Abstract
Purpose
To compare the incidence profile of four major cancers in Australia by place of birth.
Methods
In this retrospective population-based cohort study, the analysis included 548,851 residents diagnosed with primary colorectum, lung, female breast, or prostate cancer during 2005–2014. Incidence rate ratio (IRR) and 95% confidence intervals (CI) were calculated for migrant groups relative to Australian-born.
Results
Compared with Australian-born residents, most migrant groups had significantly lower incidence rates for cancers of the colorectum, breast and prostate. The lowest rates of colorectal cancer were among males born in Central America (IRR = 0.46, 95% CI 0.29–0.74) and females born in Central Asia (IRR = 0.38, 95% CI 0.23–0.64). Males born in North-East Asia had the lowest rates of prostate cancer (IRR = 0.40, 95% CI 0.38–0.43) and females born in Central Asia had the lowest rates of breast cancer (IRR = 0.55, 95% CI 0.43–0.70). For lung cancer, several migrant groups had higher rates than Australian-born residents, with the highest rates among those from Melanesia (males IRR = 1.39, 95% CI 1.10–1.76; females IRR = 1.40, 95% CI 1.10–1.78).
Conclusions
This study describes cancer patterns among Australian migrants, which are potentially helpful in understanding the etiology of these cancers and guiding the implementation of culturally sensitive and safe prevention measures. The lower incidence rates observed for most migrant groups may be maintained with continued emphasis on supporting communities to minimize modifiable risk factors such as smoking and alcohol consumption and participation in organized cancer screening programmes. Additionally, culturally sensitive tobacco control measures should be targeted to migrant communities with high lung cancer incidence rates.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cancer is the leading cause of disease burden in Australia, with cancers of the breast, prostate, colorectum, and lung among the commonest, constituting 45% of all cancers combined in 2018 (Australian Institute of Health and Welfare 2021). The incidence rates of these cancers varied markedly globally, from more than threefold variation in breast cancer, ninefold in colorectal cancer, to over 13-fold in prostate cancer, with Australia/New Zealand among the regions with the highest rates (Sung et al. 2021). Lung cancer, the second commonest cancer globally in 2020, had an over 20-fold variation in incidence between regions (Sung et al. 2021). The underlying drivers of these global patterns are multi-faceted and are likely to be associated with variation in the prevalence of exposures, access to cancer screening and detection technologies, and genetic factors (Australian Institute of Health and Welfare 2021; Sung et al. 2021).
Australia is home to approximately 7.6 million migrants, accounting for 30% of its population (Australian Bureau of Statistics 2021). Over the past several decades, Australia has evolved into a nation of people from over 190 countries and 300 different ancestries (Australian Bureau of Statistics 2021). Due to its diverse population and comprehensive cancer registration (Bray et al. 2017), Australia is well suited for studies of cancer in migrant populations. Prior Australian data showed that migrants to Australia generally have lower rates of many common cancers than native-born Australians (McCredie et al. 1994; McCredie et al. 1990a, b; McMichael and Bonett 1981; McMichael et al. 1980). However, these studies reported on relatively large, heterogenous countries of birth (e.g., Asia being classified as one group) (McCredie et al. 1990b), were state-specific or are now dated (McCredie et al. 1990b, 1994; McMichael and Bonett 1981). A contemporary analysis of the incidence of major cancers by migrant groups is warranted given the changing sociodemographic profile of migrants over time (Parliamentary Library 2018), and changing rates worldwide in these cancers over time (Sung et al. 2021). These findings potentially help understand the etiology of these cancers and guide the implementation of culturally sensitive and safe prevention measures. Therefore, this study aimed to compare the incidence of four major cancers among Australian migrants to the native-born Australians.
Methods
Study population
The number of colorectal, lung, female breast, and prostate cancer cases diagnosed during 2005–2014 by country of birth (COB) and region of birth, sex, 5 year age groups and year of diagnosis were obtained from the Australian Cancer Database (Australian Institute of Health and Welfare 2019), which compiles national data from the eight state and territory population-based cancer registries. By law, all cancers diagnosed in Australia must be reported to the relevant jurisdictional register.
The corresponding population data, estimated resident population (ERP), were obtained from the Australian Bureau of Statistics (Australian Bureau of Statistics 2019). The ERP by COB for each between-census year were estimated by interpolation, using administrative data relating to births, deaths, and overseas migration together with routinely collected information on COB for Australian residents during quinquennial population censuses.
Migrants were defined based on their COB, consistent with the most widely used definition in migrant studies (Arnold et al. 2010). Australian cancer registries routinely collect this information, generally from hospital inpatient records, supplemented with death records if the patient has died. We reported 12 COBs with relatively large populations individually (in the top ten countries for the overseas-born population in either the 2006 or 2011 Census, plus Ireland), and 17 regions with additional countries included in their relevant regions (Table 1), based on the Standard Australian Classification of Countries (SACC) (Australian Bureau of Statistics 2016). Cases for whom the cancer registry had missing COB data were excluded from the analysis.
Statistical analyses
Three regions (Micronesia, Caribbean, and Central and West Africa) were excluded from these analyses as their expected number of new cases was < 50 per cancer type/sex/region combinations (Yu et al. 2022). Data were analyzed by sex because of the anticipated differences in the prevalence of exposures and variations in screening or testing participation.
Age-standardized incidence rates (per 100,000) were calculated for each migrant group by cancer type using the world standard population (Bray et al. 2017). Incidence rate ratios (IRRs) and 95% confidence intervals (CI) were calculated for each migrant group relative to the Australian-born population, using a negative binomial regression model adjusted for age group, year of diagnosis, and the log of the population as an offset variable. All analyses were performed using SAS version 9.4 (SAS Institute Inc) and the figures were produced using R 4.0.5 (R Core Team, 2021).
Results
Over half a million (548,851) Australian residents diagnosed with one of the four selected cancers during 2005–2014 were included in the analysis. Overall, 6.7% of the records had missing COB data, ranging from 2.0% for lung cancer to 10.4% for prostate cancer. The highest proportion of cancer cases that were Australian-born were those with prostate cancer (71%), followed by colorectal and breast cancer (69%), and lung cancer (64%).
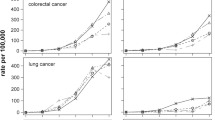
Age-standardized incidence rates and adjusted IRRs are presented in Supplementary Tables 1 and 2, with significant variation observed for each cancer type by migrant groups (p < 0.0001). The adjusted IRRs were plotted in Figs. 1, 2, 3 and 4. Incidence rates were generally lower in most migrant groups for colorectal (for males and females), breast and prostate cancer, except in migrants from English-speaking countries (UK, Ireland, New Zealand, South Africa) for whom rates were relatively higher or closer to the Australian-born rates. For lung cancer, several migrant groups had higher rates than the Australian-born.
Adjusted incidence rate ratio† by region of birth§ relative to the Australian-born residents by cancer type, females. †Adjusted for age group at diagnosis, and year of diagnosis in a negative binomial regression model with Australian-born population as a reference. §Countries/Regions ordered by the Standard Australian Classification of Countries code (see Supplementary Tables for details.)
Colorectal cancer
Most migrant groups had lower rates of colorectal cancer than the Australian-born population, with the lowest rates observed in migrants from India (IRR M 0.51–F 0.55), and Southern Asia (M 0.48–F 0.52). Only males from Ireland (1.11, 95% CI 1.00–1.22) and females from New Zealand (1.12, 95% CI 1.05–1.19) had higher rates than the Australian-born population.
Lung cancer
In males with lung cancer, migrants from five of 17 regions (Melanesia, Southern Europe, South Eastern Europe, Eastern Europe and the Middle East) had significantly higher incidence rates than their Australian-born counterparts, with the highest rates among migrants from Melanesia (IRR = 1.39, 95% CI 1.10–1.76). Migrants from four countries had significantly higher rates (UK, Ireland, Italy, and Greece), with Irish migrants having the highest rate (1.20, 95% CI 1.08–1.33). In contrast, rates were lower among migrants from four countries and nine regions. Migrants from Southern Asia (0.51, 95% CI 0.46–0.56) and Central Asia (0.51, 95% CI 0.33–0.80) had the lowest rates.
In females, two regions and three countries had higher rates of lung cancer than their Australian-born counterparts, with the highest rates among migrants from Ireland (IRR = 1.47, 95% CI 1.30–1.66) and the Melanesian region (1.40, 95% CI 1.10–1.78). Rates were lower for migrants from seven countries and 11 regions, with the lowest rate being for Greek migrants (0.35, 95% CI 0.31–0.40).
Breast cancer
Females from 12 of 17 regions had significantly lower incidence rates than Australian-born females. Lower rates were predominantly observed among females from Central Asia (IRR = 0.55, 95% CI 0.43–0.70), with Vietnamese females having the lowest rates (0.53, 95% CI 0.49–0.57). Irish and Melanesian migrants had higher rates than Australian-born females (1.12, 95% CI 1.04–1.22; 1.14, 95% CI 1.01–1.29, respectively).
Prostate cancer
Except for three migrant groups (New Zealand, Ireland, and the Melanesia region), which had similar incidence rates to Australian-born males, all migrant groups had lower incidence rates than Australian-born males. Two migrant groups with the lowest rates were those from Vietnam (IRR = 0.32, 95% CI 0.29–0.35), China (0.38, 95% CI 0.35–0.41).
Discussion
Between 2005 and 2014, almost all Australian migrant groups had significantly lower incidence rates for cancers of the colorectum, breast and prostate than their Australian-born counterparts. For lung cancer, rates were lower than Australian-born residents for many migrant groups, but males born in Melanesia and various European regions and females born in Melanesia and Northern Europe had higher rates than their Australian-born counterparts. Thus, further research focusing on the differences in behavior, attitudes, risk factors and health-related characteristics between these migrant groups could provide more insights into the etiology of these cancers. Studies examining migrant groups with low cancer rates may particularly provide insights on how to reduce the incidence in the Australian-born population.
Breast, lung and colorectal cancer are associated with modifiable risk factors (e.g., tobacco smoking, reproductive factors, excess body weight and diet) that vary in prevalence globally (Anand et al. 2008). However, socio-cultural factors and screening or testing behaviors may also be associated with the observed variation in incidence rates (Arnold et al. 2010). Overall, exposures in the COB and acculturation—a process whereby migrants adopt their host country’s exposures (e.g., changes to diet, reproductive practices, and environmental exposures)—may be important in driving patterns of incidence in Australian migrant communities. However, we were unable to account for these factors in this study due to limitations with available data.
Consistent with previous Australian studies, lower breast cancer rates were observed for most migrant groups than Australian-born females. Although differences in genetic factors cannot be ruled out, evidence suggests that other known risk factors (e.g., alcohol consumption, menopausal hormone therapy use) contribute to the higher rates for Australian-born population (Gathani et al. 2014). Lower incidence for females from non-English-speaking countries may suggest a lower prevalence of risk factors among them, e.g., lower alcohol consumption among Chinese, Vietnamese, Italian, Greek and Middle Eastern women (Duncan 2010), alongside a higher prevalence of factors associated with lower breast cancer risk, e.g., lower body mass index (BMI) (Menigoz et al. 2016), and higher rates to initiate and maintain breastfeeding among female migrants (Dennis et al. 2019), one of the strongest protective factors. The lower screening participation rate for many non-English speaking migrants than English speakers (Australian Institute of Health and Welfare 2018) may also contribute to their lower incidence. The similar or higher rates for females born in English-speaking countries suggest that risk factors and possible screening participation may be similar across these countries and Australia (Abbasi-Shavazi and McDonald 2000). Interventions targeting under-screened migrant groups, co-designed with these communities to ensure culturally appropriate delivery would help increase participation in BreastScreen. Closing the equity gap in accessing screening could also be achieved by broadening the source used to identify and invite women to join BreastScreen; currently, the electoral roll is used as the source, which does not capture permanent residents covered by Medicare.
As other Australian studies have found (McCredie et al. 1994; McCredie et al. 1990a, b; McMichael and Bonett 1981; McMichael et al. 1980), most migrant groups had a lower incidence of colorectal cancer than the Australian-born. The high rate in Australian-born residents mirrors global patterns (Sung et al. 2021), and may be partially attributed to the high prevalence of established risk factors, including physical inactivity and excess body weight, heavy alcohol consumption, red/processed meat consumption, and low consumption of dietary fiber (Johnson et al. 2013). The lower odds of colorectal cancer screening (up to 40% lower than locally born participants) among people from non-English speaking backgrounds (Australian Institute of Health and Welfare 2018) may also have contributed to their lower incidence. This may be due to delayed acculturation, as there is evidence of increased screening rates with longer duration of residence in Australia (Weber et al. 2009). Additionally, screening programs may not exist in their home country, with limited awareness or acceptance of screening practices and stigma associated with screening.
A higher incidence of lung cancer was observed among several migrant groups. Higher rates for UK/Irish migrants were consistent with previous studies (McCredie et al. 1990b; McMichael and Bonett 1981), while our findings for the other migrant groups contrast to prior study results indicating lower rates for Middle Eastern (McCredie et al. 1994) and Southern European migrants (including Italy and Greece) (McCredie et al. 1990a). These patterns likely reflect differences in smoking patterns among these migrant groups. Prior Australian studies found that males born in parts of Europe, and the Middle East (Department of Health NSW 2012; Siahpush and Borland 2001; Weber et al. 2011), and females born in New Zealand and UK/Ireland were more likely to smoke (Siahpush and Borland 2001; Weber et al. 2011) than their Australian-born counterparts. As the stages of the tobacco epidemic (i.e., the comparative levels of smoking prevalence and smoking-attributed mortality) have varied globally over time, and given the 20–30 year lag between tobacco exposure and lung cancer incidence (Drope and Schluger 2018), it is of interest to continue monitoring lung cancer rates across migrant groups. The lung cancer treatment and detection landscape is evolving rapidly in Australia, with a potential lung cancer screening program for individuals with a history of heavy smoking on the horizon (Australian Institute of Health and Welfare 2021). Key to its success will be engaging those with the highest risk, including the migrant groups identified here. Further, lung cancer among individuals without a smoking history will also be important to monitor, especially among Asian-born females who have disproportionately higher rates (Cheng et al. 2022).
Prostate cancer rates were lower among most migrant groups than Australian-born males, particularly for males from Asian countries, with rates 50–60% lower in migrants from Southern and North–East Asia. Evidence of well-established risk factors is limited. While age, family history, and specific genetic mutations are shown to increase risk, associations between modifiable factors e.g., diet, BMI and smoking are less clear (World Cancer Research Fund & American Institute for Cancer Research 2018). Internationally, African American men and Caribbean men of African ancestry have some of the highest risk of prostate cancer. The proportion of migrants from these ethnic groups is relatively small in Australia, thus our data do not allow for meaningful comparison. Much of the global variation in incidence (Sung et al. 2021) appears to be related to the prevalence of prostate cancer testing (Zhou et al. 2016). The patterns observed among Australian migrants may be associated with the prevalence of prostate-specific antigen (PSA) testing, however, studies from New South Wales have shown somewhat inconsistent evidence. Some earlier studies suggested that urban-dwelling East Asian males and Chinese-born males had lower PSA testing rates (30 and 50% less, respectively) than Australian-born males based on self-reported data (Litchfield et al. 2012; Weber et al. 2009, 2014), while a more recent analysis based on Medicare claims showed few differences in PSA testing across major migrant groups (Nair-Shalliker et al. 2018). This variation may suggest increased adoption of testing behaviors in migrant groups or issues surrounding health literacy and accuracy of self-reporting of testing behaviors by migrants from non-English speaking backgrounds. Current Australian guidelines regarding testing and treatment for prostate cancer recommend informed decision-making regarding PSA testing for asymptomatic men aged 50–69 (Prostate Cancer Foundation of Australia 2016). Migrants for whom English is not a first language may be less likely to make well-informed decisions about prostate cancer testing, and future development of culturally appropriate resources may be a priority.
The use of recent national cancer incidence data is a strength of this study, providing contemporary insights into the cancer profile of migrants to Australia. Of note, incidence data are superior to mortality data in etiology studies as mortality is influenced by treatment-related factors, which may also vary between population subgroups (McMichael and Bonett 1981). Additionally, the cohort size was sufficiently large to report cancer profiles for many smaller migrant groups, including those from Melanesia, which had higher lung and female breast cancer rates. These cancer rates may provide estimates for their countries of origin due to minimal local cancer registry data. This suggests that future studies should disaggregate migrant groups to reflect the diversity because of their heterogeneous incidence patterns. Also, we used the annual ERP data by COB to provide more accurate rate estimates than the quinquennial census population data used in many previous Australian studies (McCredie et al. 1990a, b; McMichael et al. 1980).
The exclusion of 10.4% of the records with unknown COB for prostate cancer was a limitation and may have affected these results. Many men with low-risk prostate cancer may choose active surveillance without needing hospital care (McIntosh et al. 2022) which is the primary source of the COB data recorded in the cancer registries. Another limitation is that data on the age of migration or length of residence in Australia were not available for analysis, thus we were unable to investigate the impact of acculturation on cancer rates.
The incidence patterns observed suggest that the lower rates for most migrant groups may be maintained with continued emphasis on healthy lifestyle behaviors and uptake of organized screening in culturally safe and sensitive ways. For lung cancer, this is particularly important for tobacco control measures which could be best targeted to those migrant communities identified in this study with higher incidence rates.
Data availability
This study involves the analysis of aggregated data from the Australian Cancer Database, managed by the Australian Institute of Health and Welfare (AIHW). Data may be available from the corresponding author with approval from the data custodian in each state and territory of Australia.
References
Abbasi-Shavazi MJ, Mcdonald P (2000) Fertility and multiculturalism: immigrant fertility In Australia, 1977–1991. Int Migr Rev 34:215–242
Anand P, Kunnumakkara AB, Sundaram C, Harikumar KB, Tharakan ST, Lai OS, Sung B, Aggarwal BB (2008) Cancer is a preventable disease that requires major lifestyle changes. Pharm Res 25:2097–2116
Arnold M, Razum O, Coebergh JW (2010) Cancer risk diversity in non-western migrants to Europe: an overview of the literature. Eur J Cancer 46:2647–2659
Australian Bureau Of Statistics. 2016. Standard Australian Classification Of Countries (SACC) [Online]. Canberra: ABS. Available: http://www.abs.gov.au/ausstats/abs@.nsf/latestproducts/1269.0main%20features12016?opendocument&tabname=summary&prodno=1269.0&Issue=2016&num=&View=. Accessed 30 June 2018
Australian Bureau Of Statistics (2019) Estimated Resident Population, Country of Birth, Age and Sex - As At 30 June 1996 To 2019. In: ABS (Ed.). Canberra
Australian Bureau Of Statistics. 2021. Migration, Australia [Online]. Canberra: Abs. Available: https://www.abs.gov.au/statistics/people/population/migration-australia/latest-release#:~:text=in%202020%2c%20there%20were%20over,in%20australia’s%20population%20in%202020. Accessed 20 May 2021
Australian Institute Of Health And Welfare (2018) Analysis Of cancer outcomes and screening behaviour for national cancer screening programs in Australia. AIHW, Canberra
Australian Institute Of Health And Welfare (2019) Australian Cancer Database (ACD). AIHW, Canberra
Australian Institute Of Health And Welfare (2021) Cancer in Australia 2021. Cat. No. Can, 144th edn. AIHW, Canberra
Bray F, Colombet M, Mery L, Pineros M, Znaor A, Zanetti R, Ferlay J (2017) Cancer Incidence In Five Continents, Lyon, International Agency For Research On Cancer
Cheng ES, Weber MF, Steinberg J, Canfell K, Yu XQ (2022) Evaluating risk factors for lung cancer among never-smoking individuals using two Australian studies. J Cancer Res Clin Oncol 148:2827–2840
Dennis CL, Shiri R, Brown HK, Santos HP Jr, Schmied V, Falah-Hassani K (2019) breastfeeding rates in immigrant and non-immigrant women: a systematic review and meta-analysis. Matern Child Nutr 15:E12809
Department Of Health NSW (2012) report on adult health by country of birth from the New South Wales adult population health survey 2006–2009. NSW Health, Sydney
Drope J, Schluger NW (2018) The Tobacco Atlas. American Cancer Society and Vital Strategies
Duncan B (2010) Engaging Culturally Diverse Communities. Of Subst Nati Mag Alcohol Tobacco Other Drugs 8:26–28
Gathani T, Ali R, Balkwill A, Green J, Reeves G, Beral V, Moser KA, Million Women Study, C (2014) Ethnic differences in breast cancer incidence in England are due to differences in known risk factors for the disease: prospective study. Br J Cancer 110:224–229
Johnson CM, Wei C, Ensor JE, Smolenski DJ, Amos CI, Levin B, Berry DA (2013) Meta-analyses of colorectal cancer risk factors. Cancer Causes Control 24:1207–1222
Litchfield MJ, Cumming RG, Smith DP, Naganathan V, Le Couteur DG, Waite LM, Blyth FM, Handelsman DJ (2012) Prostate-specific antigen levels in men aged 70 years and over: findings from the champ study. Med J Aust 196:395–398
McCredie M, Coates MS, Ford JM (1990a) Cancer incidence in European migrants to New South Wales. Ann Oncol 1:219–225
McCredie M, Coates MS, Ford JM (1990b) Cancer incidence in migrants to New South Wales. Int J Cancer 46:228–232
McCredie M, Coates M, Grulich A (1994) Cancer incidence in migrants to New South Wales (Australia) from the middle east, 1972–91. Cancer Causes Control 5:414–421
McIntosh M, Opozda MJ, O’Callaghan M, Vincent AD, Galvao DA, Short CE (2022) Why do men with prostate cancer discontinue active surveillance for definitive treatment? A mixed methods investigation. Psychooncology 31:1420–1430
McMichael AJ, Bonett A (1981) Cancer profiles of british and Southern-European migrants. exploring South Australia’s cancer registry data. Med J Aust 1:229–232
McMichael AJ, McCall MG, Hartshorne JM, Woodings TL (1980) Patterns of gastro-intestinal cancer in European Migrants to australia: the role of dietary change. Int J Cancer 25:431–437
Menigoz K, Nathan A, Turrell G (2016) Ethnic differences in overweight and obesity and the influence of acculturation on immigrant bodyweight: evidence from a National sample of Australian adults. BMC Public Health 16:932
Nair-Shalliker V, Bang A, Weber M, Goldsbury DE, Caruana M, Emery J, Banks E, Canfell K, O’connell DL, Smith DP (2018) Factors associated with prostate specific antigen testing in Australians: analysis of the New South Wales 45 and up study. Sci Rep 8:4261
Parliamentary Library (2018) Top 10 countries of birth for the overseas-born population since 1901. In: Department of parliamentary services (Ed.). Canberra
Prostate Cancer Foundation of Australia and Cancer Australia. (2016) Clinical practice guidelines on PSA testing. Prostate Cancer Foundation of Australia, Melbourne
Siahpush M, Borland R (2001) Socio-demographic variations in smoking status among Australians aged > Or = 18: multivariate results from the 1995 national health survey. Aust N Z J Public Health 25:438–442
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F (2021) Global cancer statistics 2020: globocan estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 71:209–249
Weber MF, Banks E, Smith DP, O’connell D, Sitas F (2009) Cancer screening among migrants in an Australian cohort; cross-sectional analyses from the 45 and up study. BMC Public Health 9:144
Weber MF, Banks E, Sitas F (2011) Smoking In migrants in New South Wales, Australia: report on data from over 100 000 participants in the 45 and up study. Drug Alcohol Rev 30:597–605
Weber MF, Chiew M, Feletto E, Kahn C, Sitas F, Webster L (2014) Cancer screening among immigrants living In Urban And Regional Australia: results from the 45 and up study. Int J Environ Res Public Health 11:8251–8266
World Cancer Research Fund & American Institute for Cancer Research. Diet, nutrition, physical activity and cancer: a global perspective. Continuous Update Project Expert Report 2018. World Cancer Research Fund
Yu XQ, Feletto E, Smith MA, Yuill S, Baade PD (2022) Cancer incidence in migrants in australia: patterns of three infection-related cancers. Cancer Epidemiol Biomarkers Prev 31:1394–1401
Zhou CK, Check DP, Lortet-Tieulent J, Laversanne M, Jemal A, Ferlay J, Bray F, Cook MB, Devesa SS (2016) Prostate cancer incidence in 43 populations worldwide: an analysis of time trends overall and by age group. Int J Cancer 138:1388–1400
Acknowledgements
We thank the Australian Institute of Health and Welfare for providing the data for this study and the data custodian in each state and territory of Australia for their approval to release the data, and Ankur Kohar for assistance in producing high-quality figures.
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions. No financial disclosures were reported by the authors of this paper.
Author information
Authors and Affiliations
Contributions
Conceptualization: XQY; formal analysis: XQY; methodology: XQY; software: XQY; visualization: XQY; writing—original draft: XQY; XQY had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis; writing—review and editing: XQY, MW, DS, LV, EVK, MD, and EF. All authors have approved the final version of the manuscript for publication.
Corresponding author
Ethics declarations
Conflict of interest
No conflict of interests is declared.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Yu, X.Q., Weber, M., Smith, D. et al. Incidence profile of four major cancers among migrants in Australia, 2005–2014. J Cancer Res Clin Oncol 149, 8317–8325 (2023). https://doi.org/10.1007/s00432-023-04764-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00432-023-04764-5