Abstract
Background
Laparoscopy offers some evidence of benefit compared to open rectal surgery. Robotic rectal surgery is evolving into an accepted approach. The objective was to analyze and compare laparoscopic and robotic rectal surgery learning curves with respect to operative times and perioperative outcomes for a novice minimally invasive colorectal surgeon.
Methods
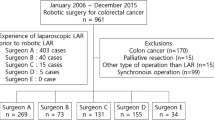
One hundred and six laparoscopic and 92 robotic LAR rectal surgery cases were analyzed. All surgeries were performed by a surgeon who was primarily trained in open rectal surgery. Patient characteristics and perioperative outcomes were analyzed. Operative time and CUSUM plots were used for evaluating the learning curve for laparoscopic versus robotic LAR.
Results
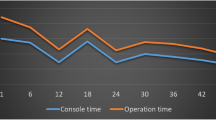
Laparoscopic versus robotic LAR outcomes feature initial group operative times of 308 (291–325) min versus 397 (373–420) min and last group times of 220 (212–229) min versus 204 (196-211) min—reversed in favor of robotics; major complications of 4.7 versus 6.5 % (NS), resection margin involvement of 2.8 versus 4.4 % (NS), conversion rate of 3.8 versus 1.1 (NS), lymph node harvest of 16.3 versus 17.2 (NS), and estimated blood loss of 231 versus 201 cc (NS). Due to faster learning curves for extracorporeal phase and total mesorectal excision phase, the robotic surgery was observed to be faster than laparoscopic surgery after the initial 41 cases. CUSUM plots demonstrate acceptable perioperative surgical outcomes from the beginning of the study.
Conclusions
Initial robotic operative times improved with practice rapidly and eventually became faster than those for laparoscopy. Developing both laparoscopic and robotic skills simultaneously can provide acceptable perioperative outcomes in rectal surgery. It might be suggested that in the current milieu of clashing interests between evolving technology and economic constrains, there might be advantages in embracing both approaches.










Similar content being viewed by others
References
Larach SW, Salomon MC, Williamson PR, Goldstein E (1993) Laparoscopic assisted abdominoperineal resection. Surg Laparosc Endosc 3(2):115–118
Chindasub S, Charntaracharmnong C, Nimitvanit C, Akkaranurukul P, Santitarmmanon B (1994) Laparoscopic abdominoperineal resection. J Laparoendosc Surg 4(1):17–21
Darzi A, Lewis C, Menzies Gow N, Guillou PJ, Monson JR (1995) Laparoscopic abdominoperineal excision of the rectum. Surg Endosc 9(4):414–417
Ramos JR, Petrosemolo RH, Valory EA, Polania FC, Pecanha R (1997) Abdominoperineal resection: laparoscopic versus conventional. Surg Laparosc Endosc 7(2):148–152
Iroatulam AJ, Agachan F, Alabaz O, Weiss EG, Nogueras JJ, Wexner SD (1998) Laparoscopic abdominoperineal resection for anorectal cancer. Am Surg 64(1):12–18
Fleshman JW, Wexner SD, Anvari M, La Tulippe JF, Birnbaum EH, Kodner IJ et al (1999) Laparoscopic versus open abdominoperineal resection for cancer. Dis Colon Rectum 42(7):930–939
Laurent C, Leblanc F, Wütrich P, Scheffler M, Rullier E (2009) Laparoscopic versus open surgery for rectal cancer: long-term oncologic results. Ann Surg 250(1):54–61
Jayne DG, Thorpe HC, Copeland J, Quirke P, Brown JM, Guillou PJ (2010) Five-year follow-up of the Medical Research Council CLASICC trial of laparoscopically assisted versus open surgery for colorectal cancer. Br J Surg 97(11):1638–1645
Trastulli S, Cirocchi R, Listorti C, Cavaliere D, Avenia N, Gullà N, Giustozzi G, Sciannameo F, Noya G, Boselli C (2012) Laparoscopic versus open resection for rectal cancer: a meta-analysis of randomized clinical trials. Colorectal Dis 14(6):277–296
Baik SH, Kwon HY, Kim JS et al (2009) Robotic versus laparoscopic low anterior resection of rectal cancer: short-term outcome of a prospective comparative study. Ann Surg Oncol 16(6):1480–1487
Mirnezami AH, Mirnezami R, Venkatasubramaniam AK et al (2010) Robotic colorectal surgery: hype or new hope? A systematic review of robotics in colorectal surgery. Colorectal Dis 12(11):1084–1093
Patriti A, Ceccarelli G, Bartoli A, Spaziani A, Biancafarina A, Casciola L (2009) Short- and medium-term outcome of robot-assisted and traditional laparoscopic rectal resection. JSLS 13(2):176–183
Bianchi PP, Ceriani C, Locatelli A, Spinoglio G, Zampino MG, Sonzogni A, Crosta C, Andreoni B (2010) Robotic versus laparoscopic total mesorectal excision for rectal cancer: a comparative analysis of oncological safety and short-term outcomes. Surg Endosc 24(11):2888–2894
Park JS, Choi GS, Lim KH, Jang YS, Jun SH (2010) Robotic-assisted versus laparoscopic surgery for low rectal cancer: case-matched analysis of short-term outcomes. Ann Surg Oncol 17(12):3195–3202
Baek JH, McKenzie S, Garcia-Aguilar J, Pigazzi A (2010) Oncologic outcomes of robotic-assisted total mesorectal excision for the treatment of rectal cancer. Ann Surg 251(5):882–886
Kim JY, Kim NK, Lee KY, Huh H, Min BS, Kim JW (2012) A comparative study of voiding and sexual function after Total Mesenteric excision with autonomic nerve preservation for rectal cancer: laparoscopic versus robotic surgery. Ann Surg Oncol 19(8):2485–2493
Baek JH, Pastor C, Pigazzi A (2011) Robotic and laparoscopic total mesorectal excision for rectal cancer: a case-matched study. Surg Endosc 25:521–525
Kim NK, Kang J (2010) Optimal total mesorectal excision for ectal cancer: the role of robotic surgery from an expert’s view. J Korean Soc Coloproctology 26:377–387
Delaney CP, Lynch AC, Senagore AJ, Fazio VW (2003) Comparison of robotically performed and traditional laparoscopic colorectal surgery. Dis Colon Rectum 46:1633–1639
Rawlings AL, Woodland JH, Vegunta RK, Crawford DL (2007) Robotic versus laparoscopic colectomy. Surg Endosc 21:1701–1708
Hommel G, Röhrig B, Blettner M (2009) Confidence Interval or P-Value? Dtsch Arztebl Int 106(19):335–339
Lim TO, Soraya A, Ding LM, Morad Z (2002) Assessing doctors’ competence: application of CUSUM technique in monitoring doctor’s performance. Int J Qual Health Care 14(3):251–258
Colquhoun PHD (2008) CUSUM analysis of J-pouch surgery reflects no learning curve after board certification. Can J Surg 51(4):296–299
Bokhari MB, Patel CB, Ramos-Valadez DI, Ragupathi M, Haas EM (2011) Learning curve for robotic-assisted laparoscopic colorectal surgery. Surg Endosc 25(3):855–860
Taflampas P, Christodoulakis M, Tsiftis DD (2009) Anastomotic Leakage after low anterior resection for rectal cancer: facts, obscurity, and fiction. Surg Today 39:183–188
Aziz O, Constantinides V, Tekkis PP, Athanasiou T, Purkayastha S, Paraskeva P, Darzi AW, Heriot AG (2006) Laparoscopic versus open surgery for rectal cancer: a meta-analysis. Ann Surg Oncol 13(3):413–424
Nagtegaal ID, Quirke P (2008) What is the role for the circumferential margin in the modern treatment of rectal cancer? J Clin Oncol 26(2):303–312
Spinoglio G, Summa M, Priora F, Quarati R, Testa S (2008) Robotic colorectal surgery: first 50 cases experience. Dis Colon Rectum 51(11):1627–1632
Hellan CM, Anderson C, Ellenhorn JDI, Paz B, Pigazzi A (2007) Short-term outcomes after robotic-assisted total mesorectal excision for rectal cancer. Ann Surg Oncol 14(11):3168–3173
Akmal Y, Baek JH, McKenzie S, Garcia-Aguilar J, Pigazzi A. Robot-assisted total mesorectal excision: is there a learning curve? Surg Endosc 2012; Surg Endosc. 2012 Mar 22 [Epub ahead of print],PMID: 22437950
Kayano H, Okuda J, Tanaka K, Kondo K, Tanigawa N (2011) Evaluation of the learning curve in laparoscopic low anterior resection for rectal cancer. Surg Endosc 25:2972–2979
Stefanidis D, Wang F, Korndorffer JR, Dunne JB, Scott DJ (2010) Robotic assistance improves intracorporeal suturing performance and safety in the operating room while decreasing operator workload. Surg Endosc 24(2):377–382
Acknowledgement
We would like to express our gratitude to Mr. Martin Morris, Librarian, Medical Library, Royal Victoria Hospital, McGill University, Montreal, Canada for assistance with literature search and Mrs. Myo Jeong Kim, MS with Dr. Dong Wook Kim, PhD from the Biostatistics Collaboration Unit, Yonsei University College of Medicine, Seoul, South Korea for their help with statistical analysis. We also acknowledge and appreciate editing services of Mr. Shaun Fawcett of Final Draft Consulting, Montreal.
Disclosure
Drs. George Melich, Young Ki Hong, Jieun, Kim, and Sender Liberman have no conflicts of interest or financial ties to disclose. Drs. Hyuk Hur MD, Seung Hyuk Baik, Nam Kyu Kim, and Byung Soh Min have received in the past travel and speaking honoraria from Intuitive Surgical.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Melich, G., Hong, Y.K., Kim, J. et al. Simultaneous development of laparoscopy and robotics provides acceptable perioperative outcomes and shows robotics to have a faster learning curve and to be overall faster in rectal cancer surgery: analysis of novice MIS surgeon learning curves. Surg Endosc 29, 558–568 (2015). https://doi.org/10.1007/s00464-014-3698-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-014-3698-0