Abstract
Background
Robotic-assisted surgery is used with increasing frequency in general surgery for a variety of applications. In spite of this increase in usage, the learning curve is not yet defined. This study reviews the literature on the learning curve in robotic general surgery to inform adopters of the technology.
Methods
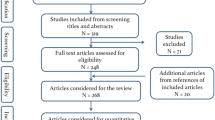
PubMed and EMBASE searches yielded 3690 abstracts published between July 1986 and March 2016. The abstracts were evaluated based on the following inclusion criteria: written in English, reporting original work, focus on general surgery operations, and with explicit statistical methods.
Results
Twenty-six full-length articles were included in final analysis. The articles described the learning curves in colorectal (9 articles, 35%), foregut/bariatric (8, 31%), biliary (5, 19%), and solid organ (4, 15%) surgery. Eighteen of 26 (69%) articles report single-surgeon experiences. Time was used as a measure of the learning curve in all studies (100%); outcomes were examined in 10 (38%). In 12 studies (46%), the authors identified three phases of the learning curve. Numbers of cases needed to achieve plateau performance were wide-ranging but overlapping for different kinds of operations: 19–128 cases for colorectal, 8–95 for foregut/bariatric, 20–48 for biliary, and 10–80 for solid organ surgery.
Conclusion
Although robotic surgery is increasingly utilized in general surgery, the literature provides few guidelines on the learning curve for adoption. In this heterogeneous sample of reviewed articles, the number of cases needed to achieve plateau performance varies by case type and the learning curve may have multiple phases as surgeons add more complex cases to their case mix with growing experience. Time is the most common determinant for the learning curve. The literature lacks a uniform assessment of outcomes and complications, which would arguably reflect expertise in a more meaningful way than time to perform the operation alone.


Similar content being viewed by others
References
Herron DM, Marohn M, SAGES-MIRA Robotic Surgery Consensus Group (2008) A consensus document on robotic surgery. Surg Endosc 22:313–325. doi:10.1007/s00464-007-9727-5
Melich G, Hong YK, Kim J, Hur H, Baik SH, Kim NK, Sender Liberman A, Min BS (2015) Simultaneous development of laparoscopy and robotics provides acceptable perioperative outcomes and shows robotics to have a faster learning curve and to be overall faster in rectal cancer surgery: analysis of novice MIS surgeon learning curves. Surg Endosc 29:558–568. doi:10.1007/s00464-014-3698-0
Anderson JE, Chang DC, Parsons JK, Talamini MA (2012) The first national examination of outcomes and trends in robotic surgery in the United States. J Am Coll Surg 215:107–114. doi:10.1016/j.jamcollsurg.2012.02.005
da Vinci Surgery. Minimally Invasive Robotic Surgery with the da Vinci Surgical System. http://www.davincisurgery.com/clinical-evidence.php. Accessed 13 Oct 2016
Hatlie MJ (1993) Climbing “the learning curve”. New technologies, emerging obligations. JAMA 270:1364–1365
Cagir B, Rangraj M, Maffuci L, Herz BL (1994) The learning curve for laparoscopic cholecystectomy. J Laparoendosc Surg 4:419–427
Bibi S, Rahnemai-Azar AA, Coralic J, Bayoumi M, Khorsand J, Farkas DT, Prasad LM (2015) Single-site robotic cholecystectomy: the timeline of progress. World J Surg 39:2386–2391. doi:10.1007/s00268-015-3135-0
Bokhari MB, Patel CB, Ramos-Valadez DI, Ragupathi M, Haas EM (2011) Learning curve for robotic-assisted laparoscopic colorectal surgery. Surg Endosc 25:855–860. doi:10.1007/s00464-010-1281-x
Boone BA, Zenati M, Hogg ME, Steve J, Moser AJ, Bartlett DL, Zeh HJ, Zureikat AH (2015) Assessment of quality outcomes for robotic pancreaticoduodenectomy: identification of the learning curve. JAMA Surg 150:416–422. doi:10.1001/jamasurg.2015.17
Hernandez JM, Dimou F, Weber J, Almhanna K, Hoffe S, Shridhar R, Karl R, Meredith K (2013) Defining the learning curve for robotic-assisted esophagogastrectomy. J Gastrointest Surg Off J Soc Surg Aliment Tract 17:1346–1351. doi:10.1007/s11605-013-2225-2
Kubat E, Hansen N, Nguyen H, Wren SM, Eisenberg D (2016) Urgent and elective robotic single-site cholecystectomy: analysis and learning curve of 150 consecutive cases. J Laparoendosc Adv Surg Tech A 26:185–191. doi:10.1089/lap.2015.0528
Nelson EC, Gottlieb AH, Müller H-G, Smith W, Ali MR, Vidovszky TJ (2014) Robotic cholecystectomy and resident education: the UC Davis experience. Int J Med Robot Comput Assist Surg MRCAS 10:218–222. doi:10.1002/rcs.1554
Shakir M, Boone BA, Polanco PM, Zenati MS, Hogg ME, Tsung A, Choudry HA, Moser AJ, Bartlett DL, Zeh HJ, Zureikat AH (2015) The learning curve for robotic distal pancreatectomy: an analysis of outcomes of the first 100 consecutive cases at a high-volume pancreatic centre. HPB 17:580–586. doi:10.1111/hpb.12412
Vidovszky TJ, Smith W, Ghosh J, Ali MR (2006) Robotic cholecystectomy: learning curve, advantages, and limitations. J Surg Res 136:172–178. doi:10.1016/j.jss.2006.03.021
Kim H-I, Park MS, Song KJ, Woo Y, Hyung WJ (2014) Rapid and safe learning of robotic gastrectomy for gastric cancer: multidimensional analysis in a comparison with laparoscopic gastrectomy. Eur J Surg Oncol J Eur Soc Surg Oncol Br Assoc Surg Oncol 40:1346–1354. doi:10.1016/j.ejso.2013.09.011
Kim HJ, Choi G-S, Park JS, Park SY (2014) Multidimensional analysis of the learning curve for robotic total mesorectal excision for rectal cancer: lessons from a single surgeon’s experience. Dis Colon Rectum 57:1066–1074. doi:10.1097/DCR.0000000000000174
Kim Y-W, Lee H-M, Kim N-K, Min B-S, Lee K-Y (2012) The learning curve for robot-assisted total mesorectal excision for rectal cancer. Surg Laparosc Endosc Percutan Tech 22:400–405. doi:10.1097/SLE.0b013e3182622c2d
Park EJ, Kim CW, Cho MS, Baik SH, Kim DW, Min BS, Lee KY, Kim NK (2014) Multidimensional analyses of the learning curve of robotic low anterior resection for rectal cancer: 3-phase learning process comparison. Surg Endosc 28:2821–2831. doi:10.1007/s00464-014-3569-8
Park S-S, Kim M-C, Park MS, Hyung WJ (2012) Rapid adaptation of robotic gastrectomy for gastric cancer by experienced laparoscopic surgeons. Surg Endosc 26:60–67. doi:10.1007/s00464-011-1828-5
Sng KK, Hara M, Shin J-W, Yoo B-E, Yang K-S, Kim S-H (2013) The multiphasic learning curve for robot-assisted rectal surgery. Surg Endosc 27:3297–3307. doi:10.1007/s00464-013-2909-4
Buchs NC, Pugin F, Bucher P, Hagen ME, Chassot G, Koutny-Fong P, Morel P (2012) Learning curve for robot-assisted Roux-en-Y gastric bypass. Surg Endosc 26:1116–1121. doi:10.1007/s00464-011-2008-3
Cundy TP, Rowland SP, Gattas NE, White AD, Najmaldin AS (2015) The learning curve of robot-assisted laparoscopic fundoplication in children: a prospective evaluation and CUSUM analysis. Int J Med Robot Comput Assist Surg MRCAS 11:141–149. doi:10.1002/rcs.1610
Giza D-E, Tudor S, Purnichescu-Purtan RR, Vasilescu C (2014) Robotic splenectomy: what is the real benefit? World J Surg 38:3067–3073. doi:10.1007/s00268-014-2697-6
Jiménez-Rodríguez RM, Díaz-Pavón JM, de Juan FDLP, Prendes-Sillero E, Dussort HC, Padillo J (2013) Learning curve for robotic-assisted laparoscopic rectal cancer surgery. Int J Colorectal Dis 28:815–821. doi:10.1007/s00384-012-1620-6
Napoli N, Kauffmann EF, Perrone VG, Miccoli M, Brozzetti S, Boggi U (2015) The learning curve in robotic distal pancreatectomy. Updates Surg 67:257–264. doi:10.1007/s13304-015-0299-y
Pietrabissa A, Sbrana F, Morelli L, Badessi F, Pugliese L, Vinci A, Klersy C, Spinoglio G (2012) Overcoming the challenges of single-incision cholecystectomy with robotic single-site technology. Arch Surg 147:709–714. doi:10.1001/archsurg.2012.508
Renaud M, Reibel N, Zarnegar R, Germain A, Quilliot D, Ayav A, Bresler L, Brunaud L (2013) Multifactorial analysis of the learning curve for totally robotic Roux-en-Y gastric bypass for morbid obesity. Obes Surg 23:1753–1760. doi:10.1007/s11695-013-1020-1
Vilallonga R, Fort JM, Gonzalez O, Caubet E, Boleko A, Neff KJ, Armengol M (2012) The initial learning curve for robot-assisted sleeve gastrectomy: a surgeon’s experience while introducing the robotic technology in a bariatric surgery department. Minim Invasive Surg 2012:347131. doi:10.1155/2012/347131
Foo CC, Law WL (2016) The learning curve of robotic-assisted low rectal resection of a novice rectal surgeon. World J Surg 40:456–462. doi:10.1007/s00268-015-3251-x
Kuo L-J, Lin Y-K, Chang C-C, Tai C-J, Chiou J-F, Chang Y-J (2014) Clinical outcomes of robot-assisted intersphincteric resection for low rectal cancer: comparison with conventional laparoscopy and multifactorial analysis of the learning curve for robotic surgery. Int J Colorectal Dis 29:555–562. doi:10.1007/s00384-014-1841-y
Yamaguchi T, Kinugasa Y, Shiomi A, Sato S, Yamakawa Y, Kagawa H, Tomioka H, Mori K (2015) Learning curve for robotic-assisted surgery for rectal cancer: use of the cumulative sum method. Surg Endosc 29:1679–1685. doi:10.1007/s00464-014-3855-5
Zhou J, Shi Y, Qian F, Tang B, Hao Y, Zhao Y, Yu P (2015) Cumulative summation analysis of learning curve for robot-assisted gastrectomy in gastric cancer. J Surg Oncol 111:760–767. doi:10.1002/jso.23876
Classics in the History of Psychology—Introduction to Ebbinghaus (1885/1913) by R. H. Wozniak. http://psychclassics.yorku.ca/Ebbinghaus/wozniak.htm. Accessed 13 Oct 2016
Classics in the History of Psychology—Ebbinghaus (1885/1913) Chapter 1. http://psychclassics.yorku.ca/Ebbinghaus/index.htm. Accessed 13 Oct 2016
Swift EJ (1903) Studies in the psychology and physiology of learning. Am J Psychol 14:201–251. doi:10.2307/1412713
Wohl H (1977) The cusum plot: its utility in the analysis of clinical data. N Engl J Med 296:1044–1045. doi:10.1056/NEJM197705052961806
Ramsay CR, Grant AM, Wallace SA, Garthwaite PH, Monk AF, Russell IT (2001) Statistical assessment of the learning curves of health technologies. Health Technol Assess Winch Engl 5:1–79
Barrie J, Jayne DG, Wright J, Murray CJC, Collinson FJ, Pavitt SH (2014) Attaining surgical competency and its implications in surgical clinical trial design: a systematic review of the learning curve in laparoscopic and robot-assisted laparoscopic colorectal cancer surgery. Ann Surg Oncol 21:829–840. doi:10.1245/s10434-013-3348-0
Darzi A, Smith S, Taffinder N (1999) Assessing operative skill. Needs to become more objective. BMJ 318:887–888
Bric J, Connolly M, Kastenmeier A, Goldblatt M, Gould JC (2014) Proficiency training on a virtual reality robotic surgical skills curriculum. Surg Endosc 28:3343–3348. doi:10.1007/s00464-014-3624-5
Gomez PP, Willis RE, Van Sickle KR (2015) Development of a virtual reality robotic surgical curriculum using the da Vinci Si surgical system. Surg Endosc 29:2171–2179. doi:10.1007/s00464-014-3914-y
Aghazadeh MA, Jayaratna IS, Hung AJ, Pan MM, Desai MM, Gill IS, Goh AC (2015) External validation of global evaluative assessment of robotic skills (GEARS). Surg Endosc 29:3261–3266. doi:10.1007/s00464-015-4070-8
Acknowledgements
Luise I. M. Pernar, MD was supported by the Foundation for Surgical Fellowships.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Dr. Tavakkoli receives consulting fees from Medtronic. Dr. Sheu received consulting fees from Kitotech and has received a grant from Mederi Therapeutics. Dr. Pernar, Dr. Brooks, Dr. Smink, and Ms. Robertson have no conflicts of interest or financial ties to disclose.
Rights and permissions
About this article
Cite this article
Pernar, L.I.M., Robertson, F.C., Tavakkoli, A. et al. An appraisal of the learning curve in robotic general surgery. Surg Endosc 31, 4583–4596 (2017). https://doi.org/10.1007/s00464-017-5520-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-017-5520-2