Abstract
Background
The objective of this review was to provide an overview of the components that comprise each of the eight barrier mesh prostheses commonly utilized for LVHR and to review the current literature related to the characteristics and effectiveness of these materials to guide the general surgeon in selecting the most appropriate material for LVHR.
Methods
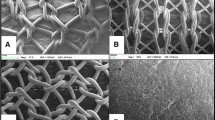
Composite prostheses with permanent barriers (Bard™ Composix™ E/X, Bard™ Composix™ L/P, and DUALMESH® Biomaterial) were compared to composite prostheses with absorbable barriers (C-QUR™ Mesh, PROCEED™ Surgical Mesh, Bard™ Sepramesh™ IP Composite, Parietex™ Composite, and PHYSIOMESH™) using scanning electron microscopy and a review of the current preclinical and clinical literature.
Results
Clinical studies and preclinical animal models have attempted to determine the adhesion characteristics and effectiveness of barrier mesh prostheses available for ventral hernia repair applications. However, it is difficult to make any definitive statements about the adhesion characteristics and effectiveness of these materials because all meshes were not included in all studies and likewise not compared under identical conditions. Overall, Parietex™ Composite and DUALMESH® Biomaterial were cited most frequently for improvement of adhesion characteristics, followed closely by Bard™ Sepramesh™ IP Composite and C-QUR™ Mesh. Bard™ Composix™, PROCEED™ Surgical Mesh, and uncoated polypropylene were cited most frequently as having the most tenacious and extensive adhesions.
Conclusions
Differences observed between the various barrier prostheses are likely attributable to the chemical composition of the barrier or the conditions required for resorption and metabolism of the barrier components. It is likely that the components of these barriers incite a wide range of inflammatory responses resulting in the range of adhesion coverage and tenacity observed in the preclinical and clinical studies reviewed. Clinical trials are needed to more appropriately define the clinical effectiveness of these barriers.


Similar content being viewed by others
References
Burger JW, Luijendijk RW, Hop WC, Halm JA, Verdaasdonk EG, Jeekel J (2004) Long-term follow-up of a randomized controlled trial of suture versus mesh repair of incisional hernia. Ann Surg 240:578–583
Heniford BT, Park A, Ramshaw BJ, Voeller G (2003) Laparoscopic repair of ventral hernias: nine years’ experience with 850 consecutive hernias. Ann Surg 238:391–399
Pierce RA, Spitler JA, Frisella MM, Matthews BD, Brunt LM (2007) Pooled data analysis of laparoscopic vs. open ventral hernia repair: 14 years of patient data accrual. Surg Endosc 21:378–386
Ray NF, Denton WG, Thamer M, Henderson SC, Perry S (1998) Abdominal adhesiolysis: inpatient care and expenditures in the United States in 1994. J Am Coll Surg 186:1–9
Gray SH, Vick CC, Graham LA, Finan KR, Neumayer LA, Hawn MT (2008) Risk of complications from enterotomy or unplanned bowel resection during elective hernia repair. Arch Surg 143:582–586
Halm JA, de Wall LL, Steyerberg EW, Jeekel J, Lange JF (2007) Intraperitoneal polypropylene mesh hernia repair complicates subsequent abdominal surgery. World J Surg 31:423–429
Usher FC, Ochsner J, Tuttle LJ (1958) Use of Marlex mesh in the repair of incisional hernias. Am Surg 24:969–974
(2007) PROCEED Surgical mesh instructions for use
(2005) Sepramesh IP composite instructions for use
Pierce RA, Perrone J, Nimeri A, Sexton J, Walcutt J, Frisella M, Matthews B (2009) 120-day comparative analysis of adhesion grade and quantity, mesh contraction, and tissue response to a novel omega-3 fatty acid bioabsorbable barrier macroporous mesh after intraperitoneal placement. Surg Innov 16:46–54
(2011) PHYSIOMESH instructions for use. Ethicon, Inc
Tingstedt B, Isaksson K, Andersson E, Andersson R (2007) Prevention of abdominal adhesions—present state and what’s beyond the horizon? Eur Surg Res 39:259–268
Schreinemacher MH, Emans PJ, Gijbels MJ, Greve JW, Beets GL, Bouvy ND (2009) Degradation of mesh coatings and intraperitoneal adhesion formation in an experimental model. Br J Surg 96:305–313
(2005) Bard* Composix E/X mesh instructions for use
(2006) Composix L/P instructions for use. CR Bard
Deeken CR, Abdo MS, Frisella MM, Matthews BD (2011) Physicomechanical evaluation of absorbable and nonabsorbable barrier composite meshes for laparoscopic ventral hernia repair. Surg Endosc 25:1541–1552
(2007) DualMesh biomaterial instructions for use
(2008) Gore DUALMESH PLUS biomaterial instructions for use
Fox C et al (1991) Infection-resistant compositions, medical devices and surfaces and methods for preparing the same. U.S. Patent #5019096
Ratner BD, Hoffman AS, Schoen FJ, Lemons JE (2004) Biomaterials science. Academic Press, San Diego
Laurent TC (1987) Biochemistry of hyaluronan. Acta Otolaryngol Suppl 442:7–24
Turaev A (1995) Dependence of the biodegradability of carboxymethylcellulose on its supermolecular structure and molecular parameters. Chem Nat Compds 31:254–259
Yamaoka T, Tabata Y, Ikada Y (1995) Fate of water-soluble polymers administered via different routes. J Pharm Sci 84:349–354
Earle DB, Mark LA (2008) Prosthetic material in inguinal hernia repair: how do I choose? Surg Clin North Am 88:179–201
(2009) C-QUR mesh instructions for use
(2007) What is atrium’s omega-3–coated mesh and what happens following implantation? Atrium Medical Corp Technical Data Report No 010. http://www.atriummed.com/EN/Biosurgery/cqur-data.asp
Kabara J, Swieczkowski D, Conley AJ, Truant J (1972) Fatty acids and derivatives as antimicrobial agents. Antimicrob Agents Chemother 2:23–28
Thormar H, Isaacs CE, Brown HR, Barshatzky MR, Pessolano T (1987) Inactivation of enveloped viruses and killing of cells by fatty acids and monoglycerides. Antimicrob Agents Chemother 31:27–31
Ferrucci L, Cherubini A, Bandinelli S, Bartali B, Corsi A, Lauretani F, Martin A, Andres-Lacueva C, Senin U, Guralnik JM (2006) Relationship of plasma polyunsaturated fatty acids to circulating inflammatory markers. J Clin Endocrinol Metab 91:439–446
Arita M, Yoshida M, Hong S, Tjonahen E, Glickman JN, Petasis NA, Blumberg RS, Serhan CN (2005) Resolvin E1, an endogenous lipid mediator derived from omega-3 eicosapentaenoic acid, protects against 2,4,6-trinitrobenzene sulfonic acid-induced colitis. Proc Natl Acad Sci USA 102:7671–7676
(2010) Parietex composite instructions for use
Ory F et al (2002) Composite prosthesis for preventing post-surgical adhesions and method for obtaining same. U.S. Patent #09463313
Tayot J et al (2002) Collagenic material useful in particular for preventing post-operative adhesions. U.S. Patent #6391939
van Amerongen MJ, Harmsen MC, Petersen AH, Kors G, van Luyn MJ (2006) The enzymatic degradation of scaffolds and their replacement by vascularized extracellular matrix in the murine myocardium. Biomaterials 27:2247–2257
Campbell M (1995) Biochemistry. Saunders, New York
Boland ED, Coleman BD, Barnes CP, Simpson DG, Wnek GE, Bowlin GL (2005) Electrospinning polydioxanone for biomedical applications. Acta Biomater 1:115–123
Pillai CK, Sharma CP (2010) Review paper: absorbable polymeric surgical sutures: chemistry, production, properties, biodegradability, and performance. J Biomater Appl 25:291–366
Ashton W et al (1968) Oxidized cellulose product and method for preparing the same. U.S. Patent #3364200
Boardman F et al (1993) Cellulose oxidation by a perfluoronated hydrocarbon solution of nitrogen dioxide. U.S. Patent #5180398
Wiseman D et al (2003) Bioabsorbable medical devices from oxidized polysaccharides. U.S. Patent #20030073663
Dimitrijevich SD, Tatarko M, Gracy RW, Linsky CB, Olsen C (1990) Biodegradation of oxidized regenerated cellulose. Carbohydr Res 195:247–256
Dimitrijevich SD, Tatarko M, Gracy RW, Wise GE, Oakford LX, Linsky CB, Kamp L (1990) In vivo degradation of oxidized, regenerated cellulose. Carbohydr Res 198:331–341
Nary FH, Matsumoto MA, Batista AC, Lopes LC, de Goes FC, Consolaro A (2002) Comparative study of tissue response to polyglecaprone 25, polyglactin 910 and polytetrafluoroethylene suture materials in rats. Braz Dent J 13:86–91
Arnaud JP, Hennekinne-Mucci S, Pessaux P, Tuech JJ, Aube C (2003) Ultrasound detection of visceral adhesion after intraperitoneal ventral hernia treatment: a comparative study of protected versus unprotected meshes. Hernia 7:85–88
Cobb WS, Harris JB, Lokey JS, McGill ES, Klove KL (2003) Incisional herniorrhaphy with intraperitoneal composite mesh: a report of 95 cases. Am Surg 69:784–787
Koehler RH, Begos D, Berger D, Carey S, LeBlanc K, Park A, Ramshaw B, Smoot R, Voeller G (2003) Minimal adhesions to ePTFE mesh after laparoscopic ventral incisional hernia repair: reoperative findings in 65 cases. JSLS 7:335–340
Leber GE, Garb JL, Alexander AI, Reed WP (1998) Long-term complications associated with prosthetic repair of incisional hernias. Arch Surg 133:378–382
Jenkins ED, Yom V, Melman L, Brunt LM, Eagon JC, Frisella MM, Matthews BD (2010) Prospective evaluation of adhesion characteristics to intraperitoneal mesh and adhesiolysis-related complications during laparoscopic re-exploration after prior ventral hernia repair. Surg Endosc 24:3002–3007
Chelala E, Debardemaeker Y, Elias B, Charara F, Dessily M, Alle JL (2010) Eighty-five redo surgeries after 733 laparoscopic treatments for ventral and incisional hernia: adhesion and recurrence analysis. Hernia 14:123–129
Wassenaar EB, Schoenmaeckers EJ, Raymakers JT, Rakic S (2010) Subsequent abdominal surgery after laparoscopic ventral and incisional hernia repair with an expanded polytetrafluoroethylene mesh: a single institution experience with 72 reoperations. Hernia 14:137–142
Duffy AJ, Hogle NJ, LaPerle KM, Fowler DL (2004) Comparison of two composite meshes using two fixation devices in a porcine laparoscopic ventral hernia repair model. Hernia 8:358–364
McGinty JJ, Hogle NJ, McCarthy H, Fowler DL (2005) A comparative study of adhesion formation and abdominal wall ingrowth after laparoscopic ventral hernia repair in a porcine model using multiple types of mesh. Surg Endosc 19:786–790
Jacob BP, Hogle NJ, Durak E, Kim T, Fowler DL (2007) Tissue ingrowth and bowel adhesion formation in an animal comparative study: polypropylene versus proceed versus parietex composite. Surg Endosc 21:629–633
Gonzalez R, Rodeheaver GT, Moody DL, Foresman PA, Ramshaw BJ (2004) Resistance to adhesion formation: a comparative study of treated and untreated mesh products placed in the abdominal cavity. Hernia 8:213–219
Gaertner WB, Bonsack ME, Delaney JP (2010) Visceral adhesions to hernia prostheses. Hernia 14:375–381
Kayaoglu HA, Ozkan N, Hazinedaroglu SM, Ersoy OF, Erkek AB, Koseoglu RD (2005) Comparison of adhesive properties of five different prosthetic materials used in hernioplasty. J Invest Surg 18:89–95
Matthews BD, Mostafa G, Carbonell AM, Joels CS, Kercher KW, Austin C, Norton HJ, Heniford BT (2005) Evaluation of adhesion formation and host tissue response to intra-abdominal polytetrafluoroethylene mesh and composite prosthetic mesh. J Surg Res 123:227–234
Matthews BD, Pratt BL, Pollinger HS, Backus CL, Kercher KW, Sing RF, Heniford BT (2003) Assessment of adhesion formation to intra-abdominal polypropylene mesh and polytetrafluoroethylene mesh. J Surg Res 114:126–132
Novitsky YW, Harrell AG, Cristiano JA, Paton BL, Norton HJ, Peindl RD, Kercher KW, Heniford BT (2007) Comparative evaluation of adhesion formation, strength of ingrowth, and textile properties of prosthetic meshes after long-term intra-abdominal implantation in a rabbit. J Surg Res 140:6–11
Greenawalt KE, Butler TJ, Rowe EA, Finneral AC, Garlick DS, Burns JW (2000) Evaluation of Sepramesh biosurgical composite in a rabbit hernia repair model. J Surg Res 94:92–98
Acknowledgments
The authors acknowledge the efforts of Hilda Kabiru and Jocelyn Prowse at Atrium Medical Corporation for technical expertise and assistance with the scanning electron micrographs.
Disclosures
Dr. Deeken is a consultant for Atrium Medical Corporation and Davol Incorporated. Dr. Faucher is an employee of Atrium Medical Corporation. Dr. Matthews is a consultant for Atrium Medical Corporation and Ethicon Incorporated. He also receives honoraria and research/equipment support from Atrium Medical Corporation, Ethicon EndoSurgery, Karl Storz Endoscopy, Stryker Endoscopy, and W.L. Gore & Associates, Incorporated.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Deeken, C.R., Faucher, K.M. & Matthews, B.D. A review of the composition, characteristics, and effectiveness of barrier mesh prostheses utilized for laparoscopic ventral hernia repair. Surg Endosc 26, 566–575 (2012). https://doi.org/10.1007/s00464-011-1899-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-011-1899-3