Abstract
Introduction
There is an increasing emphasis on optimizing and measuring surgical quality. The safety and efficacy of minimally invasive techniques have been proven; however, direct comparison of outcomes across platforms has not been performed. Our goal was to compare operative times and quality across three minimally invasive platforms in colorectal surgery.
Methods
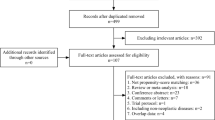
A prospective database was reviewed for elective minimally invasive surgery (MIS) cases from 2008 to 2014. Patients were stratified into multiport laparoscopic, single-incision laparoscopic (SILS) or robotic-assisted laparoscopic approaches (RALS). Demographics, perioperative, and postoperative outcomes were analyzed. Multivariate regression analysis was used to predict the demographic and procedural factors and outcomes associated with each platform. The main outcome measures were operative time and surgical quality by approach.
Results
A total of 1055 cases were evaluated—28.4 % LAP, 18.5 % RALS, and 53.1 % SILS. RALS had the most complex patients, pathology, and procedures. The main diagnosis for RALS was rectal cancer (49.5 %), patients predominantly underwent pelvic surgery (72.8 %), had higher rates of neoadjuvant chemoradiation (p < 0.001) and stoma creation (p < 0.001). RALS had the longest operative time and highest complication and readmissions rates (all p < 0.001). Multiport patients were older than SILS and RALS (p = 0.021), had the most intraoperative complications (p < 0.001), conversions (p < 0.001), and had the longest length of stay (p = 0.001). SILS had the shortest operative times (p < 0.001), length of stay (p = 0.001), and lowest rates of complications (p < 0.001), readmissions (p < 0.001), and unplanned reoperation (p = 0.014). All platforms offered high quality (HARM score 0) from overall short LOS, low readmission, and mortality rates.
Conclusions
Multiport, RALS, and SILS each serve a distinct demographic and disease profile and have predictable outcomes. All have risks and benefits, but offer overall high-quality care with a composite of LOS, readmission, and mortality rates. Operative times were directly associated with readmission rates. As all three platforms offer good quality, the choice of which MIS approach to use should be guided by demographics and disease process.


Similar content being viewed by others
References
Birkmeyer JD, Dimick JB, Birkmeyer NJ (2004) Measuring the quality of surgical care: structure, process, or outcomes? J Am Coll Surg 198:626–632
Almoudaris AM, Clark S, Vincent C, Faiz O (2011) Establishing quality in colorectal surgery. Colorectal Dis 13:961–973
Bilimoria KY, Cohen ME, Merkow RP et al (2010) Comparison of outlier identification methods in hospital surgical quality improvement programs. J Gastrointest Surg 14:1600–1607
Flum DR, Pellegrini CA (2012) The business of quality in surgery. Ann Surg 255:6–7
Keller DS, Chien HL, Hashemi L, Senagore AJ, Delaney CP (2014) The HARM score: a novel, easy measure to evaluate quality and outcomes in colorectal surgery. Ann Surg 259:1119–1125
Centers for Medicare and Medicaid Readmissions Reduction Program (2012). http://cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/Readmissions-Reduction-Program.html. Accessed Mar 2015
Medicare.gov Hospital Compare. http://www.medicare.gov/hospitalcompare/search.html. Accessed Dec 2014
CMS.gov Physician Quality Reporting System. http://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/PQRS/index.html?redirect=/PQRS/. Accessed Dec 2014
Kelly KN, Iannuzzi JC, Rickles AS, Monson JR, Fleming FJ (2014) Risk factors associated with 30-day postoperative readmissions in major gastrointestinal resections. J Gastrointest Surg 18(1):35–43; discussion 43–44
Bailey MB, Davenport DL, Vargas HD, Evers BM, McKenzie SP (2014) Longer operative time: deterioration of clinical outcomes of laparoscopic colectomy versus open colectomy. Dis Colon Rectum 57:616–622
Collins TC, Daley J, Henderson WH, Khuri SF (1999) Risk factors for prolonged length of stay after major elective surgery. Ann Surg 230:251–259
Kurmann A, Vorburger SA, Candinas D, Beldi G (2011) Operation time and body mass index are significant risk factors for surgical site infection in laparoscopic sigmoid resection: a multicenter study. Surg Endosc 25:3531–3534
Procter LD, Davenport DL, Bernard AC, Zwischenberger JB (2010) General surgical operative duration is associated with increased risk-adjusted infectious complication rates and length of hospital stay. J Am Coll Surg 210:60-5.e1–60-5.e2
Keller DS, Bankwitz B, Woconish D et al (2014) Predicting who will fail early discharge after laparoscopic colorectal surgery with an established enhanced recovery pathway. Surg Endosc 28:74–79
Evans C, Lim J, Gatzen C, Huang A (2012) Factors influencing laparoscopic colorectal operative duration and its effect on clinical outcome. Surg Laparosc Endosc Percutan Tech 22:437–442
Nelson H, Sargent DJ, COST Study Group (2004) A comparison of laparoscopically assisted and open colectomy for colon cancer. N Engl J Med 350:2050–2059
Bonjer HJ, Hop WC, Nelson H et al (2007) Laparoscopically assisted vs open colectomy for colon cancer: a meta-analysis. Arch Surg 142:298–303
Delaney CP, Chang E, Senagore AJ, Broder M (2008) Clinical outcomes and resource utilization associated with laparoscopic and open colectomy using a large national database. Ann Surg 247:819–824
Kennedy GD, Heise C, Rajamanickam V, Harms B, Foley EF (2009) Laparoscopy decreases postoperative complication rates after abdominal colectomy: results from the national surgical quality improvement program. Ann Surg 249:596–601
Lacy AM, Delgado S, Castells A et al (2008) The long-term results of a randomized clinical trial of laparoscopy-assisted versus open surgery for colon cancer. Ann Surg 248:1–7
Schwenk W, Haase O, Neudecker J, Muller JM (2005) Short term benefits for laparoscopic colorectal resection. Cochrane Database Syst Rev. doi:10.1002/14651858.CD003145.pub2
Veldkamp R, Kuhry E, Hop WC et al (2005) Laparoscopic surgery versus open surgery for colon cancer: short-term outcomes of a randomised trial. Lancet Oncol 6:477–484
Boutros M, Hippalgaonkar N, Silva E, Allende D, Wexner SD, Berho M (2013) Laparoscopic resection of rectal cancer results in higher lymph node yield and better short-term outcomes than open surgery: a large single-center comparative study. Dis Colon Rectum 56:679–688
Braga M, Frasson M, Vignali A, Zuliani W, Capretti G, Di Carlo V (2007) Laparoscopic resection in rectal cancer patients: outcome and cost-benefit analysis. Dis Colon Rectum 50:464–471
Chen HH, Wexner SD, Weiss EG et al (1998) Laparoscopic colectomy for benign colorectal disease is associated with a significant reduction in disability as compared with laparotomy. Surg Endosc 12:1397–1400
Shapiro SB, Lambert PJ, Mathiason MA (2008) A comparison of open and laparoscopic techniques in elective resection for diverticular disease. Wis Med J 107:287–291
Sklow B, Read T, Birnbaum E, Fry R, Fleshman J (2003) Age and type of procedure influence the choice of patients for laparoscopic colectomy. Surg Endosc 17:923–929
Salloum RM, Bulter DC, Schwartz SI (2006) Economic evaluation of minimally invasive colectomy. J Am Coll Surg 202:269–274
Biondi A, Grosso G, Mistretta A et al (2013) Laparoscopic vs. open approach for colorectal cancer: evolution over time of minimal invasive surgery. BMC Surg 13(Suppl 2):S12
D’Annibale A, Morpurgo E, Fiscon V et al (2004) Robotic and laparoscopic surgery for treatment of colorectal diseases. Dis Colon Rectum 47:2162–2168
Keller DS, Senagore AJ, Lawrence JK, Champagne BJ, Delaney CP (2014) Comparative effectiveness of laparoscopic versus robot-assisted colorectal resection. Surg Endosc 28(1):212–221
Kim CW, Kim CH, Baik SH (2014) Outcomes of robotic-assisted colorectal surgery compared with laparoscopic and open surgery: a systematic review. J Gastrointest Surg 18:816–830
Champagne BJ, Papaconstantinou HT, Parmar SS et al (2012) Single-incision versus standard multiport laparoscopic colectomy: a multicenter, case-controlled comparison. Ann Surg 255:66–69
Fung AK, Aly EH (2012) Systematic review of single-incision laparoscopic colonic surgery. Br J Surg 99:1353–1364
Huscher CG, Mingoli A, Sgarzini G et al (2012) Standard laparoscopic versus single-incision laparoscopic colectomy for cancer: early results of a randomized prospective study. Am J Surg 204:115–120
Makino T, Milsom JW, Lee SW (2012) Feasibility and safety of single-incision laparoscopic colectomy: a systematic review. Ann Surg 255:667–676
Trastulli S, Farinella E, Cirocchi R et al (2012) Robotic resection compared with laparoscopic rectal resection for cancer: systematic review and meta-analysis of short-term outcome. Colorectal Dis 14:e134–e156
Cevasco M, Ashley SW (2011) Quality measurement and improvement in general surgery. Perm J 15:48–53
Kassin MT, Owen RM, Perez SD et al (2012) Risk factors for 30-day hospital readmission among general surgery patients. J Am Coll Surg 215:322–330
Morris AM, Baldwin LM, Matthews B et al (2007) Reoperation as a quality indicator in colorectal surgery: a population-based analysis. Ann Surg 245:73–79
Delaney CP (2008) Outcome of discharge within 24–72 hours after laparoscopic colorectal surgery. Dis Colon Rectum 51:181–185
Delaney CP, Brady K, Woconish D, Parmar SP, Champagne BJ (2012) Towards optimizing perioperative colorectal care: outcomes for 1,000 consecutive laparoscopic colon procedures using enhanced recovery pathways. Am J Surg. 203:353–355; discussion 355–356
Kariv Y, Wang W, Senagore AJ, Hammel JP, Fazio VW, Delaney CP (2006) Multivariable analysis of factors associated with hospital readmission after intestinal surgery. Am J Surg 191:364–371
Kalish RL, Daley J, Duncan CC, Davis RB, Coffman GA, Iezzoni LI (1995) Costs of potential complications of care for major surgery patients. Am J Med Qual 10:48–54
Wick EC, Shore AD, Hirose K et al (2011) Readmission rates and cost following colorectal surgery. Dis Colon Rectum 54:1475–1479
Keller DS, Park KJ, Augestad KM, Delaney CP (2014) Integration of open and laparoscopic approaches for rectal cancer resection: oncologic and short-term outcomes. Surg Endosc 28:2129–2136
Baek SJ, Kim CH, Cho MS et al (2015) Robotic surgery for rectal cancer can overcome difficulties associated with pelvic anatomy. Surg Endosc 29(6):1419–1424
Memon S, Heriot AG, Murphy DG, Bressel M, Lynch AC (2012) Robotic versus laparoscopic proctectomy for rectal cancer: a meta-analysis. Ann Surg Oncol 19:2095–2101
Yang Y, Wang F, Zhang P et al (2012) Robot-assisted versus conventional laparoscopic surgery for colorectal disease, focusing on rectal cancer: a meta-analysis. Ann Surg Oncol 19(12):3727–3736
Keller DS, Bankwitz B, Nobel T, Delaney CP (2014) Using frailty to predict who will fail early discharge after laparoscopic colorectal surgery with an established recovery pathway. Dis Colon Rectum 57:337–342
Manilich E, Vogel JD, Kiran RP, Church JM, Seyidova-Khoshknabi D, Remzi FH (2013) Key factors associated with postoperative complications in patients undergoing colorectal surgery. Dis Colon Rectum 56:64–71
Azimuddin K, Rosen L, Reed JF III, Stasik JJ, Riether RD, Khubchandani IT (2001) Readmissions after colorectal surgery cannot be predicted. Dis Colon Rectum 44:942–946
Lee SW, Milsom JW, Nash GM (2011) Single-incision versus multiport laparoscopic right and hand-assisted left colectomy: a case-matched comparison. Dis Colon Rectum 54:1355–1361
Khayat A, Maggiori L, Vicaut E, Ferron M, Panis Y (2015) Does single port improve results of laparoscopic colorectal surgery? A propensity score adjustment analysis. Surg Endosc. doi:10.1007/s00464-015-4063-7
Patel CB, Ragupathi M, Ramos-Valadez DI, Haas EM (2011) A three-arm (laparoscopic, hand-assisted, and robotic) matched-case analysis of intraoperative and postoperative outcomes in minimally invasive colorectal surgery. Dis Colon Rectum 54:144–150
Dimick JB, Staiger DO, Hall BL, Ko CY, Birkmeyer JD (2013) Composite measures for profiling hospitals on surgical morbidity. Ann Surg 257:67–72
Acknowledgments
The authors acknowledge Jiandi Mo, MS for assistance with statistical analysis.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Deborah S. Keller, Juan R. Flores-Gonzalez, Sergio Ibarra, Nisreen Madhoun, Reena Tahilramani, Ali Mahmood, and Eric M. Haas have no conflicts of interest or financial ties to disclose.
Rights and permissions
About this article
Cite this article
Keller, D.S., Flores-Gonzalez, J.R., Ibarra, S. et al. Evaluating quality across minimally invasive platforms in colorectal surgery. Surg Endosc 30, 2207–2216 (2016). https://doi.org/10.1007/s00464-015-4479-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-015-4479-0