Abstract
Background
Our objective was to evaluate the impact of a novel multimodal pain management strategy on intraoperative opioid requirements, postoperative pain, narcotic use, and length of stay.
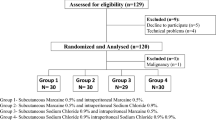
Methods
Consecutive patients undergoing elective laparoscopic colorectal resection were managed with an experimental protocol. The protocol uses a post-induction, pre-incision bilateral TAP block and local peritoneal infiltration at port sites with long-acting liposomal bupivacaine (20 mL long-acting liposomal bupivacaine, 30 mL 0.25 % bupivacaine, 30 mL saline). Experimental patients were matched on age, body mass index, gender, comorbidity, diagnosis, and procedure to a control group that received no block or local wound infiltration. Both groups followed a standardized enhanced recovery pathway. Demographics, perioperative, and postoperative outcomes were evaluated. The main outcome measures were intraoperative opioids, postoperative pain, opioid use, and length of stay.
Results
Fifty patients were analyzed—25 experimental and 25 controls. Patients were well matched on all demographics. In both cohorts, the main diagnosis was colorectal cancer and primary procedure performed a segmental resection. Operative times were similar (p = 0.41). Experimental patients received significantly less intraoperative fentanyl (mean 158 mcg experimental vs. 299 mcg control; p < 0.01). The experimental group had significantly lower initial (p < 0.01) and final PACU pain scores (p = 0.04) and shorter LOS (3.0 vs. 4.1 days, p = 0.04) compared to controls. Experimental patients trended toward shorter PACU times and lower opioid use and daily pain scores throughout the hospital stay. Postoperative complication and readmission rates were similar across groups. There were no reoperations or mortality.
Conclusions
Our multimodal pain management strategy reduced intraoperative opioid administration. Postoperatively, improvements in PACU time, postoperative pain and narcotic use, and lengths of stay were seen in the experimental cohort. With the favorable finding from the pilot study, further investigation is warranted to fully evaluate the impact of this pain management protocol on patient satisfaction, clinical and financial outcomes.
Similar content being viewed by others
References
Delaney CP, Zutshi M, Senagore AJ, Remzi FH, Hammel J, Fazio VW (2003) Prospective, randomized, controlled trial between a pathway of controlled rehabilitation with early ambulation and diet and traditional postoperative care after laparotomy and intestinal resection. Dis Colon Rectum 46:851–859
Vlug MS, Wind J, Hollmann MW et al (2011) Laparoscopy in combination with fast track multimodal management is the best perioperative strategy in patients undergoing colonic surgery: a randomized clinical trial (LAFA-study). Ann Surg 254:868–875
Adamina M, Kehlet H, Tomlinson GA, Senagore AJ, Delaney CP (2011) Enhanced recovery pathways optimize health outcomes and resource utilization: a meta-analysis of randomized controlled trials in colorectal surgery. Surgery 149:830–840
Adamina M, Senagore AJ, Delaney CP, Kehlet H (2015) A systematic review of economic evaluations of enhanced recovery pathways for colorectal surgery. Ann Surg 261(5):e138
Kehlet H, Wilmore DW (2008) Evidence-based surgical care and the evolution of fast-track surgery. Ann Surg 248:189–198
Joshi GP, Beck DE, Emerson RH et al (2014) Defining new directions for more effective management of surgical pain in the United States: highlights of the inaugural Surgical Pain Congress. Am Surg 80:219–228
Gosh S (1994) Patient satisfaction and postoperative demands on hospital and community services after day surgery. Br J Surg 81:1635–1638
Joshi GP (1994) Postoperative pain management. Int Anesthesiol Clin 32:113–126
Medicare. gov Hospital Compare. http://www.medicare.gov/hospitalcompare/search.html. Last Accessed Dec 2014
Centers for Medicare and Medicaid Services. Physician Quality Reporting System. http://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/PQRS/index.html?redirect=/PQRS/. Last Accessed Dec 2014
Centers for Medicare and Medicaid Readmissions Reduction Program. http://cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/Readmissions-Reduction-Program.html/. Last Accessed Mar 2015
Kehlet H, Wilkinson RC, Fischer HB, Camu F (2007) PROSPECT: evidence-based, procedure-specific postoperative pain management. Best Pract Res Clin Anaesthesiol 21:149–159
Barrington JW, Dalury DF, Emerson RHJ, Hawkins RJ, Joshi GP, Stulberg BN (2013) Improving patient outcomes through advanced pain management techniques in total hip and knee arthroplasty. Am J Orthop (Belle Mead NJ) 42:S1–S20
Carroll J, Alavi K (2009) Pathogenesis and management of postoperative ileus. Clin Colon Rectal Surg 22:47–50
Senagore AJ (2007) Pathogenesis and clinical and economic consequences of postoperative ileus. Am J Health Syst Pharm 64:S3–S7
Senagore AJ (2010) Pathogenesis and clinical and economic consequences of postoperative ileus. Clin Exp Gastroenterol 3:87–89
Delaney CP, Senagore AJ, Gerkin TM et al (2010) Association of surgical care practices with length of stay and use of clinical protocols after elective bowel resection: results of a national survey. Am J Surg 199:299–304
Kehlet H, Wilmore DW (2002) Multimodal strategies to improve surgical outcome. Am J Surg 183:630–641
Kehlet H (2008) Fast-track colorectal surgery. Lancet 371:791–793
Keller DS, Ermlich BO, Schiltz N et al (2014) The effect of transversus abdominis plane blocks on postoperative pain in laparoscopic colorectal surgery: a prospective, randomized, double-blind trial. Dis Colon Rectum 57:1290–1297
Hu D, Onel E, Singla N, Kramer WG, Hadzic A (2013) Pharmacokinetic profile of liposome bupivacaine injection following a single administration at the surgical site. Clin Drug Investig 33:109–115
Viscusi G, Sinatra R (2011) The safety of exparel, a multi-vesicular liposomal extended-release bupivacaine. International Anesthesia Research Society Annual Meeting, Vancouver
Alexander DJ, Ngoi SS, Lee L et al (1996) Randomized trial of periportal peritoneal bupivacaine for pain relief after laparoscopic cholecystectomy. Br J Surg 83:1223–1225
Colbert S, O’Hanlon DM, Courtney DF, Quill DS, Flynn N (1998) Analgesia following appendicectomy—the value of peritoneal bupivacaine. Can J Anaesth 45:729–734
Stuhldreher JM, Adamina M, Konopacka A, Brady K, Delaney CP (2012) Effect of local anesthetics on postoperative pain and opioid consumption in laparoscopic colorectal surgery. Surg Endosc 26:1617–1623
Haas E, Onel E, Miller H, Ragupathi M, White PF (2012) A double-blind, randomized, active-controlled study for post-hemorrhoidectomy pain management with liposome bupivacaine, a novel local analgesic formulation. Am Surg 78:574–581
Marcet JE, Nfonsam VN, Larach S (2013) An extended paIn relief trial utilizing the infiltration of a long-acting multivesicular liPosome foRmulation of bupiVacaine, EXPAREL (IMPROVE): a Phase IV health economic trial in adult patients undergoing ileostomy reversal. J Pain Res 6:549–555
Cohen SM (2012) Extended pain relief trial utilizing infiltration of Exparel((R)), a long-acting multivesicular liposome formulation of bupivacaine: a Phase IV health economic trial in adult patients undergoing open colectomy. J Pain Res. 5:567–572
Fayezizadeh M, Petro CC, Rosen MJ, Novitsky YW (2014) Enhanced recovery after surgery pathway for abdominal wall reconstruction: pilot study and preliminary outcomes. Plast Reconstr Surg 134:151S–159S
Gorfine SR, Onel E, Patou G, Krivokapic ZV (2011) Bupivacaine extended-release liposome injection for prolonged postsurgical analgesia in patients undergoing hemorrhoidectomy: a multicenter, randomized, double-blind, placebo-controlled trial. Dis Colon Rectum 54:1552–1559
Vogel JD (2013) Liposome bupivacaine (EXPAREL(R)) for extended pain relief in patients undergoing ileostomy reversal at a single institution with a fast-track discharge protocol: an IMPROVE Phase IV health economics trial. J Pain Res 6:605–610
Hawker GA, Mian S, Kendzerska T, French M (2011) Measures of adult pain: Visual Analog Scale for Pain (VAS Pain), Numeric Rating Scale for Pain (NRS Pain), McGill Pain Questionnaire (MPQ), Short-Form McGill Pain Questionnaire (SF-MPQ), Chronic Pain Grade Scale (CPGS), Short Form-36 Bodily Pain Scale (SF-36 BPS), and Measure of Intermittent and Constant Osteoarthritis Pain (ICOAP). Arthritis Care Res (Hoboken) 63(Suppl 11):S240–S252
Recart A, Duchene D, White PF, Thomas T, Johnson DB, Cadeddu JA (2005) Efficacy and safety of fast-track recovery strategy for patients undergoing laparoscopic nephrectomy. J Endourol 19:1165–1169
Conaghan P, Maxwell-Armstrong C, Bedforth N et al (2010) Efficacy of transversus abdominis plane blocks in laparoscopic colorectal resections. Surg Endosc 24:2480–2484
Zafar N, Davies R, Greenslade GL, Dixon AR (2010) The evolution of analgesia in an ‘accelerated’ recovery programme for resectional laparoscopic colorectal surgery with anastomosis. Colorectal Dis 12:119–124
Johns N, O’Neill S, Ventham NT, Barron F, Brady RR, Daniel T (2012) Clinical effectiveness of transversus abdominis plane (TAP) block in abdominal surgery: a systematic review and meta-analysis. Colorectal Dis 14:e635–e642
Siddiqui MR, Sajid MS, Uncles DR, Cheek L, Baig MK (2011) A meta-analysis on the clinical effectiveness of transversus abdominis plane block. J Clin Anesth 23:7–14
Favuzza J, Brady K, Delaney CP (2013) Transversus abdominis plane blocks and enhanced recovery pathways: making the 23-h hospital stay a realistic goal after laparoscopic colorectal surgery. Surg Endosc 27:2481–2486
Walter CJ, Maxwell-Armstrong C, Pinkney TD et al (2013) A randomised controlled trial of the efficacy of ultrasound-guided transversus abdominis plane (TAP) block in laparoscopic colorectal surgery. Surg Endosc 27:2366–2372
Keller DS, Ermlich BO, Delaney CP (2014) Demonstrating the benefits of transversus abdominis plane blocks on patient outcomes in laparoscopic colorectal surgery: review of 200 consecutive cases. J Am Coll Surg 219:1143–1148
Ris F, Findlay JM, Hompes R et al (2014) Addition of transversus abdominis plane block to patient controlled analgesia for laparoscopic high anterior resection improves analgesia, reduces opioid requirement and expedites recovery of bowel function. Ann R Coll Surg Engl 96:579–585
Tong YC, Kaye AD, Urman RD (2014) Liposomal bupivacaine and clinical outcomes. Best Pract Res Clin Anaesthesiol 28:15–27
Acknowledgments
The authors acknowledge Madhu Ragupathi MD for data collection.
Funding
The authors received no funding or financial support for this project.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Dr. Haas is a consultant for Pacira Pharmaceuticals, Inc. Drs. Keller, Tahilramani, Flores-Gonzalez, and Ibarra have no relevant conflicts of interest and nothing to disclose.
Rights and permissions
About this article
Cite this article
Keller, D., Tahilramani, R., Flores-Gonzalez, J. et al. Pilot study of a novel pain management strategy: evaluating the impact on patient outcomes. Surg Endosc 30, 2192–2198 (2016). https://doi.org/10.1007/s00464-015-4459-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-015-4459-4