Abstract
Background
This study aimed to quantify the clinical parameters of mono- and bipolar instruments that inhibit pacemaker function. The specific aims were to quantify pacer inhibition resulting from the monopolar instrument by altering the generator power setting, the generator mode, the distance between the active electrode and the pacemaker, and the location of the dispersive electrode.
Methods
A transvenous ventricular lead pacemaker overdrive paced the native heart rate of an anesthetized pig. The primary outcome variable was pacer inhibition quantified as the number of beats dropped by the pacemaker during 5 s of monopolar active electrode activation.
Results
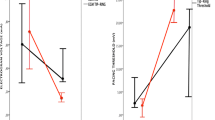
Lowering the generator power setting from 60 to 30 W decreased the number of dropped paced events (2.3 ± 1.2 vs 1.6 ± 0.8 beats; p = 0.045). At 30 W of power, use of the cut mode decreased the number of dropped paced beats compared with the coagulation mode (0.6 ± 0.5 vs 1.6 ± 0.8; p = 0.015). At 30 W coagulation, firing the active electrode at different distances from the pacemaker generator (3.75, 7.5, 15, and 30 cm) did not change the number of dropped paced beats (p = 0.314, analysis of variance [ANOVA]). The dispersive electrode was placed in four locations (right/left gluteus, right/left shoulder). More paced beats were dropped when the current vector traveled through the pacemaker/leads than when it did not (1.5 ± 1.0 vs 0.2 ± 0.4; p < 0.001).
Conclusions
Clinical parameters that reduce the inhibition of a pacemaker by monopolar instruments include lowering the generator power setting, using cut (vs coagulation) mode, and locating the dispersive electrode so the current vector does not traverse the pacemaker generator or leads.

Similar content being viewed by others
References
Greenspon AJ, Patel JD, Lau E, Ochoa JA, Frisch DR, Ho RT, Pavri BB, Kurtz SM (2011) 16-Year trends in the infection burden for pacemakers and implantable cardioverter–defibrillators in the United States 1993 to 2008. J Am Coll Cardiol 58:1001–1006
Rozner MA (2007) The patient with a cardiac pacemaker or implanted defibrillator and management during anaesthesia. Curr Opin Anaesthesiol 20:261–268
Crossley GH, Poole JE, Rozner MA, Asirvatham SJ, Cheng A, Chung MK, Ferguson TB Jr, Gallagher JD, Gold MR, Hoyt RH, Irefin S, Kusumoto FM, Moorman LP, Thompson A (2011) The Heart Rhythm Society (HRS)/American Society of Anesthesiologists (ASA) Expert Consensus Statement on the perioperative management of patients with implantable defibrillators, pacemakers, and arrhythmia monitors: facilities and patient management. This document was developed as a joint project with the American Society of Anesthesiologists (ASA), and in collaboration with the American Heart Association (AHA) and the Society of Thoracic Surgeons (STS). Heart Rhythm 8:1114–1154
American Society of Anesthesiologists Task Force on Perioperative Management of Patients with Cardiac Implantable Electronic Devices (2011) Practice advisory for the perioperative management of patients with cardiac implantable electronic devices: pacemakers and implantable cardioverter–defibrillators: an updated report. Anesthesiology 114:247–261
Massarweh NN, Cosgriff N, Slakey DP (2006) Electrosurgery: history, principles, and current and future uses. J Am Coll Surg 202:520–530
Guertin D, Faheem O, Ling T, Pelletier G, McComas D, Yarlagadda RK, Clyne C, Kluger J (2007) Electromagnetic Interference (EMI) and arrhythmic events in ICD patients undergoing gastrointestinal procedures. Pacing Clin Electrophysiol 30:734–739
Cheng A, Nazarian S, Spragg DD, Bilchick K, Tandri H, Mark L, Halperin H, Calkins H, Berger RD, Henrikson CA (2008) Effects of surgical and endoscopic electrocautery on modern-day permanent pacemaker and implantable cardioverter–defibrillator systems. Pacing Clin Electrophysiol 31:344–350
Disclosures
Thomas N. Robinson has received honoraria from ConMed Electrosurgery and Covidien for teaching the topic of electrosurgery. He has an educational grant from Gyrus and a research grant from Medtronic. Guillaume Girard is a current employee of Medtronic, Inc. Henry R. Govekar, Paul D. Varosy, Paul N. Montero, Christina L. Dunn, Edward L. Jones, and Greg V. Stiegmann have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Govekar, H.R., Robinson, T.N., Varosy, P.D. et al. Effect of monopolar radiofrequency energy on pacemaker function. Surg Endosc 26, 2784–2788 (2012). https://doi.org/10.1007/s00464-012-2279-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-012-2279-3