Abstract
Background
Accurate measurement of esophageal hiatus size is clinically important, especially when antireflux surgery is planned. We present a novel method for in vivo measurement of esophageal hiatal surface area using MDCT multiplanar reconstruction. We aimed to determine whether large hiatal area is associated with hiatal hernia and gastroesophageal reflux disease.
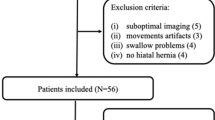
Methods
We retrospectively analyzed subjects prospectively enrolled in the COPDGene® project. We created two test groups, one with hiatal hernia on chest CT and one with GERD on medical treatment identified by history without hernia. Matched control groups were formed. We performed CT postprocessing to define the double-oblique plane of the esophageal hiatus, on which the hiatal surface area is manually traced.
Results
Subjects with hernia (n = 48) had larger mean hiatus areas than matched controls (6.9 vs. 2.5 cm2, p < 0.0001), and were more likely to have GERD (42 vs. 10 %, p < 0.0005). Subjects with mixed (type III) hernias had larger hiatuses compared to subjects with sliding (type I) hernias, who, in turn, had larger hiatuses than subjects without hernia (p < 0.0001). Hernia-negative subjects with GERD (n = 55) did not have significantly larger mean hiatal areas compared to matched controls (3.0 vs. 2.5 cm2, p = 0.12). Twenty measurements obtained by two radiologists showed correlation of 0.93, with mean difference of 0.5 cm2 (p = 0.20).
Conclusions
We devised a method to measure in vivo esophageal hiatal surface area using MDCT reconstruction and established the normal size range for the first time. This methodology has the potential to guide decision-making in antireflux surgery technique preoperatively, and assess surgical result postoperatively. The presence of hernia correlated with large hiatuses and GERD. However, hiatal area failed to identify those with GERD in the absence of hiatal hernia.








Similar content being viewed by others
References
Collis J, Kelly T, Wiley A (1954) Anatomy of the crura of the diaphragm and the surgery of hiatus hernia. Thorax 9:175–189
Barbosa Costa M, Ary Pires-Neto M (2004) Anatomical investigation of the esophageal and aortic hiatuses: physiologic, clinical and surgical considerations. Anat Sci Int 79:21–31
Loukas M, Wartmann ChT, Tubbs RS, Apaydin N, Louis RG Jr, Gupta AA, Jordan R (2008) Morphologic variation of the diaphragmatic crura: a correlation with pathologic processes of the esophageal hiatus? Folia Morphol (Warsz) 67:273–279
Mittal RK, Rochester DF, McCallum RW (1989) Sphincteric action of the diaphragm during a relaxed lower esophageal sphincter in humans. Am J Physiol 256:G139–G144
Gordon C, Kang J, Neild P, Maxwell J (2004) The role of the hiatus hernia in gastro-oesophageal reflux disease. Aliment Pharmacol Ther 20:719–732
Gryglewski A, Pena I, Tomaszewski K, Walocha J (2014) Unsolved questions regarding the role of esophageal hiatus anatomy in the development of esophageal hiatal hernias. Adv Clin Exp Med 23:639–644
Batirel H, Uygur-Bayramicli O, Giral A, Ekici B, Bekiroglu N, Yildizeli B, Yüksel M (2009) The size of the esophageal hiatus in gastroesophageal reflux pathophysiology: outcome of intraoperative measurements. J Gastrointest Surg 14:38–44
Koch O, Kaindlstorfer A, Antoniou S, Asche K, Granderath F, Pointner R (2012) Influence of the esophageal hiatus size on the lower esophageal sphincter, on reflux activity and on symptomatology. Dis Esophagus 25:201–208
Koch O, Asche K, Berger J, Weber E, Granderath F, Pointner R (2011) Influence of the size of the hiatus on the rate of reherniation after laparoscopic fundoplication and refundopilication with mesh hiatoplasty. Surg Endosc 25:1024–1030
Grubnik V, Malynovskyy A (2013) Laparoscopic repair of hiatal hernias: new classification supported by long-term results. Surg Endosc 27:4337–4346
Granderath F (2007) Measurement of the esophageal hiatus by calculation of the hiatal surface area (HSA). Why, when and how? Surg Endosc 21:2224–2225
Antoniou S, Pointner R, Granderath F (2014) Hiatal surface area as a basis for a new classification of hiatal hernia. Surg Endosc 28:1384–1385
Koch O, Schurich M, Antoniou S, Spaun G, Kaindlstorfer A, Pointner R, Swanstrom L (2013) Predictability of hiatal hernia/defect size: is there a correlation between pre- and intraoperative findings? Hernia 18:883–888
Granderath F, Schweiger U, Pointner R (2007) Laparoscopic antireflux surgery: tailoring the hiatal closure to the size of hiatal surface area. Surg Endosc 21:542–548
Shamiyeh A, Szabo K, Granderath F, Syré G, Wayand W, Zehetner J (2010) The esophageal hiatus: what is the normal size? Surg Endosc 24:988–991
Regan E, Hokanson J, Murphy J, Make B, Lynch D, Beaty T, Curran-Everett D, Silverman E, Crapo J (2010) Genetic epidemiology of COPD (COPDGene) study design. COPD 7:32–43
Abbara S, Kalan M, Lewicki A (2003) Intrathoracic stomach revisited. Am J Roentgenol 181:403–414
Cerillo A, Mariani M, Berti S, Glauber M (2012) Sizing the aortic annulus. Ann Cardiothorac Surg 1:245–256
Sloan S, Rademaker A, Kahrilas P (1992) Determinants of gastroesophageal junction incompetence: hiatal hernia, lower esophageal sphincter, or both? Ann Intern Med 117:977
Kahrilas P (2003) GERD pathogenesis, pathophysiology, and clinical manifestations. Cleve Clin J Med 70:S4–S19
Jones M, Sloan S, Rabine J, Ebert C, Huang C, Kahrilas P (2001) Hiatal hernia size is the dominant determinant of esophagitis presence and severity in gastroesophageal reflux disease. Am J Gastroenterol 96:1711–1717
Franzén T (2014) Is the severity of gastroesophageal reflux dependent on hiatus hernia size? WJG 20:1582
Chen M, Ott D, Sinclair J, Wu W, Gelfand D (1992) Gastroesophageal reflux disease: correlation of esophageal pH testing and radiographic findings. Radiology 185:483–486
Saleh C, Smout A, Bredenoord A (2014) The diagnosis of gastro-esophageal reflux disease cannot be made with barium esophagograms. Neurogastroenterol Motil 27:195–200
Acknowledgments
The authors wish to thank the COPDGene® investigators for access to their considerable body of data and continued support of this research.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Rights and permissions
About this article
Cite this article
Ouyang, W., Dass, C., Zhao, H. et al. Multiplanar MDCT measurement of esophageal hiatus surface area: association with hiatal hernia and GERD. Surg Endosc 30, 2465–2472 (2016). https://doi.org/10.1007/s00464-015-4499-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-015-4499-9