Abstract
Background
Mesh use during hiatal hernia repair (HHR) has been suggested to be safe and effective. Concern has been raised about the risk of mesh-related complications, and the higher risk of complications if revisional hiatal surgery is undertaken after mesh has been used. Available data have not established a clear role for mesh in HHR. To assess surgeons’ adoption of the use of mesh for HHR, SAGES members were surveyed regarding their practice related to mesh use for HHR.
Methods
Between April and September 2010, an internet-based survey tool was used to survey SAGES members. Potential participants were contacted via e-mail and invited to complete the survey. Of the 5,323 attempted contacts, 5,024 reached active e-mail accounts. From these, 2,518 members responded (50% response rate).
Results
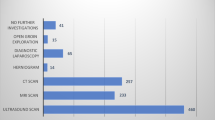
The majority of respondents currently perform HHR (69%), but only 18% perform more than 20 per year. Of those who perform HHR, 94% use a laparoscopic approach for the majority of repairs. Whereas 25% of surgeons use mesh for the majority of repairs, 23% of surgeons never use mesh. When mesh is used, an absorbable mesh is most commonly used (67%). An onlay technique is used by 93% of respondents. Only 7% of surgeons who have been in practice more than 20 years use mesh compared with 59% of surgeons in practice less than 10 years. Fifty-seven percent of surgeons have never performed revisional foregut surgery on a patient with prior mesh.
Conclusions
Although the majority of surgeons have used mesh for HHR, it is the minority who use it routinely, with younger surgeons more likely to use mesh than older surgeons. Absorbable mesh is most commonly used. When mesh is used, an onlay technique is most commonly used. There is no clear accepted use of mesh in hiatal hernia repair.





Similar content being viewed by others
References
Curci JA, Melman LM, Thompson RW, Soper NJ, Matthews BD (2008) Elastic fiber depletion in the supporting ligaments of the gastroesophageal junction: a structural basis for the development of hiatal hernia. J Am Coll Surg 207:191–196
Mattar SG, Bowers SP, Galloway KD, Hunter JG, Smith CD (2002) Long-term outcome of laparoscopic repair of paraesophageal hernia. Surg Endosc 16:745–749
Hashemi M, Peters JH, DeMeester TR, Huprich JE, Quek M, Hagen JA, Crookes PF, Theisen J, DeMeester SR, Sillin LF, Bremner CG (2000) Laparoscopic repair of large type III hiatal hernia: objective followup reveals high recurrence rate. J Am Coll Surg 190:553–560
Granderath FA, Granderath UM, Pointner R (2008) Laparoscopic revisional fundoplication with circular hiatal mesh prosthesis: the long-term results. World J Surg 32:999–1007
Granderath FA, Schweiger UM, Kamolz T, Asche KU, Pointner R (2005) Laparoscopic Nissen fundoplication with prosthetic hiatal closure reduces postoperative intrathoracic wrap herniation: preliminary results of a prospective randomized functional and clinical study. Arch Surg 140:40–48
Lee YK, James E, Bochkarev V, Vitamvas M, Oleynikov D (2008) Long-term outcomes of cruroplasty reinforcement with human acellular dermal matrix in large paraesophageal hiatal hernia. J Gastrointest Surg 12:811–815
Oelschlager BK, Pellegrini CA, Hunter J, Soper N, Brunt M, Sheppard B, Jobe B, Polissar N, Mitsumori L, Nelson J, Swanstrom L (2006) Biologic prosthesis reduces recurrence after laparoscopic paraesophageal hernia repair: a multicenter, prospective, randomized trial. Ann Surg 244:481–490
Tatum RP, Shalhub S, Oelschlager BK, Pellegrini CA (2008) Complications of PTFE mesh erosion at the diaphragmatic hiatus. J Gastrointest Surg 12:953–957
Stadlhuber RJ, Sherif AE, Mittal SK, Fitzgibbons RJ, Brunt LM, Hunter JG, Demeester TR, Swanstrom LL, Smith CD, Filipi CJ (2009) Mesh complications after prosthetic reinforcement of hiatal closure: a 28-case series. Surg Endosc 23:1219–1226
Parker M, Bowers SP, Bray JM, Harris AS, Belli EV, Pfluke JM, Preissler S, Asbun HJ, Smith CD (2010) Hiatal mesh is associated with major resection at revisional operation. Surg Endosc 24:3095–3101
Dutta S (2007) Prosthetic esophageal erosion after mesh hiatoplasty in a child, removed by transabdominal endogastric surgery. J Pediatr Surg 42:252–256
Herqueta-Delgado P, Marin-Moreno M, Morales-Conde S, Reina-Serrano S, Jurado-Castillo C, Pellicer-Bautista F, Herrerias-Gutierrez JM (2006) Transmural migration of a prosthetic mesh after surgery of a paraesophageal hernia. Gastrointest Endosc 64:120–121
Hazebroek EJ, Liebman S, Smith GS (2009) Erosion of a composite PTFE/ePTFE mesh after hiatal hernia surgery. Surg Laparosc Endosc Percutan Tech 19:175–177
Kepenekci I, Turkcapar AG (2009) Mesh erosion as a complication of laparoscopic fundoplication with prosthetic hiatal closure: report of a case. Surg Laparosc Endosc Percut Tech 10:e51–e54
Zehetner J, Demeester SR, Ayazi S, Kilday P, Augustin F, Hagen JA, Lipham JC, Sohn HJ, Demeester TR (2011) Laparoscopic versus open repair of paraesophageal hernia: the second decade. J Am Coll Surg (Epub ahead of print)
Luketich JD, Nason KS, Christie NA, Pennathur A, Jobe BA, Landreneau RJ, Schuchert MJ (2010) Outcomes after a decade of laparoscopic giant paraesophageal hernia repair. J Thorac Cardiovasc Surg 139:395–404
Frantzides CT, Carlson MA, Loizides S, Papafili A, Luu M, Roberts J, Zeni T, Frantzides A (2009) Hiatal hernia repair with mesh: a survey of SAGES members. Surg Endosc 24:1017–1024
Acknowledgments
The authors thank Ian S. Warshak for assistance with data collection.
Disclosures
Drs. Pfluke, Parker, Bowers, Asbun, and Smith have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pfluke, J.M., Parker, M., Bowers, S.P. et al. Use of mesh for hiatal hernia repair: a survey of SAGES members. Surg Endosc 26, 1843–1848 (2012). https://doi.org/10.1007/s00464-012-2150-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-012-2150-6