Abstract
Background
The optimal opioid-sparing analgesic regimen following laparoscopic colorectal surgery (LCS) remains uncertain. We sought to determine the efficacy of low-dose bupivacaine infusion via surgeon-inserted modified continuous transversus abdominis plane (mcTAP) catheters after LCS.
Methods
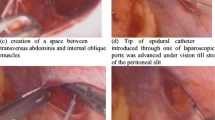
A parallel-group, placebo-controlled, randomized single-centre trial was conducted between April 2017 and February 2018. Block-of-four randomization and allocation concealment by sequentially-numbered, opaque sealed envelopes were used. Patients, surgeons and assessors were blinded. Fifty-two patients were randomized to receive either 0.2% bupivacaine or saline through mcTAP catheters. A 5 ml bolus followed by a 72 h infusion at 2 ml/h was started, with patient-controlled fentanyl analgesia and oral paracetamol given on demand. Primary outcomes were fentanyl consumptions in the first 24 h, second 24 h, and third 24 h following surgery. Secondary outcomes were pain numeric rating scores, recovery outcomes and complications.
Results
Twenty-five patients in the bupivacaine group and 26 in the control group were analysed. Patients in the bupivacaine group required significantly less fentanyl overall (106.1 vs 484.5 mcg, p < 0.001) and at all time points (first 24 h: 61.0 vs 324.3 mcg, p < 0.001; second 24 h: 36.3 vs 119.0 mcg, p = 0.033; third 24 h: 8.8 vs 41.2, p = 0.030) when compared to placebo. Significantly lower pain scores at rest at 6 h (2.32 vs 4.0, p = 0.002), and 12 h (1.80 vs 3.08, p = 0.011) and on coughing at 6 h (4.56 vs 5.84, p = 0.019), 12 h (3.76 vs 4.96, p = 0.009), and 24 h (3.44 vs 4.24, p = 0.049) as well as significantly lower opioid-related complications such as nausea or vomiting (9 (36%) vs 1 (4%), p = 0.005) were observed in the bupivacaine group. There were no major block-related complications, and recovery outcomes were similar in both groups.
Conclusions
McTAP block reduces postoperative fentanyl consumption and pain scores after LCS, highlighting its role as a safe and useful opioid-sparing analgesia.
Registration number
TCTR20150831001 (Thai Clinical Trials Registry). Full trial protocol can be assessed at https://www.clinicaltrials.in.th/.




Similar content being viewed by others
References
Gustafsson UO, Scott MJ, Schwenk W et al (2012) Guidelines for perioperative care in elective colonic surgery: Enhanced Recovery After Surgery (ERAS) Society recommendations. Clin Nutr 31:783–800
Sarin A, Litonius ES, Naidu R et al (2016) Successful implementation of an Enhanced Recovery After Surgery program shortens length of stay and improves postoperative pain, and bowel and bladder function after colorectal surgery. BMC Anesthesiol 16:55
Walter CJ, Maxwell-Armstrong C, Pinkney TD et al (2013) A randomised controlled trial of the efficacy of ultrasound-guided transversus abdominis plane (TAP) block in laparoscopic colorectal surgery. Surg Endosc 27:2366–2372
Pedrazzani C, Menestrina N, Moro M et al (2016) Local wound infiltration plus transversus abdominis plane (TAP) block versus local wound infiltration in laparoscopic colorectal surgery and ERAS program. Surg Endosc 30:5117–5125
Park JS, Choi GS, Kwak KH et al (2015) Effect of local wound infiltration and transversus abdominis plane block on morphine use after laparoscopic colectomy: a nonrandomized, single-blind prospective study. J Surg Res 195:61–66
Rashid A, Gorissen KJ, Ris F et al (2017) No benefit of ultrasound-guided transversus abdominis plane blocks over wound infiltration with local anaesthetic in elective laparoscopic colonic surgery: results of a double-blind randomized controlled trial. Colorectal Dis 19:681–689
Fustran N, Dalmau A, Ferreres E et al (2015) Postoperative analgesia with continuous wound infusion of local anaesthesia vs saline: a double-blind randomized, controlled trial in colorectal surgery. Colorectal Dis 17:342–350
Ventham NT, O'Neill S, Johns N et al (2014) Evaluation of novel local anesthetic wound infiltration techniques for postoperative pain following colorectal resection surgery: a meta-analysis. Dis Colon Rectum 57:237–250
Oh TK, Lee SJ, Do SH et al (2018) Transversus abdominis plane block using a short-acting local anesthetic for postoperative pain after laparoscopic colorectal surgery: a systematic review and meta-analysis. Surg Endosc 32:545–552
Hain E, Maggiori L, AlDJ P et al (2018) Transversus abdominis plane (TAP) block in laparoscopic colorectal surgery improves postoperative pain management: a meta-analysis. Colorectal Dis 20:279–287
McDonnell JG, O'Donnell BD, Farrell T et al (2007) Transversus abdominis plane block: a cadaveric and radiological evaluation. Reg Anesth Pain Med 32:399–404
Mineo R, Sharrock NE (1992) Venous levels of lidocaine and bupivacaine after midtarsal ankle block. Reg Anesth 17:47–49
Abdallah FW, Laffey JG, Halpern SH et al (2013) Duration of analgesic effectiveness after the posterior and lateral transversus abdominis plane block techniques for transverse lower abdominal incisions: a meta-analysis. Br J Anaesth 111:721–735
Boulind CE, Ewings P, Bulley SH et al (2013) Feasibility study of analgesia via epidural versus continuous wound infusion after laparoscopic colorectal resection. Br J Surg 100:395–402
Hafizoglu MC, Katircioglu K, Ozkalkanli MY et al (2008) Bupivacaine infusion above or below the fascia for postoperative pain treatment after abdominal hysterectomy. Anesth Analg 107:2068–2072
Yndgaard S, Holst P, Bjerre-Jepsen K, Thomsen CB, Struckmann J, Mogensen T (1994) Subcutaneously versus subfascially administered lidocaine in pain treatment after inguinal herniotomy. Anesth Analg 79(2):324–327
Ventham NT (2018) Continuous wound infiltration. In: Krige A, Scott MJP (eds) Analgesia in major abdominal surgery. Springer International Publishing, Cham, pp 217–232
Moore SE, Reid KC, Draganic BD et al (2012) Randomized clinical trial of ropivacaine wound infusion following laparoscopic colorectal surgery. Tech Coloproctol 16:431–436
Aboelela M, Kandeel AR, Elsayed U et al (2018) Dexmedetomidine in a surgically inserted catheter for transversus abdominis plane block in donor hepatectomy: a prospective randomized controlled study. Saudi J Anaesth 12:297–303
Jankovic ZB, Pollard SG, Nachiappan MM (2009) Continuous transversus abdominis plane block for renal transplant recipients. Anesth Analg 109:1710–1711
Parikh BK, Waghmare V, Shah VR et al (2015) The analgesic efficacy of continuous transversus abdominis plane block in renal transplant recipients. J Anaesthesiol Clin Pharmacol 31:531–534
Schulz KF, Altman DG, Moher D (2010) CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. BMJ 340:c332
Morarach P, Haruethaivijitchock P (2018) Analgesic effectiveness of modified continuous transversus abdominis plane block with low dose of Local anesthetic continuous infusion in closure loop stoma. Thai J Anesth 44:79–84
Rao Kadam V, Van Wijk RM, Moran JL et al (2017) Continuous transversus abdominis plane block vs intermittent bolus for analgesia after abdominal surgery: a randomized trial. J Pain Res 10:1705–1712
Ganapathy S, Sondekoppam RV, Terlecki M et al (2015) Comparison of efficacy and safety of lateral-to-medial continuous transversus abdominis plane block with thoracic epidural analgesia in patients undergoing abdominal surgery: a randomised, open-label feasibility study. Eur J Anaesthesiol 32:797–804
Yoshida T, Furutani K, Watanabe Y et al (2016) Analgesic efficacy of bilateral continuous transversus abdominis plane blocks using an oblique subcostal approach in patients undergoing laparotomy for gynaecological cancer: a prospective, randomized, triple-blind, placebo-controlled study. Br J Anaesth 117:812–820
Carney J, Finnerty O, Rauf J et al (2011) Studies on the spread of local anaesthetic solution in transversus abdominis plane blocks. Anaesthesia 66:1023–1030
Griffiths JD, Le NV, Grant S et al (2013) Symptomatic local anaesthetic toxicity and plasma ropivacaine concentrations after transversus abdominis plane block for Caesarean section. Br J Anaesth 110:996–1000
Kahokehr AA (2013) Intraperitoneal wound in abdominal surgery. World J Crit Care Med 2:1–3
Tsai HC, Yoshida T, Chuang TY et al (2017) Transversus abdominis plane block: an updated review of anatomy and techniques. Biomed Res Int. 2017:8284363
Dierking GW, Dahl JB, Kanstrup J et al (1992) Effect of pre- vs postoperative inguinal field block on postoperative pain after herniorrhaphy. Br J Anaesth 68:344–348
Mishra AK, Afzal M, Mookerjee SS, Bandyopadhyay KH, Paul A (2013) Pre-emptive analgesia: recent trends and evidences. Indian J Pain 27:114–120
Knudson RA, Dunlavy PW, Franko J et al (2016) Effectiveness of liposomal bupivacaine in colorectal surgery: a pragmatic nonsponsored prospective randomized double blinded trial in a community hospital. Dis Colon Rectum 59:862–869
Kendall MC, Castro Alves LJ, De Oliveira G Jr. (2018) Liposome bupivacaine compared to plain local anesthetics to reduce postsurgical pain: an updated meta-analysis of randomized controlled trials. Pain Res Treat 2018:5710169
Stokes AL, Adhikary SD, Quintili A et al (2017) Liposomal bupivacaine use in transversus abdominis plane blocks reduces pain and postoperative intravenous opioid requirement after colorectal surgery. Dis Colon Rectum 60:170–177
Felling DR, Jackson MW, Ferraro J et al (2018) Liposomal bupivacaine transversus abdominis plane block versus epidural analgesia in a colon and rectal surgery enhanced recovery pathway: a randomized clinical trial. Dis Colon Rectum 61:1196–1204
Acknowledgements
The authors would like to express our gratitude to Prof. Somrat Chaluluxananan, Head of Department of Anesthesiology, Chulalongkorn University, for his advice and guidance.
Funding
The authors have no sources of funding to declare for this manuscript.
Author information
Authors and Affiliations
Contributions
All authors/co-authors meet the four author criteria as defined by ICMJE. Conception or design of work: PH, CS, GT, JT. Data acquisition, analysis, interpretation: all authors. Drafting work, critical revision: all authors. Final approval: all authors. Agreement to be accountable: all authors.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Haruethaivijitchock, P., Ng, J.L., Taksavanitcha, G. et al. Postoperative analgesic efficacy of modified continuous transversus abdominis plane block in laparoscopic colorectal surgery: a triple-blind randomized controlled trial. Tech Coloproctol 24, 1179–1187 (2020). https://doi.org/10.1007/s10151-020-02311-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10151-020-02311-9