Abstract
Purpose
The aim of our study was to evaluate if therapeutic success in the first-line of anticancer treatments in patients with NSCLC may predict treatment success in the following lines.
Methods
We analyzed the data of patients with NSCLC stage III/IV from the TULUNG registry separately for chemotherapy, TKIs, ALK inhibitors, and immunotherapy in the first line during the years 2011–2019. „Succesful treatment “ was defined as PFS ≥ 6 months, a „good responder “ was a patient with ˃50% of „successful treatment “ lines. Treatment responses were analyzed separately for each drug group. Descriptive statistics, Fisher exact test, Pearson Chi-Squared test, log-rank test, and univariate/multivariate logistic regression models were used.
Results
The first-line TKI therapy was successful in 66.2%, while good responders accounted for 50.7% of the cohort and their rates were similar for all types of TKIs. First-line platinum-based chemotherapy was successful in 43.1% and 48.6% for combinations with pemetrexed and bevacizumab, respectively. Good responders accounted for 29.5% and 25.9%, respectively. In the group of ALK inhibitors, we observed treatment success in 52.3% of cases, while alectinib showed the highest effectiveness (up to 70%). Good responders constituted 50% of the group. In the first-line immunotherapy group, survival benefit was observed in 52.3%, and good responders constituted 52.3% of the cohort.
Conclusion
We concluded that the treatment success in first-line therapies in patients with NSCLC may predict survival benefits in the subsequent lines, particularly in EGFR- or ALK-positive disease and immunotherapy-treated patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
By the 2020s, lung cancer remains one of the most serious cancer diseases, claiming millions of lives worldwide. Despite notable progress in understanding lung cancer pathobiology, further therapeutic improvements are desired. Novel targeted treatments emerged during the last decade and the most apparent progress in treatment outcomes has been achieved in non-squamous non-small cell lung cancer (NSCLC). Importantly, the introduction of novel therapies resulted also in increased opportunities for treatment sequencing in multiple treatment lines.
In daily practice, the real-life effectiveness of various treatments may differ from the efficacy reported from clinical trials (Brat et al. 2020; Cramer-van der Welle et al. 2018), e.g., overall survival (OS) and progression-free survival (PFS) rates for pemetrexed, bevacizumab and tyrosine kinase inhibitors (TKIs) were higher than pooled OS and PFS from clinical trials in our previous study (Brat et al. 2020). Favorable treatment outcomes may be related to the existence of „good responders “—patients benefitting from most types of anticancer therapy. Understanding several new molecular pathways resulted in an increased opportunity for treatment response prediction; however, the relationships in sequenced multilinear treatment are more complex and poorly understood. Some patients with NSCLC respond favorably to multiple treatments and can be generally considered „good responders “. To date, we lack specific biomarkers of good treatment response and favorable outcomes within the use of multiple treatment lines.
The effectiveness of first-line anticancer therapy could be one of such aspects as demonstrated in a study by Bonotto et al. (Bonotto et al. 2015). In this study, the authors demonstrated that a 6-month benefit with the first line of anticancer treatment was associated with benefits in the second and further lines in patients with breast cancer (Bonotto et al. 2015). Among the modern-era treatments of NSCLC, pemetrexed is the oldest and most explored regime. A relation between response to the previous treatment line and subsequent treatment success with pemetrexed therapy has been described also in patients with NSCLC (Sun et al. 2010). Similarly, sensitivity to pemetrexed predicted therapeutic benefits from further treatment lines (Park et al. 2019).
In this study, we focused on various classes of first-line anticancer treatments in patients with NSCLC, including platinum-based chemotherapy, tyrosine kinase inhibitors (TKIs), anaplastic lymphoma kinase (ALK) inhibitors, and immunotherapy (IO). Our aim was to evaluate if therapeutic success with certain types of first-line anticancer treatments may predict treatment success in the following lines. We hypothesized that treatment success within first-line therapies may predict the probability of treatment success with subsequent lines.
Methods
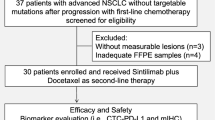
Subjects
The source of the large-scale data was the TULUNG Registry (a joint registry of the Czech Pneumological Society, the Czech Society for Oncology, and the Institute of Biostatistics and Analyses, Ltd.), a prospective multicenter database of patients with advanced-stage NSCLC treated by modern-era treatments including antifolates, biological agents and/or immunotherapy.
Briefly, the TULUNG registry encompasses prospective data of NSCLC patients from 11 tertiary- or university-type healthcare centers in the Czech Republic. Written informed consent was signed by each patient sharing his/her anonymized data with the scientific community. Patient participation in the study was voluntary. The following data were collected: demography (age, sex, weight, height, body mass index, performance status, race), smoking history, main comorbidities, lung cancer histology, disease stage at time of diagnosis (using the 7th TNM classification) (Mirsadraee et al. 2012), molecular genetic profile (mainly mutation status of EGFR gene), the use of anticancer treatments (including dosage, adverse events and main reasons of treatment discontinuation), radiotherapy or lung surgery, and survival data (overall survival, progression-free survival). The data were collected continuously, and updated regularly on at least twice a year basis.
Statistics
For this study, we analyzed data of patients with an anticancer treatment initiated between July 1st, 2011 (the foundation of the TULUNG Registry) and December 31st, 2019. The data were analyzed separately for each group of first-line anticancer treatment (chemotherapy, TKIs, ALK inhibitors, and immunotherapy).
Treatment responses were analyzed using the RECIST 1.1 criteria (Eisenhauer et al. 2009). Overall survival (OS) was defined as the time from anticancer treatment initiation to (all-cause) death. Progression-free survival (PFS) was defined as the time from anticancer treatment initiation to the date of first documented disease progression or all-cause death. OS and PFS were estimated using the Kaplan–Meier method and all estimates at various time points included a 95% confidence interval (CI).
„Succesful treatment “ was defined as reaching progression-free survival (PFS) of ≥ 6 months. A „good responder “ was defined as a patient with ˃50% of „successful treatment “ lines of all recorded. Accordingly, a „poor responder “ was defined as a patient with less than 50% of „successful treatment “ lines of all. Treatment responses for each particular drug were analyzed separately and also on a group basis for TKIs, chemotherapy, ALK inhibitors, and IO.
The basic characteristics of the cohort were described by descriptive statistics. Continuous variables were described by means and 95% CI and by medians with minimum and maximum values. Categorical variables were presented as absolute and relative frequencies. Relative frequencies were calculated based on the number of patients in the treatment subgroups. Comparisons between groups were made by the Fisher exact test and Pearson Chi-Squared test.
Differences in PFS were tested by the Log-rank test. Univariate and multivariate logistic regression models were constructed for good and bad responders.
Statistical analyses were performed using IBM SPSS, Statistics (version 25.0), and R software (version 3.5.1).
Ethics
The study has been approved by the institutional ethics committees of all centers participating in the TULUNG registry (University Hospital Brno, University Hospital Pilsen, University Hospital Olomouc, University Hospital Hradec Kralove, University Hospital Motol (Prague), University Hospital Prague-Bulovka, Thomayer Hospital (Prague), University Hospital Ostrava, Hospital Jihlava, Masaryk Memorial Cancer Institute (Brno) and VFN (Prague)). This particular study was approved by the Ethics Committee of the University Hospital Hradec Kralove on May 11th, 2018, reference number: 201805 I134R.
Results
We analyzed data from a total of 2317 patients with advanced-stage NSCLC treated in the first line of their anticancer therapy by afatinib (180 patients), gefitinib (340 patients), erlotinib (60 patients), platinum-based chemotherapy plus pemetrexed (1204 patients), platinum-based chemotherapy plus bevacizumab (451 patients), alectinib (24 patients), crizotinib (14 patients), or pembrolizumab (44 patients).
Tyrosine kinase inhibitors
Five hundred and eighty patients were treated by TKIs during the study period, including 66.2% women with a mean age of 65.9 years and a mean BMI of 26.2 kg/m2. Eastern Cooperative Oncology Group performance status (ECOG PS) was mostly 0–1, stage IV patients represented the majority of the cohort. Adverse events (AEs) were reported in 29.7% of cases (Table 1).
The first-line therapy was successful in 66.2% while the effectiveness of further lines gradually decreased with increasing treatment lines. No differences in the effectiveness of individual TKIs were observed across the lines (Table 2). Good responders for the TKIs group accounted for 50.7% of the cohort and their rates were similar for all TKIs. The probability of a ≥ 6-month PFS after a TKI did not differ for any of the TKIs. The ten most frequent treatment patterns/sequences are presented in Table 3. Of the EGFR mutations, the deletion in exon 19 dominated (53.1% of all patients), while the L858R mutation in exon 21 was less frequent with 26%, and other mutations (the T790M and other rare mutations) constituted a total of 26.4% (Table 4). The proportion of EGFR mutations was similar/balanced in all TKI subgroups (Table 4). In the multivariate analysis, age and Exon 19 deletion were the only factors independently associated with being a good responder while former smoking was associated with a poor responder (Supplementary Table 1).
The subgroup of patients treated by osimertinib in the second line included a significantly higher proportion of patients with a 6-month benefit (60.5%) (Supplementary Table 2), as well as good responders (55%) (Supplementary Table 3) when compared to patients on platinum-based chemotherapy (41.9% and 34.5%) or other treatment (mostly chemo-monotherapy) (34.6% and 28%; p = 0.021 and <0.001, respectively).
Chemotherapy with pemetrexed or bevacizumab
Chemotherapeutic regimens with pemetrexed or bevacizumab were used in 1655 patients, of these 58.9% were men with a mean age of 63.1 years and a mean BMI of 26.3 kg/m2. Most patients were diagnosed with stage IV disease and had an initial ECOG PS 0-1. Treatment AEs were reported in 13.5% of patients (Table 1).
The rate of patients with a ≥ 6-month PFS with first-line pemetrexed- or bevacizumab-based regimens was 43.1% and 48.6%, respectively. In the pemetrexed subgroup, we observed 29.5% of good responders, while only 25.9% in the bevacizumab-based regimen subgroup. There was no difference between the two subgroups regarding survival benefit in any of the subsequent lines, i.e., the effectiveness was similar for both regimens (Table 5). The ten most frequent treatment sequences/patterns are presented in Table 6. In the multivariate analysis, age was associated with a good responder, while higher ECOG PS at treatment initiation with a poor responder (Supplementary Table 4).
For the second line of treatment, there was no significant difference in the proportion of patients with a 6-month benefit among groups with immunotherapy, platinum-based chemotherapy, and other treatments (mostly chemo-monotherapy, e.g., docetaxel, gemcitabine, and vinorelbine) (Supplementary Table 5). On the other hand, in the first-line chemotherapy group, we observed a higher proportion of good responders in the second line with IO and platinum-based chemotherapy compared to the subgroup of chemo-monotherapy (24.7% and 33.7% vs 15.5%, respectively, p < 0.001) (Supplementary Table 6).
ALK inhibitors
In the studied period, alectinib or crizotinib was used in the first line of anticancer treatment in thirty-six ALK-positive patients. In this group, men constituted 31.6% of the cohort, with a mean age of 61.2 years and a mean BMI of 26.1 kg/m2. Unlike in other treatment groups, 68.4% were non-smokers. Initial stage IV disease was diagnosed in 94.7% of patients (Table 1).
Alectinib was significantly more effective than crizotinib in the first-line therapy of ALK-positive patients (Table 7). Good responders constituted 50% of the entire group; however, the result was largely driven by alectinib (66.7% of good responders compared to 21.4% for crizotinib, p = 0.007). The six most common treatment sequences/patterns are presented in Table 8. Age was the only independent factor of a poor responder with ALK inhibitors (Supplementary Table 7).
Immunotherapy (IO)
From 2011 to 2019, pembrolizumab was the only first-line check-point inhibitor available for use in the Czech Republic for patients with a stage IV NSCLC with PD-L1 expression of ˃50%. Pembrolizumab monotherapy was initiated in 44 patients during the study period. In this group, men accounted for 59.1% of the cohort, the mean age was 66.4 years, and the mean BMI was 27.1 kg/m2. All patients were diagnosed with stage IV. AEs of IO were observed in 22.7% of patients (Table 1).
First-line survival benefit (≥ 6-month PFS) was observed in 52.3% of patients. Treatment benefit from the second line was the same and good responders constituted 52.3% of the cohort (Table 9). The treatment sequences/patterns are presented in Table 10. In the multivariate analysis, a statistically insignificant trend towards a good responder was observed in former/current smokers and patients experiencing AEs (Supplementary Table 8).
An inter-group comparison of good responders across all treatment groups showed a significantly higher (almost doubled) rate of good responders in groups of biological therapy and IO when compared to the chemotherapy-based groups (Supplementary Table 9).
Discussion
To our best knowledge, this was the first study attempting to assess survival benefits in its complexity during all lines of patients´ anticancer therapies in patients with NSCLC. A similar study has been performed by Bonotto et al. in 2015 (Bonotto et al. 2015). The authors of this study described the most frequent sequences/patterns of anticancer therapies in a cohort of 472 patients with breast cancer and assessed if treatment response of PFS ≥ 6 months within the first line of treatment resulted in a higher probability of survival benefit with further treatment lines. As an extension of this study design, we attempted to assess treatment responses for all lines in groups of patients with NSCLC treated by different first-line therapies.
The main finding of our study was that patients treated by certain groups of anticancer therapies (EGFR inhibitors, ALK inhibitors, IO) had an increased probability of experiencing a ≥ 6-month survival benefit not only in their first line of anticancer treatment but also in subsequent treatment lines. This observation was most apparent in patients treated with alectinib (ALK inhibitor). On the contrary, patients treated with chemotherapy-based regimens experienced the lowest rate of survival benefit in the first and also in the subsequent lines of their anticancer therapies.
The observed favorable outcomes with EGFR inhibitors, ALK inhibitors, and IO have been demonstrated previously in a number of studies.
For both EGFR- and ALK-positive patients, our data showed that the rate of good responders was significantly higher than in the chemotherapy-based group. We speculate that these tumor types may be composed of heterogenic (but dominantly EGFR- or ALK-mutant) cancer cells that are prone to significant treatment response with targeted therapies. Residual cancer tissue may harbor a broader number and spectrum of oncogenic driver mutations with an overall weaker potential for rapid progression of the disease after targeted treatment.
To date, the most frequently used biological therapy in patients with NSCLC is the group of EGFR inhibitors (TKIs). Several predictive markers exist, indicating a potential therapeutic benefit from TKIs. These include Exon 19 deletion as some subtypes of this mutation may have an important clinical impact (Huang et al. 2022) or the plasma level of circulating tumor DNA (ctDNA) as lower ctDNA during the treatment course is associated with better survival (Kallergi et al. 2022; Provencio et al. 2021).
Several TKIs (erlotinib, gefitinib, afatinib, dacomitinib, and osimertinib) can be used in various treatment lines, and also in a sequence. The optimal sequencing strategy appeared to be the combination of afatinib in the first line, followed by second-line osimertinib in a case of a proven T790M mutation (Hirsh et al. 2020; Kim et al. 2023), until the results of the FLAURA study have been published, shifting osimertinib to the first-line therapy of EGFR positive NSCLC (Lorenzi et al. 2022). Exact recommendations on treatment after first- or second-line osimertinib failure were not formulated. Usually, a switch to chemotherapy or chemo-immunotherapy is preferred (Reck et al. 2019). In our study, we found larger numbers of treatment benefits and good responders among patients treated by osimertinib in the second line which is in accordance with current knowledge (Hirsh et al. 2020; Kim et al. 2023).
According to recent studies, PD-L1 expression of ≤ 1% (Lasvergnas et al. 2023) and concomitant genetic mutations AXIN2, P2CG, or RAD51C may predict a poor response to a first-line TKI therapy (Wen et al. 2023). On the other hand, post-treatment TKIs-resistant NSCLC tumors have recently been considered potentially targetable by MET-, HER2-, and HER3-directed therapies (Johnson et al. 2022).
For ALK-positive NSCLC, several ALK inhibitors can be used in a sequence (alectinib, ceritinib, crizotinib, brigatinib, lorlatinib) (Kauffman et al. 2021). Alectinib, brigatinib and lorlatinib, ALK inhibitors with high intracerebral penetration, are recommended as first-line drugs. Lorlatinib is preferred in the second line of treatment post-failure after a second-generation ALK inhibitor (ESMO guidelines 2023; Hochmair et al. 2020). On the other hand, a recent study by Takeyasu et al. found similar effectivity of second-line lorlatinib and pemetrexed-based chemotherapy after failure of alectinib (Takayasu et al. 2022).
After crizotinib failure, a variety of other ALK drugs can be used (ESMO guidelines 2023). Survival of patients with NSCLC harboring ALK mutation and receiving an ALK inhibitor seems to be independent of the fusion variants of ALK translocation (Tabbó et al. 2022). In contrast, other authors discuss worse effectiveness in patients harboring variant 3 of the ALK translocation (Lin et al. 2018). Further studies are needed to uncover the mechanisms of resistance in ALK-mutated NSCLC disease.
Another group of highly effective anticancer treatment for NSCLC is immunotherapy. It gains a still larger therapeutic scope not only in the treatment of NSCLC but also in small-cell lung cancer (SCLC) or malignant pleural mesothelioma. To date, expression of PD-L1 remains the key marker of treatment response to IO (Herbst et al. 2014; Kim et al. 2018). However, new markers of treatment response emerged, including ECOG PS, presence of brain metastases, molecular genetic factors, circulating regulatory T cells, and immune-related adverse events (irAEs). Circulating regulatory T cells are associated with better response during IO and may help to differentiate between disease pseudoprogression and hyperprogression (Kang et al. 2022). As to the molecular genetic factors, patients with a concurrent KRAS- or BRAF-positive disease experienced longer PFS when compared to those with an EGFR- or ALK-positive profile (Bodor et al. 2022). By contrast, ECOG PS ≥ 2 or the presence of brain metastases were associated with early progression of the disease (Dumenil et al. 2018). Patients developing irAEs are known to benefit more significantly compared to those without irAEs; the more irAEs the patient experiences, the higher the probability of a survival benefit from IO (Sonehara et al. 2021).
Similarly to our observation, better survival outcomes after first-line IO have also been reported in a retrospective multicenter study by Bersanelli et al. (Bersanelli et al. 2020). In this study, the authors observed improved survival and ORR after chemotherapy in patients pre-treated with IO, concluding that IO may increase the tumor´s sensitivity to the (subsequent) chemotherapy (Bersanelli et al. 2020). Our data seem to support this hypothesis.
In contrast, low TMB has been found a predictor of responsiveness to first-line chemotherapy (PFS 9.77 vs 6.33 months, HR = 0.523; p = 0.009) (Song et al. 2022) while other authors report the tumor mutation index model (based on total/sensitive TMB from blood and mutation score) as a potential predictor of response to chemotherapy or immunotherapy in the subsequent treatment lines (Lu et al. 2022). Nastase et al. identified a group of genes associated with a good response to platinum chemotherapy in IIIA stage NSCLC (Nastase et al. 2022). Genetic background of treatment response to adjuvant chemotherapy has also been observed in patients with low-stage NSCLC (Van Laar 2012).
In summary, the differences in treatment responses to various classes of first-line anticancer therapies observed in our study likely point out the complexity of mechanisms of tumor pathogenesis in NSCLC. Different tumor subpopulations may coexist in each individual patient, and this may evolve also during the course of their anticancer therapy. Further research is needed to understand the molecular and genetic mechanisms and the broader clinical context beyond our observation.
Limitations
There are several limitations of this study. First, the study is retrospective, however, based on large-scale data that provide relevant information regarding real-life experience with anticancer therapy of NSCLC in the Czech Republic. Second, the data are not fully representative of the entire Czech Republic as it comes from 11 tertiary- or university-type healthcare centers and do not fully represent the situation in the whole Czech healthcare system. Third, we did not differentiate between various types of chemotherapeutic regimens in detail as this would make the interpretation of the results almost impossible. Fourth, the ALK and IO subgroups are relatively small as these therapies were introduced just at the end of the study period. Last, we considered only limited treatment options for the advanced stages of NSCLC. In the study period, chemo/immunotherapy was not used commonly in the first-line anticancer strategy compared to the current clinical practice. Despite these limitations, we consider the presented data strong, generalizable, and representative of the treatment strategies in the Czech Republic.
Conclusion
We concluded that the effectiveness of first-line therapies in patients with NSCLC may predict survival benefit in the subsequent lines, particularly in EGFR-, ALK-, or PD-L1-positive disease treated by targeted therapies. By contrast, chemotherapy-based regimens were associated with the highest rate of poor response in all lines of anticancer treatment. Further studies are needed to uncover and better understand the underlying mechanisms of increased treatment responsiveness in certain subgroups of patients with NSCLC.
Data availability
The datasets generated and/or analyzed during the study are available from the corresponding author on a reasonable request.
References
Bersanelli M, Buti S, Giannarelli D et al (2020) Chemotherapy in non-small cell lung cancer patients after prior immunotherapy: the multicenter retrospective CLARITY study. Lung Cancer 150:123–131
Bodor JN, Bauman JR, Handorf EA et al (2022) Real-world progression-free survival (rwPFS) and the impact of PD-L1 and smoking in driver-mutated non-small cell lung cancer (NSCLC) treated with immunotherapy. J Cancer Res Clin Oncol. Epub ahead of print.
Bonotto M, Gerratana L, Iacono D et al (2015) Treatment of metastatic breast cancer in a real-world scenario: Is progression-free survival with first line predictive of benefit from second and later lines? Oncologist 20(7):719–724
Brat K, Bratova M, Skrickova J et al (2020) Real-life effectiveness of first-line anticancer treatments in stage IIIB/IV NSCLC patients: data from the Czech TULUNG registry. Thorac Cancer 11(11):3346–3356
Clinical practice living guidelines. ESMO Clinical Practice Guidelines for diagnosis, treatment and follow. 2023. https://www.annalsofoncology.org/action/showPdf?pii=S0923-7534%2822%2904781-0. Accessed 19 June 2023.
Cramer-van der Welle CM, Peters BJM, Schramel FMNH et al (2018) Systematic evaluation of the efficacy-effectiveness gap of systemic treatments in metastatic nonsmall cell lung cancer. Eur Respir J 52:1801100
Dumenil C, Massiani MA, Dumoulin J et al (2018) Clinical factors associated with early progression and grade 3–4 toxicity in patients with advanced non-small-cell lung cancers treated with nivolumab. PLoS ONE 13(4):e0195945
Eisenhauer EA, Therasse P and Bogaerts J (2009) New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer 45(2): 228–47.
Herbst RS, Soria JC, Kowanetz M et al (2014) Predictive correlates of response to the anti-PD-L1 antibody MPDL3280A in cancer patients. Nature 515(7528):563–567
Hirsh V, Singh J (2020) Optimal sequencing strategies in the treatment of EGFR mutation-positive non-small cell lung cancer: clinical benefits and cost-effectiveness. Am J Health Syst Pharm 77(18):1466–1476
Hochmair MJ, Fabikan H, Illini O et al (2020) Later-line treatment with lorlatinib in ALK- and ROS1-rearrangement-positive NSCLC: a retrospective. Multicenter Anal Pharmaceuticals 13(11):371
Huang LT, Zhang SL, Han CB et al (2022) Impact of EGFR exon 19 deletion subtypes on clinical outcomes in EGFR-TKI-Treated advanced non-small-cell lung cancer. Lung Cancer 166:9–16
Johnson M, Garassino MC, Mok T et al (2022) Treatment strategies and outcomes for patients with EGFR-mutant non-small cell lung cancer resistant to EGFR tyrosine kinase inhibitors: focus on novel therapies. Lung Cancer 170:41–51
Kallergi G, Kontopodis E, Ntzifa A et al (2022) Effect of osimertinib on CTCs and ctDNA in EGFR mutant non-small cell lung cancer patients: the prognostic relevance of liquid biopsy. Cancers 14(6):1574
Kang DH, Chung C, Sun P et al (2022) Circulating regulatory T cells predict efficacy and atypical responses in lung cancer patients treated with PD-1/PD-L1 inhibitors. Cancer Immunol Immunother 71(3):579–588
Kauffmann-Guerrero D, Kahnert K, Huber RM (2021) Treatment sequencing for anaplastic lymphoma kinase-rearranged non-small-cell lung cancer. Drugs 81(1):87–100
Kim J, Cho J, Lee MH et al (2018) Relative efficacy of checkpoint inhibitors for advanced NSCLC according to programmed death-ligand-1 expression: a systematic review and network meta-analysis. Sci Rep 8(1):11738
Kim T, Jang TW, Choi CM et al (2023) Final report on real-world effectiveness of sequential afatinib and osimertinib in EGFR positive advanced non-small cell lung cancer: updated analysis of the RESET study. Cancer Res Treat. Epub ahead of print.
Lasvergnas J, Fallet V, Duchemann B et al (2023) PDL1-status predicts primary resistance of metastatic, EGFR-mutated non small cell lung cancers to EGFR tyrosine-kinase inhibitors. Respir Med Res 84:101018
Lin JJ, Zhu VW, Yoda S et al (2018) Impact of EML4-ALK variant on resistance mechanisms and clinical outcomes in ALK-positive lung cancer. J Clin Oncol 36(12):1199–1206
Lorenzi M, Ferro A, Cecere F et al (2022) First-line osimertinib in patients with EGFR-mutant advanced non-small cell lung cancer: outcome and safety in the real world: FLOWER study. Oncologist 27(2):87-e115
Lu J, Wu J, Lou Y et al (2022) Blood-based tumour mutation index act as prognostic predictor for immunotherapy and chemotherapy in non-small cell lung cancer patients. Biomark Res 10(1):55
Mirsadraee S, Oswal D, Alizadeh Y (2012) The 7th lung cancer TNM classification and staging system: review of the changes and implications. World J Radiol 28(4):128–134
Nastase A, Dima SO, Lupo A et al (2022) Molecular markers for long-term survival in stage IIIA (N2) NSCLC patients. Cancer Genomics Proteomics 19(1):94–104
Park JH, Kwon BS, Park SJ et al (2019) Exceptional pemetrexed sensitivity can predict therapeutic benefit from subsequent chemotherapy in metastatic non-squamous non-small cell lung cancer. J Cancer Res Clin Oncol 145(7):1897–1905
Provencio M, Serna-Blasco R, Franco F et al (2021) Analysis of circulating tumour DNA to identify patients with epidermal growth factor receptor-positive non-small cell lung cancer who might benefit from sequential tyrosine kinase inhibitor treatment. Eur J Cancer 149:61–72
Reck M, Mok TSK, Nishio M et al (2019) Atezolizumab plus bevacizumab and chemotherapy in non-small-cell lung cancer (IMpower150): key subgroup analyses of patients with EGFR mutations or baseline liver metastases in a randomised, open-label phase 3 trial. Lancet Respir Med 7(5):387–401
Sonehara K, Tateishi K, Araki T et al (2021) The role of immune-related adverse events in prognosis and efficacy prediction for patients with non-small cell lung cancer treated with immunotherapy: a retrospective clinical analysis. Oncology 99(5):271–279
Song J, Yan Y, Chen C et al (2022) Tumor mutational burden and efficacy of chemotherapy in lung cancer. Clin Transl Oncol. Epub ahead of print.
Sun JM, Oh DY, Lee SH et al (2010) The relationship between response to previous systemic treatment and the efficacy of subsequent pemetrexed therapy in advanced non-small cell lung cancer. Lung Cancer 68(3):427–432
Tabbò F, Muscarella LA, Gobbini E et al (2022) Detection of ALK fusion variants by RNA-based NGS and clinical outcome correlation in NSCLC patients treated with ALK-TKI sequences. Eur J Cancer 174:200–211
Takeyasu Y, Yoshida T, Masuda K et al (2022) Lorlatinib versus pemetrexed-based chemotherapy in patients with ALK-rearranged NSCLC previously treated with alectinib. JTO Clin Res Rep 3(5):100311
Van Laar RK (2012) Genomic signatures for predicting survival and adjuvant chemotherapy benefit in patients with non-small-cell lung cancer. BMC Med Genomics 2(5):30
Wen R, Chen Y, Long J et al (2023) Aggressive progression to EGFR tyrosine kinase inhibitors in advanced NSCLC patients: concomitant mutations, prognostic indicator and subsequent management. J Cancer Res Clin Oncol Epub ahead of print.
Funding
The additional statistical analyses have been financed/supported by the Czech Pneumological and Physiological Society.
Author information
Authors and Affiliations
Contributions
MB contributed to data collection, analysis, interpretation, and writing of the manuscript. KB contributed to the interpretation and writing the manuscript. MB and KH contributed to sample processing and evaluation, laboratory analysis, and interpretation of the data. The other authors collected the data in the TULUNG registry and critically revised and approved the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Author MB received speaker and consultant honoraria from Astra Zeneca CZ, Roche CZ, MSD CZ, and Bristol-Myers Squibb CZ. The other authors declare no conflicts of interest relevant to this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Bratova, M., Skrickova, J., Matusikova, M. et al. Effectiveness of first-line anticancer treatment may predict treatment response in further lines in stage III/IV patients with non-small cell lung cancer. J Cancer Res Clin Oncol 149, 17123–17131 (2023). https://doi.org/10.1007/s00432-023-05431-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00432-023-05431-5