid resection, and emergency cases. Vignali [22] performed a case-matched control study and matched for disease stage (II/III/IV), ASA score, year of surgery (±3 years), and sex.
Three multicentre studies were included and ten single-centre studies. All studies together comprised 1217 patients that received laparoscopic surgery and 1357 that underwent open surgery. In all studies, converted patients were included in the laparoscopic group as intention to treat principle. After contacting the authors of combined colon and rectal cancer series, four studies provided separate data of T4 colon cancer [18, 21, 23, 24]. Regarding pathological versus clinical staging, ten studies included only patients with pT4 stage and inclusion was based on cT4 stage in three studies, with confirmation of pT4 by the pathologist in 77, 38, and 50%. Regarding pathological subgroups of pT4, one study included only pT4a stage [13], and in nine other studies, mainly (>60%) pT4a patients were included [11, 14, 17,18,19, 21,22,23, 25]. In two studies, MVR was the main focus, resulting in mostly pT4b stage [16, 20]. In eight studies, patients with metastatic disease were excluded. Emergency procedures were included in five studies [13,14,15, 18, 19], excluded in six other studies [11, 12, 16, 21,22,23], and not mentioned in the two remaining studies [17, 20].
Using the Newcastle–Ottawa Scale, two studies scored 9 out of 9 points, one study 8, three studies 7, five studies 6, and two studies were awarded 5 points (Supplementary Table 2).
Patient, disease, and treatment characteristics
Patient and disease characteristics are displayed in Table 2 for the laparoscopic and open subgroups separately. In Supplementary Table 3, data on operative characteristics are displayed. Conversion rates varied from 5.6 to 23%, with a pooled proportion of 0.11 (95% CI:0.09–0.14). In six of the eight comparative studies that also included MVR [11, 14, 15, 17, 19, 22], the proportion of MVR was higher in the open subgroups and the remaining two comparative studies included 100% MVR [20, 24].
Postoperative complication rates were described in 11 of the 13 studies, without clear definitions. Postoperative (30-day, early) complication rates ranged from 7.7 to 30% in laparoscopic groups and from 21 to 49% in the open cohorts, mainly including anastomotic leakage, (intra-abdominal) abscess, ileus, urinary tract infection, and wound infection. Pooled proportion of postoperative complications was 0.23 (95% CI: 0.19–0.27) for laparoscopy, and 0.35 (95% CI: 0.31–0.40) for open surgery (Table 4). Pooled postoperative mortality rates were 0.02 (95% CI: 0.01–0.04) and 0.03 (95% CI: 0.02–0.06), respectively. Meta-analysis of comparative studies reporting on postoperative complications revealed a risk ratio for laparoscopic versus open surgery of 0.65 for postoperative complications [95% CI: 0.55–0.77; p < 0.001, (heterogeneity: I 2 0%, p = 0.51)].
Adjuvant chemotherapy was applied in 55–100% of patients after laparoscopic surgery and in 37–80% after open resection. Time to adjuvant chemotherapy was only reported in one study [15]; 34 days (SD9) in the laparoscopic group versus 36 (SD21) days after open resection (p = 0.510).
Oncological outcomes
Eleven studies reported on radicality of resection (R0). Proportions of radical resections varied from 74 to 100% for laparoscopic surgery and from 76 to 100% in the open group (Table 3). Pooled proportions were 0.96 (95% CI: 0.91–0.99) and 0.96 (95% CI: 0.90–0.98), respectively (Table 4). Meta-analysis revealed no significant difference in radicality of resection between laparoscopic and open surgery (RR: 1.00 (95% CI: 0.98–1.01), p = 0.80) (Supplementary Fig. 2).
Endpoints used for long-term outcomes varied amongst the studies (Table 3). The pooled proportions are displayed in Table 4. Using meta-analysis, no statistically significant differences were found between laparoscopic and open surgery for any survival measure: RR 1.07 (95% CI: 0.96–1.20) for 3-year DFS, RR 1.04 (95% CI: 0.95–1.15) for 5-year DFS, RR 1.07 (95% CI: 0.99–1.14) for 3-year OS, and RR 1.05 (95% CI: 0.98–1.12) for 5-year OS (Supplementary Table 4).
For subgroup analyses of T4a stage, seven studies were selected of which six provided separate data for pT4a [11, 13, 16, 18, 21, 22] and in one additional study, pT4a was included in >80% in both the open and laparoscopic groups [15]. Pooled proportions of R0 resection of these studies were 0.94 (95% CI: 0.81–0.98) and 0.94 (95% CI: 0.82–0.98) after laparoscopic and open surgery, respectively (RR 1.00, 95% CI: 0.97–1.02, p = 0.75 (I 2 = 0%, p = 0.99), 6 studies). Furthermore, no significant difference was found for any survival measure: RR 1.09 (95% CI: 0.93–1.29, 3 studies) for 3-year DFS, RR 1.03 (95% CI: 0.82–1.31, 2 studies) for 5-year DFS, RR 1.11 (95% CI: 1.00–1.25, 3 studies) for 3-year OS, and RR 0.98 (95% CI: 0.83–1.173, 3 studies) for 5-year OS.
Considering T4b stage, five studies provided separate data (Table 3). Pooled proportions of R0 resection of these studies were 0.91 (95% CI: 0.80–0.96) and 0.93 (95% CI: 0.80–0.98) after laparoscopic and open surgery, respectively (RR 0.99, 95% CI: 0.92–1.05, p = 0.68 (I 2 = 0%, p = 0.69), 4 studies). Although in favour of open surgery, no significant differences were found for any survival measure: RR 0.91 (95% CI: 0.62–1.34, 1 study) for 3-year DFS, RR 0.91 (95% CI: 0.0.58–1.42, 1 study) for 5-year DFS, RR 0.85 (95% CI: 0.63–1.15, 1 study) for 3-year OS, and RR 0.96 (95% CI: 0.69–1.35, 2 studies) for 5-year OS.
Discussion
This systematic review of the literature revealed that only observational cohort studies on laparoscopic surgery for T4 colon cancer have been published. The open groups more often included MVRs, and six studies including both pT4a and pT4b stages provided separate outcome data. The pooled proportion of radical resection was 96% for both laparoscopic and open surgery. Analysing evaluable studies for different pT4 stages revealed pooled R0 resection rates for pT4a of 94% in both the laparoscopic and open groups. For pT4b, pooled R0 resection rates were 0.91 and 0.93. Available long-term oncological outcome measures in comparative studies did not show any significant differences between laparoscopic and open surgery for locally advanced colon cancer in both overall, T4a and T4b subgroup analyses.
Given the non-randomized design of the comparative studies, it should be noted that the approach of surgery (laparoscopic or open) has been chosen by the surgeon for specific reasons and with several influencing factors. Criteria on which this decision was made are often hard to determine retrospectively. In general, a laparoscopic approach for T4 colon cancer is used in patients with less extensive tumours requiring less complex procedures. This is confirmed by the comparative studies including MVR, showing a lower proportion of MVR in the laparoscopic groups compared to the open groups. The surgeon’s experience in minimally invasive surgery is crucial, and the laparoscopic and open resections from one institute might have been performed by different surgeons. Furthermore, when there is only peritoneal penetration (T4a), T4 stage is often diagnosed postoperatively, having less influence on the choice of the surgical approach. Achieving an R0 resection of T4a tumours is comparable to T3 tumours, because serosal ingrowth does not threaten margins. T4b tumours invade adjacent structures and require more complex (multivisceral) surgery [26, 27]. Inequality in distribution of T4a and T4b stages between the laparoscopic and open groups may significantly influence the results of comparative studies. In six of the included comparative studies, the proportion of T4b was substantially higher in the open group [14, 15, 17,18,19,20]. To overcome these methodological problems, Elnahas et al. excluded T4b stage [13] and Nagasue selected only MVR [24]. Furthermore, three studies applied matching or weighing in order to correct for baseline differences between the two surgical approaches. Only De’Angelis et al. [11] matched for T4a/b stage.
Considering the fact that laparoscopic surgery was likely being performed in more ‘favourable’ T4 colon cancers, one might argue that the pooled 96% radicality of resection should actually be considered worse compared to the similar radicality after open resection of more high-risk T4 cancers. Also the comparable survival probabilities should be interpreted with this allocation bias kept in mind. Selecting (mainly) T4a tumours allows for a more reliable comparison between the surgical approaches. The similar R0 resection rates for laparoscopic and open surgery in this subgroup analysis suggest that laparoscopic surgery for T4a stage is safe. The oncological safety of a minimally invasive multivisceral resection is, however, not clear based on the present data. The pooled radical resection rate after laparoscopic surgery for exclusively T4b stage was only 91%. Allocation bias may particularly play a crucial role in these tumours that invade surrounding organs by probably selecting, for example, a (limited) abdominal wall resection for a laparoscopic approach, whereas extensive multiorgan resections are often performed using open surgery. Future prospective studies differentiating between limited and extensive T4b tumours should point out the suitability of laparoscopic surgery for (part of) the T4b subgroup.
The risk of developing a postoperative complication was significantly lower after laparoscopic surgery as compared to open surgery (RR 0.65; 95% CI: 0.55–0.77, p < 0.001). However, in five out of ten comparative studies reporting on postoperative complications, substantially more MVRs were performed in the open group as compared to the laparoscopic group (Supplementary Table 3) [14, 15, 17, 19, 22]. A MVR is accompanied by more postoperative complications than just a segmental colectomy [26, 27]. The benefit of a laparoscopic approach for MVR might be limited, especially considering the fact that often large extraction incisions have to be made to remove the relatively large MVR specimens. Furthermore, in the open subgroups of three studies [15, 18, 19], significantly higher proportions of emergency procedures were included, with its impact on postoperative complications [28].
The influence of expertise on oncological outcomes is suggested based on a wide range in reported R0 resection rates of 74–100%. The study of Elnahas et al. [13] was a multi-institutional cohort study and used data from a (bi)nationwide database, showing overall R0 resection rates of 75%. Information on surgical experience and hospital volume was not provided, but the nationwide character of the study suggests a substantial contribution of non-expert centres. Potentially, centralization of care contributes to better R0 resection rates.
This systematic review has several limitations. An important limitation is the relatively low quality of evidence of the included studies as already discussed. Only three multicentre studies were included, suggesting publication bias of single-centre studies originating from expert centres. Furthermore, substantial heterogeneity between the studies exists because of the different patient populations assessed with regard to definition of T4 (clinical T4 versus pathological T4, T4a versus T4b). Duration of follow-up was relatively short, with two studies reporting on 3-year oncological outcomes [15, 29], while median follow-up was only 27 and 32 months, respectively. Also, with conversion rates of up to 23%, the intention to treat analysis might muddle the reported outcomes.
In conclusion, current literature does not provide the definitive answer on oncological safety of minimally invasive surgery for locally advanced colon cancer. Based on subgroup analysis, we cautiously conclude that laparoscopic surgery for T4a tumours might be safe, whereas it seems less appropriate for T4b tumours requiring multivisceral resection. Laparoscopic resection of T4 colon cancer should probably only be performed in selected patients by experienced surgeons. These selection criteria and level of experience have to be defined more precisely in future studies.
References
Ferlay J, Soerjomataram II, Dikshit R, Eser S, Mathers C, Rebelo M, Parkin DM, Forman DD, Bray F (2014) Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer 136:E359–E386. doi:10.1002/ijc.29210
Nelson H, Sargent DWH (2004) A comparison of laparoscopically assisted and open colectomy for colon cancer. N Engl J Med 350:2050–2059. doi:10.1016/j.ctrv.2004.09.001
Guillou PJ, Quirke P, Thorpe H, Walker J, Jayne DG, Smith AM, Heath RM, Brown JM (2005) Short-term endpoints of conventional versus laparoscopic-assisted surgery in patients with colorectal cancer (MRC CLASICC trial): multicentre, randomised controlled trial. Lancet 365:1718–1726. doi:10.1016/S0140-6736(05)66545-2
Lacy AM, García-Valdecasas JC, Delgado S, Castells A, Taurá P, Piqué JM, Visa J (2002) Laparoscopy-assisted colectomy versus open colectomy for treatment of non-metastatic colon cancer: a randomised trial. Lancet 359:2224–2229. doi:10.1016/S0140-6736(02)09290-5
Veldkamp R, Kuhry E, Hop WC, Jeekel J, Kazemier G, Bonjer HJ, Haglind E, Påhlman L, Cuesta MA, Msika S, Morino M, Lacy AM, COlon cancer Laparoscopic or Open Resection Study Group (COLOR) (2005) Laparoscopic surgery versus open surgery for colon cancer: short-term outcomes of a randomised trial. Lancet Oncol 6:477–484. doi:10.1016/S1470-2045(05)70221-7
Pecorelli N, Greco M, Amodeo S, Braga M (2016) Small bowel obstruction and incisional hernia after laparoscopic and open colorectal surgery: a meta-analysis of comparative trials. Surg Endosc. doi:10.1007/s00464-016-4995-6
Colon Cancer Laparoscopic or Open Resection Study Group, Buunen M, Veldkamp R, Hop WC, Kuhry E, Jeekel J, Haglind E, Påhlman L, Cuesta MA, Msika S, Morino M, Lacy A, Bonjer HJ (2009) Survival after laparoscopic surgery versus open surgery for colon cancer: long-term outcome of a randomised clinical trial. Lancet Oncol 10:44–52. doi:10.1016/S1470-2045(08)70310-3
Amri R, Bordeianou LG, Sylla P, Berger DL (2015) Association of radial margin positivity with colon cancer. JAMA Surg 150:890–898. doi:10.1001/jamasurg.2015.1525
Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, Shekelle P, Stewart LA, PRISMA-P Group (2015) Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev 4:1. doi:10.1186/2046-4053-4-1
Wells G, Shea B, O’Connell D, Peterson J, Welch V, Losos M, Tugwell P (2009) The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Accessed 1 Aug 2016
de’ Angelis N, Vitali GC, Brunetti F, Wassmer C-H, Gagniere C, Puppa G, Tournigand C, Ris F (2016) Laparoscopic vs. open surgery for T4 colon cancer: a propensity score analysis. Int J Colorectal Dis. doi:10.1007/s00384-016-2646-y
Chan DKH, Tan K-K (2016) Laparoscopic surgery should be considered in T4 colon cancer. Int J Colorectal Dis. doi:10.1007/s00384-016-2702-7
Elnahas A, Sunil S, Jackson TD, Okrainec A, Quereshy FA (2015) Laparoscopic versus open surgery for T4 colon cancer: evaluation of margin status. Surg Endosc. doi:10.1007/s00464-015-4360-1
Kang J, Baik SH, Lee KY, Sohn S-K (2016) Outcomes of laparoscopic surgery in pathologic T4 colon cancers compared to those of open surgery. Int J Colorectal Dis. doi:10.1007/s00384-016-2720-5
Kim IY, Kim BR, Kim YW (2015) The short-term and oncologic outcomes of laparoscopic versus open surgery for T4 colon cancer. Surg Endosc. doi:10.1007/s00464-015-4364-x
Nagasue Y, Akiyoshi T, Ueno M, Fukunaga Y, Nagayama S, Fujimoto Y, Konishi T, Nagasaki T, Nagata J, Mukai T, Ikeda A, Ono R, Yamaguchi T (2013) Laparoscopic versus open multivisceral resection for primary colorectal cancer: comparison of perioperative outcomes. J Gastrointest Surg 17:1299–1305. doi:10.1007/s11605-013-2222-5
Park JS, Huh JW, Park YA, Cho YB, Yun SH, Kim HC, Lee WY, Chun H-K, Lacy A, Garcia-Valdecasas J, Delgado S, Castells A, Taura P, Pique J, Guillou P, Quirke P, Thorpe H, Walker J, Jayne D, Smith A, Veldkamp R, Kuhry E, Hop W, Jeekel J, Kazemier G, Bonjer H, Chang G, Kaiser A, Mills S, Rafferty J, Buie W, Monson J, Weiser M, Buie W, Chang G, Rafferty J, Buie W, Zerey M, Hawver L, Awad Z, Stefanidis D, Richardson W, Fanelli R, Bretagnol F, Dedieu A, Zappa M, Guedj N, Ferron M, Panis Y, Hemandas A, Abdelrahman T, Flashman K, Skull A, Senapati A, O’Leary D, Kim K, Hwang D, Park Y, Lee H, Huh J, Kim H, Vignali A, Ghirardelli L, Palo S, Orsenigo E, Staudacher C, Nagasue Y, Akiyoshi T, Ueno M, Fukunaga Y, Nagayama S, Fujimoto Y, Ng D, Co C, Cheung H, Chung C, Li M, Park I, Choi G, Lim K, Kang B, Jun S, Agha A, Furst A, Iesalnieks I, Fichtner-Feigl S, Ghali N, Krenz D, Benson A, Bekaii-Saab T, Chan E, Chen Y, Choti M, Cooper H, Huh J, Park Y, Jung E, Lee K, Sohn S, Dighe S, Swift I, Brown G, Huh J, Jeong Y, Kim H, Kim Y (2016) Clinically suspected T4 colorectal cancer may be resected using a laparoscopic approach. BMC Cancer 16:714. doi:10.1186/s12885-016-2753-8
Sammour T, Jones IT, Gibbs P, Chandra R, Steel MC, Shedda SM, Croxford M, Faragher I, Hayes IP, Hastie IA (2015) Comparing oncological outcomes of laparoscopic versus open surgery for colon cancer: analysis of a large prospective clinical database. J Surg Oncol 111:891–898. doi:10.1002/jso.23893
Shukla PJ, Trencheva K, Merchant C, Maggiori L, Michelassi F, Sonoda T, Lee SW, Milsom JW (2015) Laparoscopic resection of T4 colon cancers: is it feasible? Dis Colon Rectum 58:25–31. doi:10.1097/DCR.0000000000000220
Takahashi R, Hasegawa S, Hirai K, Hisamori S, Hida K, Kawada K, Sakai Y (2017) Safety and feasibility of laparoscopic multivisceral resection for surgical T4b colon cancers: retrospective analyses. Asian J Endosc Surg. doi:10.1111/ases.12355
Vallribera Valls F, Filippo Landi B, Eloy Espín Basany B, José Luis Sánchez García B, Luis Miguel Jiménez Gómez B, Marc Martí Gallostra B, Luis Salgado Cruz B, Manuel Armengol Carrasco B (2014) Laparoscopy-assisted versus open colectomy for treatment of colon cancer in the elderly: morbidity and mortality outcomes in 545 patients. Surg Endosc. doi:10.1007/s00464-014-3597-4
Vignali A, Ghirardelli L, Di Palo S, Orsenigo E, Staudacher C (2013) Laparoscopic treatment of advanced colonic cancer: a case-matched control with open surgery. Colorectal Dis 15:944–948. doi:10.1111/codi.12170
Allaix ME, Degiuli M, Arezzo A, Arolfo S, Morino M (2013) Does conversion affect short-term and oncologic outcomes after laparoscopy for colorectal cancer? Surg Endosc 27:4596–4607. doi:10.1007/s00464-013-3072-7
Nagasue Y, Akiyoshi T, Ueno M, Fukunaga Y, Nagayama S, Fujimoto Y, Konishi T, Nagasaki T, Nagata J, Mukai T, Ikeda A, Ono R, Yamaguchi T (2013) Laparoscopic versus open multivisceral resection for primary colorectal cancer: comparison of perioperative outcomes. J Gastrointest Surg 17:1299–1305. doi:10.1007/s11605-013-2222-5
Shen P, Levine EA, Hall J, Case D, Russell G, Fleming R, McQuellon R, Geisinger KR, Loggie BW (2003) Factors predicting survival after intraperitoneal hyperthermic chemotherapy with mitomycin C after cytoreductive surgery for patients with peritoneal carcinomatosis. Arch Surg 138:26–33
Mohan HM, Evans MD, Larkin JO, Beynon J, Winter DC (2013) Multivisceral resection in colorectal cancer: a systematic review. Ann Surg Oncol 20:2929–2936. doi:10.1245/s10434-013-2967-9
Hoffmann M, Phillips C, Oevermann E, Killaitis C, Roblick UJ, Hildebrand P, Buerk CG, Wolken H, Kujath P, Schloericke E, Bruch HP (2012) Multivisceral and standard resections in colorectal cancer. Langenbeck’s Arch Surg 397:75–84. doi:10.1007/s00423-011-0854-z
Bayar B, Yılmaz KB, Akıncı M, Şahin A, Kulaçoğlu H (2016) An evaluation of treatment results of emergency versus elective surgery in colorectal cancer patients. Ulus Cerrahi Derg 32:11–17. doi:10.5152/UCD.2015.2969
Huh JW, Kim HR (2012) The feasibility of laparoscopic resection compared to open surgery in clinically suspected T4 colorectal cancer. J Laparoendosc Adv Surg Tech A 22:463–467. doi:10.1089/lap.2011.0425
Acknowledgements
The authors acknowledge F.S. van Etten-Jamaludin for her assistance with the search strategy.
Author information
Authors and Affiliations
Contributions
Study conception and design: CELK, TMK, WAAB, WAB, and PJT. Acquisition of data: CELK, TMK, and WAAB. Analysis and interpretation of data: CELK, TMK, WAAB, WAB, and PJT. Writing manuscript: CELK, TMK, and PJT. Revising it critically for important intellectual content: WAB and PJT. All authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Disclosures
C.E.L. Klaver, T. M. Kappen, W.A.A. Borstlap, W.A. Bemelman, and P.J. Tanis have no conflicts of interest or financial ties to disclose.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Klaver, C.E.L., Kappen, T.M., Borstlap, W.A.A. et al. Laparoscopic surgery for T4 colon cancer: a systematic review and meta-analysis. Surg Endosc 31, 4902–4912 (2017). https://doi.org/10.1007/s00464-017-5544-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-017-5544-7