Abstract
Background
Energy devices can result in devastating complications to patients. Yet, they remain poorly understood by trainees and surgeons. A single-institution pilot study suggested that structured simulation improves knowledge of the safe use of electrosurgery (ES) among trainees (Madani et al. in Surg Endosc 28(10):2772–2782, 2014). The purpose of this study was to estimate the extent to which the addition of this structured bench-top simulation improves ES knowledge across multiple surgical training programs.
Methods
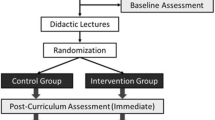
Trainees from 11 residency programs in Canada, the USA and UK participated in a 1-h didactic ES course, based on SAGES’ Fundamental Use of Surgical Energy™ (FUSE) curriculum. They were then randomized to one of two groups: an unstructured hands-on session where trainees used ES devices (control group) or a goal-directed hands-on training session (Sim group). Pre- and post-curriculum (immediately and 3 months after) knowledge of the safe use of ES was assessed using separate examinations. Data are expressed as mean (SD) and N (%), *p < 0.05.
Results
A total of 289 (145 control; 144 Sim) trainees participated, with 186 (96 control; 90 Sim) completing the 3-month assessment. Baseline characteristics were similar between the two groups. Total score on the examination improved from 46 % (10) to 84 % (10)* for the entire cohort, with higher post-curriculum scores in the Sim group compared with controls [86 % (9) vs. 83 % (10)*]. All scores declined after 3 months, but remained higher in the Sim group [72 % (18) vs. 64 % (15)*]. Independent predictors of 3-month score included pre-curriculum score and participation in a goal-directed simulation.
Conclusions
This multi-institutional study confirms that a 2-h curriculum based on the FUSE program improves surgical trainees’ knowledge in the safe use of ES devices across training programs with various geographic locations and resident volumes. The addition of a structured interactive bench-top simulation component further improved learning.


Similar content being viewed by others
References
Health devices: top 10 health technology hazards for 2011. ECRI Institute (2010)
Sankaranarayanan G, Resapu RR, Jones DB, Schwaitzberg S, De S (2013) Common uses and cited complications of energy in surgery. Surg Endosc 27:3056–3072
Govekar HR, Robinson TN, Varosy PD, Girard G, Montero PN, Dunn CL, Jones EL, Stiegmann GV (2012) Effect of monopolar radiofrequency energy on pacemaker function. Surg Endosc 26:2784–2788
Jones EL, Robinson TN, McHenry JR, Dunn CL, Montero PN, Govekar HR, Stiegmann GV (2012) Radiofrequency energy antenna coupling to common laparoscopic instruments: practical implications. Surg Endosc 26:3053–3057
Nduka CC, Super PA, Monson JR, Darzi AW (1994) Cause and prevention of electrosurgical injuries in laparoscopy. J Am Coll Surg 179:161–170
Cormier B, Nezhat F, Sternchos J, Sonoda Y, Leitao MM Jr (2012) Electrocautery-associated vascular injury during robotic-assisted surgery. Obstet Gynecol 120:491–493
Feldman LS, Fuchshuber P, Jones DB, Mischna J, Schwaitzberg SD, Force FT (2012) Surgeons don’t know what they don’t know about the safe use of energy in surgery. Surg Endosc 26:2735–2739
Madani A, Watanabe Y, Vassiliou MC, Fuchshuber P, Jones DB, Schwaitzberg SD, Fried GM, Feldman LS (2014) Impact of a hands-on component on learning in the Fundamental Use of Surgical Energy (FUSE) curriculum: a randomized-controlled trial in surgical trainees. Surg Endosc 28:2772–2782
Feldman L, Fuchshuber P, Jones D (2012) The SAGES manual on the Fundamental Use of Surgical Energy (FUSE). Springer, New York
Sutherland LM, Middleton PF, Anthony A, Hamdorf J, Cregan P, Scott D, Maddern GJ (2006) Surgical simulation: a systematic review. Ann Surg 243:291–300
Scott DJ, Bergen PC, Rege RV, Laycock R, Tesfay ST, Valentine RJ, Euhus DM, Jeyarajah DR, Thompson WM, Jones DB (2000) Laparoscopic training on bench models: better and more cost effective than operating room experience? J Am Coll Surg 191:272–283
Seymour NE, Gallagher AG, Roman SA, O’Brien MK, Bansal VK, Andersen DK, Satava RM (2002) Virtual reality training improves operating room performance: results of a randomized, double-blinded study. Ann Surg 236:458–463 discussion 463-454
Andreatta PB, Woodrum DT, Birkmeyer JD, Yellamanchilli RK, Doherty GM, Gauger PG, Minter RM (2006) Laparoscopic skills are improved with LapMentor training: results of a randomized, double-blinded study. Ann Surg 243:854–860 discussion 860-853
Anastakis DJ, Regehr G, Reznick RK, Cusimano M, Murnaghan J, Brown M, Hutchison C (1999) Assessment of technical skills transfer from the bench training model to the human model. Am J Surg 177:167–170
Palter VN, Orzech N, Reznick RK, Grantcharov TP (2013) Validation of a structured training and assessment curriculum for technical skill acquisition in minimally invasive surgery: a randomized controlled trial. Ann Surg 257:224–230
Pape-Koehler C, Immenroth M, Sauerland S, Lefering R, Lindlohr C, Toaspern J, Heiss M (2013) Multimedia-based training on Internet platforms improves surgical performance: a randomized controlled trial. Surg Endosc 27:1737–1747
Acknowledgments
We acknowledge the SAGES FUSE task force for the development of the FUSE curriculum and presentation slides, as well as the facilitators who assisted in conducting the electrosurgery course. This study was funded by a SAGES Research Grant (#188). A.M. is supported by the Quebec Health Science Research Scholarship (FRQ-S) and the McGill Surgeon-Scientist Program. The Steinberg-Bernstein Centre for Minimally Invasive Surgery and Innovation is supported by an unrestricted educational grant from Covidien©.
Disclosures
Dr. Liane Feldman received an unrestricted educational grant from ConMed. Drs. Amin Madani, Yusuke Watanabe, Nicole Townsend, Philip H. Pucher, Thomas N. Robinson, Patricia E. Egerszegi, Jaisa Olasky, Sharon L. Bachman, Chan W. Park, Nalin Amin, David T. Tang, Erika Haase, Davide Bardana, Daniel B. Jones, Melina Vassiliou and Gerald M. Fried MD have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Madani, A., Watanabe, Y., Townsend, N. et al. Structured simulation improves learning of the Fundamental Use of Surgical Energy™ curriculum: a multicenter randomized controlled trial. Surg Endosc 30, 684–691 (2016). https://doi.org/10.1007/s00464-015-4260-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-015-4260-4