Abstract
Glycerol derivatives are a class of compounds, which are easy and inexpensive to produce with potent anti-malarial activities against blood stages of Plasmodium falciparum in vitro. In the present study, one of these compounds, termed 1t, which had the lowest IC50 values, was assessed in a murine malarial model. Nuclear magnetic resonance imaging and Balb/c mice infected with Plasmodium berghei ANKA strain were treated in a 4-day suppressive test. Mice received a once-daily intraperitoneal administration of 50 mg/Kg of the drug for 4 days. Although no parasitaemia clearance was reached, a slower parasite proliferation and a slightly longer survival time compared with the placebo group were observed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Despite substantial efforts to control malaria, chemotherapy of the causative agent Plasmodium falciparum is limited by increasing drug resistance to anti-malarial drugs used as first line treatment and is worsened by the lack of novel treatment options (Guinovart et al. 2006). In the absence of vaccines, new chemotherapies are urgently needed to help in prevention and control. Development of anti-malarials can follow several strategies, ranging from minor modifications of existing agents to the design of novel agents that act against new targets. Parasite-specific transport processes are of potential importance because they may become new drug targets or may be used as uptake routes of cytotoxic drugs into the parasite cell (Pavlovic-Djuranovic et al. 2006). In previous publications, P. falciparum aquaglyceroporin was characterised as an attractive target for new malaria chemotherapy because of its uniqueness and conservation in the parasite’s genome (Bahamontes-Rosa et al. 2007; Hansen et al. 2002).
Some new structures based on glycerol and designed to block aquaporins exhibited anti-malarial activity against the intra-erythrocytic stage of P. falciparum in vitro. They were found to be very efficient with a 50% inhibitory concentration (IC50) ranging on the micromolar range in chloroquine-resistant and non-resistant P. falciparum. These compounds are inexpensive to produce, stable and water soluble (Robin et al. 2007).
To demonstrate the full potential of the compound, the anti-malarial properties need to be compared in vivo by using a murine malaria-infected model. Rodent malaria parasites are recognised as valuable model parasites for the investigation of the developmental biology of malaria parasites, parasite–host interactions, vaccine development and drug testing. Plasmodium berghei, isolated from thicket rats from Central Africa, is used in research programs for development and screening of anti-malarial drugs (Fidock et al. 2004).
Here, we conducted an investigation of the in vivo anti-malarial activity of the most active of these compounds in this model.
Materials and methods
Chemicals
The product 1-benzyloxy-3-[(2-thienylmethyl)amino]propan-2-ol named 1t was synthesised by ring opening of (±) benzyl glycidyl ether with 2-thiophenemethylamine (1.5 equivalents) under microwave irradiation (4 min at 140°C, 80 W power; Fig. 1). It was isolated in 84% yield after purification via Kugelrohr bulb to bulb distillation (Robin et al. 2007).
For the biological assays it was dissolved in dimethyl sulfoxide at concentrations of 100 mM and stored at −20°C. In the in vitro test against P. falciparum, it was diluted to a concentration of 100 μM in RPMI-1640 medium (SIGMA, Steinheim, Germany). For the in vivo test, the compound was prepared for intraperitoneally administration (i.p.) at a concentration of 50 mg/Kg as a 50-μl solution containing 7% Tween 80 (SIGMA) and 3% ethanol (Merck, Darmstadt, Germany).
Biological material
Parasite strains
The P. falciparum strains used in this study were three laboratory strains: a chloroquine-sensitive parasite strain (3D7) and two chloroquine-resistant strains (FCR3 and Dd2). Parasites were maintained in continuous culture as previously described (Trager and Jensen 1976).
The rodent malaria parasite was the P. berghei ANKA strain, originally obtained from David Walliker (University of Edinburgh, Edinburgh, UK) and maintained as cryopreserved stabilates. When needed, the parasites were thawed and injected i.p. into a donor mouse. Four days later, blood obtained from this mouse served to generate the inoculum used to infect the experimental mice.
Mice
Twelve female albino outbred Naval Medical Research Institute (NMRI) mice about 4 weeks of age and 14 male albino inbred Balb/c mice about 7 weeks of age were purchased from Harlan Winkelmann GmbH (Borchen, Germany). Animals were maintained under standard conditions in the animal facilities of the Institute for Tropical Medicine, University of Tübingen. Mice were supplied with food supplemented with p–aminobenzoic acid and water ad libitum.
In vitro drug susceptibility assay
P. falciparum drug sensitivity assays were performed by monitoring the accumulation of the parasite protein Histidin-Rich Protein 2 (HRPII) in the culture after lysis of the parasite cells. Quantification of HRPII was assessed by a double-site antigen capture ELISA as previously described (Robin et al. 2007). The photometric readings obtained and the corresponding log drug concentrations were fitted to a dose-response curve model using an automated curve-fitting analytical software (Table Curve 2D version 4). The results were expressed as the drug concentration resulting in 50%, 90% and 99% inhibition of parasite growth (IC50, IC90, IC99).
Assessment of drug toxicity in mice
Toxicity was determined after a daily i.p. single-drug injection during 4 days of 1t (50 mg/Kg) into two naive NMRI mice. Absence of toxicity was defined as survival after treatment. Change of body mass and haemoglobin levels were followed for 15 days.
In vivo drug susceptibility assay
In vivo anti-malarial activity of the compound 1t was determined against the rodent malaria P. berghei ANKA strain according to a 4-day suppressive test (Ancelin et al. 1994). The experiment was performed independently twice: first with ten NMRI mice and secondly with 14 Balb/c mice. Two experimental groups were created: a group treated with 50 mg/Kg of 1t or with placebo (7% Tween 80 and 3% ethanol). Each animal was used only for one treatment and was randomly assigned to one experimental group containing five NMRI or seven Balb/c mice per group.
NMRI mice were inoculated i.p. with 108 parasitised red blood cells (pRBC; resuspended in saline medium) and Balb/c mice with 106 pRBC. Two hours post-infection the animals were treated i.p. with a single dose of 1t or with placebo. The experimental groups were treated again i.p. with the same dose of drug or placebo at 24, 48 and 72 h post-infection. Survival of the mice was monitored daily.
Mice were weighted daily in a digital gram scale during the first 7 days and every 2 days until they die. Changes in body mass were calculated in relation to the initial measurements made for each mouse. Zeroes, thus, represent no change, positive values represent gains and negative represent loss.
Tail blood was taken to determine parasitaemia and haemoglobin levels daily during the first 7 days and every 2 days until mice died. The haemoglobin levels were measured by absorbance at 540 nm with a Uvikon Spectrophotometer 930 (Kontron, Neufahrn, Germany) of 4 μl of tail-vain blood suspended in 996 μl Drabkin’s reagent (SIGMA, Steinheim, Germany) and is expressed as a percentage of baseline levels.
Parasitaemia was assessed by thin blood smears stained with 20% Giemsa stain solution (SIGMA) in phosphate buffer pH 7.2 and visualised under a light microscope (Nikon Eclipse E200). A minimum of 1,000 erythrocytes per slide was counted.
The inhibitory rate of the drug was expressed as [(Parasitaemia in placebo group − Parasitaemia in drug treated group)/(Parasitaemia in placebo group) × 100%] (Su et al. 2003).
The course of P. berghei infection and the signs or symptoms of malaria complications were reported daily. Disease severity was quantified in terms of haemoglobin and body weight loss.
Statistical analyses
Analyses were performed by using StatView for Windows 5.0.1 (SAS Institute Inc., Cary, NC, USA) running on Windows XP (Microsoft Corp., Redmond, WA, USA). Parasitaemia, body mass and haemoglobin levels were expressed as mean ± SD. The Kaplan–Meier analysis was selected for the survival analysis. Two group comparisons were performed with the nonparametric Mann–Whitney U test. The level of significance was set at P value of <0.05.
Results
In vitro drug susceptibility assay
Compound 1t was active against both QR and QS parasite strains with low IC values and was also effective against the multi-drug resistant Dd2 strain (Table 1). The enantiomers compounds (8b and 9b) had the same inhibitory effect, similar to that of the racemic mixtures (Table 1 and see (Robin et al. 2007)). Therefore, 1t was selected as lead compound for the further in vivo test.
Assessment of drug toxicity in mice
Despite compound 1t was not toxic against three different human cell lines (Robin et al. 2007) to assess the possible toxicity in mice, two naive NMRI non-infected mice were injected during 4 days with one single-drug injection of 1t (50 mg/Kg). Mice survived the treatment and during the 15 days of the follow-up, animals increased the body mass as expected and no obvious secondary effects were observed (data not shown).
In vivo anti-malarial activity of 1t against P. berghei
The compound 1t was tested in mice infected with P. berghei ANKA according to a version of a 4-day suppressive test (Ancelin et al. 1994). Compounds were administered i.p. once daily during 4 days, with the first drug administered 2 h after i.p. parasite inoculation.
A first experiment with ten female NMRI was done. The survival time on average was 17.2 days for the treated group and 14.8 days for the placebo group. Two mice (40%) of the treatment group died at day 6 and one (20%) in the placebo group at day 9 with signs of cerebral malaria (Fig. 2a). The neurological manifestations included hemi- or paraplegia, tendency to roll over on stimulation, ataxia and convulsions. At the day of death, parasitaemia levels were low and levels of haemoglobin as well as body mass although reduced were not significantly different from the control mice (data not shown).
In the treatment group, three mice (60%) died at the days 19, 27 and 28 with severe anaemia, hyperparasitaemia and without neurological signs. In the placebo group, four mice (80%) survived for 16 days on average (range between days 15 and 18) and also developed severe anaemia and hyperparasitaemia (Fig. 2a). The levels of parasitaemia in those mice rose steadily throughout the course of the infection, with a peak from 66% to 95% at the time of death (data not shown). Infection-related differences in anaemia like loss of body mass or reduction in haemoglobin levels across the experiment was recorded (Fig. 3). The levels of haemoglobin in peripheral blood and the body mass decreased in both groups but with statistically significant differences only on weight at day 12 (p 12 = 0.034; Fig. 3a).
Anti-malarial activity of 1t in P. berghei-infected mice as a function of change in body mass, haemoglobin levels and parasitemia. a NMRI mice were inoculated i.p. with 108 P. berghei-infected erythrocytes at day 0 and treated at days 0, 1, 2 and 3 with 1t (50 mg/Kg; filled square) or placebo (empty square). The body mass decreased in both groups but with significant differences only at day 12 (p 12 = 0.034). b Balb/c mice were inoculated i.p. with 106 P. berghei-infected erythrocytes at day 0 and treated at days 0, 1, 2 and 3 with 1t (50 mg/Kg; filled square) or placebo (empty square). Significant differences in change of body mass were observed at days 3, 4 and 5 (p 3 = 0.035, p 4 = 0.007 and p 5 = 0.007, respectively)
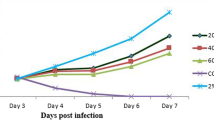
Parasitaemia in the treatment group at days 1, 2 and 3, when the mice were still treated daily, was low having an increasing inhibitory rate from 0% to 25% and 27% (Table 2). Immediately after treatment (day 4) parasitaemia of the treatment group was still lower than the placebo group with an inhibitory rate of 26%, although in the following 2 days, parasitaemia in the treatment group increased and the inhibitory rate became negative (Table 2). Even though not significantly, parasitaemia in the placebo group had a tendency to increase after day 12 faster than the treated group (Fig. 3a).
To avoid cerebral complication, a second experiment with Balb/c mice that are not susceptible to develop cerebral malaria was performed. Each experimental group contained seven mice and all died before day 25. At the end of the second week after infection, one mouse (14%) in the treatment and two mice (29%) in the placebo group, respectively, died with haematuria. The rest of the mice (n = 6 in the treatment group and n = 5 in the placebo group) died with severe anaemia and hyperparasitaemia in the following days. Mice survived 18.6 and 18.1 days on average in the treatment and in the placebo group, respectively (Fig. 2b). As observed before, the levels of parasitaemia rose steadily throughout the course of the infection, with a peak from 31% to 98% at the time of death (data not shown). The levels of haemoglobin in peripheral blood and the body mass decreased in both groups but with significant differences only on weight at days 3, 4 and 5 (p 3 = 0.035, p 4 = 0.007 and p 5 = 0.007, respectively; Fig. 3b).
The inhibitory rate in the treatment group at days 2 and 3 was 24% and 40%, respectively (Table 2). Immediately after treatment (day 4), parasitaemia were equal in both groups and the inhibitory rate, therefore, became 0. In the following day (day 5), the inhibitory rate became negative, but at day 6, it increased again to 19% (Table 2). Although no statistically significant differences were registered in parasitaemia, it had a tendency to increase faster after day 14 in the placebo group (Fig. 3b). Both groups behaved equally in the decrease of haemoglobin and body mass (Fig. 3b).
Discussion
Glycerol analogues were found to be highly active in vitro against P. falciparum (Robin et al. 2007). One compound, termed 1t, was reported to inhibit the proliferation of chloroquine-resistant and sensitive strains in vitro with low inhibitory concentrations (Robin et al. 2007). To demonstrate the full potential of the compound, their anti-malarial properties were compared in vivo. We, thus, used the murine malaria parasite P. berghei (Fidock et al. 2004).
In the present study, the compound 1t was unable to clear parasitaemia in infected mice. NMRI mice died in a biphasic pattern of survival which has been described in rodent malaria models (Jennings et al. 1998;Lou et al. 2001). Animals that develop cerebral manifestations fall ill in the first 6 to 9 days of infection. They die with paralysis and coma with a parasitaemia averaging 10%. Animals that survive the early phase of infection develop hyperparasitaemia and die from severe anaemia during week three and four of infection (Lou et al. 2001). Cerebral malaria is only induced in susceptible strains of mice by injection of virulent P. berghei ANKA blood stages parasites. NMRI mice developed neurological complications since they are susceptible to cerebral malaria (Jennings et al. 1998;Lou et al. 2001). However, NMRI mice treated with 1t showed longer survival time when compared with the placebo group.
Because Balb/c mice are not susceptible to cerebral malaria, no cerebral case was found. Mice developed hyperparasitaemia and die with severe anaemia. The presence of haematuria presented in several mice is associated with intravascular haemolysis because of a heavy parasitaemia (Boonpucknavig and Sitprija 1979). Although the compound 1t was not able to cure the infected mice with P. berghei, a slight prolonged survival time was observed. The compound 1t achieved a high level of activity in vitro against P. falciparum, but a potent in vivo anti-malarial activity was not achieved. In the murine model, the anti-malarial activity of the compound 1t was not completely successful. However, the absence of toxicity, the strong effect in vitro and the slightly improved survival in mice still makes this class of compounds promising anti-malarials for further study.
References
Ancelin ML, Vial HJ, Calas M, Giral L, Piquet G, Rubi E, Thomas A, Peters W, Slomianny C, Herrera S (1994) Present development concerning anti-malarial activity of phospholipid metabolism inhibitors with special reference to in vivo activity. Mem Inst Oswaldo Cruz 89 Suppl 2:85–90
Bahamontes-Rosa N, Wu B, Beitz E, Kremsner PG, Kun JF (2007) Limited genetic diversity of the Plasmodium falciparum aquaglyceroporin gene. Mol Biochem Parasitol 156(2):255–257
Boonpucknavig V, Sitprija V (1979) Renal disease in acute Plasmodium falciparum infection in man. Kidney Int 16:44–52
Fidock DA, Rosenthal PJ, Croft SL, Brun R, Nwaka S (2004) Anti-malarial drug discovery: efficacy models for compound screening. Nat Rev Drug Discov 3:509–520
Guinovart C, Navia MM, Tanner M, Alonso PL (2006) Malaria: burden of disease. Current Molecular Medicine 6:137–140
Hansen M, Kun JF, Schultz JE, Beitz E (2002) A single, bi-functional aquaglyceroporin in blood-stage Plasmodium falciparum malaria parasites. J Biol Chem 277:4874–4882
Jennings VM, Lal AA, Hunter RL (1998) Evidence for multiple pathologic and protective mechanisms of murine cerebral malaria. Infect Immun 66:5972–5979
Lou J, Lucas R, Grau GE (2001) Pathogenesis of cerebral malaria: recent experimental data and possible applications for humans. Clin Microbiol Rev 14:810–820, table
Pavlovic-Djuranovic S, Kun JF, Schultz JE, Beitz E (2006) Dihydroxyacetone and methylglyoxal as permeants of the Plasmodium aquaglyceroporin inhibit parasite proliferation. Biochim Biophys Acta 1758:1012–1017
Robin A, Brown F, Bahamontes-Rosa N, Wu B, Beitz E, Kun JF, Flitsch SL (2007) Microwave-assisted ring opening of epoxides: a general route to the synthesis of 1-aminopropan-2-ols with anti malaria parasite activities. J Med Chem 50:4243–4249
Su RB, Wei XL, Liu Y, Li J (2003) Anti-malarial effect of agmatine on Plasmodium berghei K173 strain. Acta Pharmacol Sin 24:918–922
Trager W, Jensen JB (1976) Human malaria parasites in continuous culture. Science 193:673–675
Acknowledgements
This study was supported by the European Commission (LSHP-CT-2004-012189). We are also grateful to Gennadij Trabant for excellent assistance with the mice.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bahamontes-Rosa, N., Bucher, K., Held, J. et al. In vivo anti-malarial effect of the ß-amino alcohol 1t on Plasmodium berghei . Parasitol Res 104, 1459–1464 (2009). https://doi.org/10.1007/s00436-009-1348-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00436-009-1348-6