Abstract
Purpose
Systemic immune-inflammation index (SII) has been demonstrated to be closely associated with the poor prognosis of nasopharyngeal carcinoma (NPC). However, the role of SII during treatment of NPC has not been reported. This study aimed to determine the prognostic value of SII during treatment for NPC patients.
Methods
A total of 759 patients diagnosed with NPC were included in this retrospective study (393 in training cohort and 366 in validation cohort). The correlation between variables was analyzed by the chi-squared test, the Fisher’s exact test or the likelihood test. Kaplan–Meier method and log-rank test were used to analyze progression-free survival (PFS) and overall survival (OS). The independent prognostic factors were determined by multivariate analysis of Cox proportional hazards regression model. The uncontrolled risk was analyzed by Logistic regression. Receiver operating characteristic (ROC) curves were used to assess prognostic value.
Results
The optimal cut-off point for the SII during treatment was 937.32. High SII during treatment group had higher uncontrolled risk than low SII during treatment group (p = 0.008). In multivariate Cox proportional hazard models analysis, SII during treatment was an independent prognostic factor for 5-year PFS (p < 0.001) and 5-year OS (p < 0.001). All results were found in the training cohort and confirmed in the validation cohort.
Conclusions
The SII during treatment is a promising indicator of predicting the survival in NPC patients, especially the risk of uncontrolled occurrence. By monitoring the SII during treatment, it is possible to better evaluate the treatment effect and formulate personalized treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Nasopharyngeal carcinoma (NPC) is a malignant tumor of the head and neck originating from the nasopharyngeal epithelium, it is closely related to Epstein–Barr virus (EBV) infection, and has apparent regional and epidemic characteristics (Chen et al. 2019; Sung et al. 2021). Since it is sensitive to chemo-radiation, radiotherapy with or without chemotherapy is the main treatment for NPC patients. However, the survival of one-third of patients remains poor because of local recurrence and distant metastasis (Wu et al. 2014; Lee et al. 2015). In addition, some patients have residual disease or develop recurrent disease at the primary or regional site (Mao et al. 2016). Therefore, finding an effective and accurate prognostic indicator is crucial to improve the clinical management of NPC.
In recent years, increasing evidence has shown that activation of inflammation is a crucial mechanism for the recurrence and metastasis of cancer (Balkwill and Mantovani 2010). Inflammatory parameters such as the neutrophil to lymphocyte ratio (NLR) (Chua et al. 2016), platelet-to-lymphocyte ratio (PLR) (Fang et al. 2020), systemic immune-inflammation index (SII) (Hu et al. 2014) and systemic inflammation response index (SIRI) (Valero et al. 2019) have been identified as prognostic biomarkers in multiple cancers, including gastric cancer, hepatocellular cancer, oral cavity cancer and NPC. A previous study was followed by Zeng et al. (2020), which conducted a retrospective study including 559 NPC patients and 500 chronic rhinitis patients. This study reported that pre-treatment inflammatory parameters (including NLR, PLR, SII and SIRI) in patients with NPC were significantly higher than those in patients with chronic rhinitis, and could be used as prognostic indicators in NPC patients. However, since most of the relevant studies mainly focused on prognosis with pre-treatment inflammatory parameters, to our knowledge, no data on the investigation of the prognostic potential of the inflammatory parameters during treatment for NPC are present. In addition, some patients have residual tumor or metastasis within 6 months after the end of the treatment, these patients were called uncontrolled in clinical practice. Radio-resistance is an important cause of uncontrolled occurrence in NPC, and studies reported that radio-resistant tumor cells could cause an increase in inflammation during treatment (Nantajit et al. 2015; Yuan et al. 2021). Therefore, observing changes in inflammatory parameters during treatment was of great significance in predicting the degree of uncontrolled risk.
Therefore, a total 759 NPC patients were included in this retrospective study. The objective of this study was to evaluate the prognostic of inflammatory parameters during treatment. In addition, whether the inflammatory parameters during treatment provides a credible prognostic evaluation for uncontrolled patients was also assessed. This study aimed to determine the prognostic value of inflammatory parameters for NPC patients during treatment, and determine whether inflammatory parameters can enhance the survival prediction, and promote development of individualized treatment approach for NPC.
Materials and methods
Case selection
We retrospectively recruited 759 patients who were diagnosed with NPC at NanFang Hospital of Southern Medical University from December 2007 to December 2015. All patients were treated according to the guidelines (The treatment method was detailed in Supplementary file 1). All patients were divided into the training cohort and validation cohort by random number. The eighth edition of the American Joint Committee on Cancer (AJCC) staging system was used for stage classification. This study was approved by the Ethics Committee of Nanfang Hospital of Southern Medical University (Ethical review approval no.: NFEC-2017-165).
Inclusion and exclusion criteria
The inclusion criteria in this study comprised of: (a) patients with histopathological confirmation of NPC; (b) patients with complete medical records and treatment time records; and (c) patients with at least one complete record of haematological indicators during treatment. The exclusion criteria were as follows: (a) patients with non-WHO pathological types; (b) patients with prior malignancy; and (c) non-first-treatment; (d) patients with uncontrolled infection.
Haematological examination
The peripheral blood of all patients was collected and tested for neutrophil, lymphocyte, platelet and monocyte counts within 2 days before the start of each chemotherapy and 3 days after the end of each chemotherapy, or at least once a week during the entire treatment period. The measurements of plasma EBV DNA were performed within 1 month before therapy. If the patient had II bone marrow suppression, peripheral blood cells were monitored twice a week, while if the patient had III or worse bone marrow suppression, short-acting recombinant human granulocyte colony stimulating factor therapy was given. The peripheral blood data with the lowest leukocyte count was selected during treatment. All peripheral blood cell and EBV DNA assessments were performed in our hospital’s institutional laboratory according to standard operating procedures (The detection method for EBV DNA in Supplementary file 2). The cut-off level chosen to classify the patients into the negative and positive EBV DNA groups was 500 copies/mL before treatment, referring to the threshold of Laboratory Medicine Center, Nanfang Hospital, Southern Medical University. The NLR was defined as neutrophil/lymphocyte; the PLR was defined as platelet/lymphocyte; the SII was defined as (neutrophil*platelet)/lymphocyte; the SIRI was defined as (neutrophil*monocyte)/lymphocyte.
Follow-up
Patients were followed up at 3, 6, and 12 months in the first year after treatment, every 6 months in the second and third years, and once a year thereafter. Follow-up assessments included head and neck physical examination, nasopharyngeal endoscopy, chest radiograph, abdominal ultrasound, peripheral blood examination, nasopharyngeal and neck magnetic resonance imaging (MRI) and emission computed tomography (ECT) or the whole-body positron emission tomography-computed tomography (PET-CT). For cases of suspected nasopharyngeal and neck tumor recurrence or distant metastasis to cervical lymph nodes, biopsy or acupuncture biopsy of the suspected site was performed to confirm the diagnosis. Progression-free survival (PFS) was defined as the time from the initial pathological diagnosis of NPC to the date of disease progression or death from any cause. Overall survival (OS) was defined as the time between the initial pathological diagnosis of NPC and all-cause death, or at the last follow-up. Uncontrolled was defined as the tumor remained or metastases appeared within 6 months after the end of treatment.
Statistical analysis
The Statistical Packages for Social Science version 23.0 (IBM, Corporation) was used. The optimal cut-off value of NLR, PLR, SII and SIRI were determined using X-tile 3.6.1 software (Robert L Camp, Yale University, New Haven, CT, USA) (Camp et al. 2004; Lolli et al. 2016). The cut-off value was plotted by X-tile 3.6.1 software, and other figures were plotted by GraphPad Prism V8.0. The chi-squared test, Fisher’s exact test or likelihood test was used to explore the baseline balance between the inflammatory parameters groups. Survival curves were analyzed using the Kaplan–Meier method and compared using the log-rank test. Univariate and multivariate Cox proportional hazards regressions were conducted to evaluate the prognostic significance of each variable with respect to PFS and OS. Logistic regression was used to estimate odds ratio (OR) and 95% CI in order to evaluate the association between clinical characteristics and uncontrolled rate. Receiver operating characteristic (ROC) curve analysis was performed to compare the different prognostic values. All results were validated by the validation cohort. A two-tailed p value of less than 0.05 was considered as statistically significant.
Results
The optimal cut-off values of inflammatory parameters
The X-tile 3.6.1 software was used to evaluate the optimal cutoff value of the NLR, PLR, SII and SIRI for progression outcome in training cohort. The cut-off values of the NLR, PLR, SII and SIRI were 4.38 (p = 0.053), 311.86 (p = 0.035), 937.32 (p = 0.003) and 1.27 (p = 0.051), respectively (Fig. 1). Since only the cut-off values of PLR and SII were statistically significant after being calculated by X-tile software, PLR and SII were included in the subsequent statistical analysis.
X-tile analysis of survival data of NPC patients. a The optimal cut-off value for the NLR was 4.38 (chi square = 9.184, p = 0.053); b The optimal cut-off value for the PLR was 311.86 (chi square = 10.112, p = 0.035); c The optimal cut-off value for the SII was 937.32 (chi square = 15.732, p = 0.003); d The optimal cut-off value for the SIRI was 1.27 (chi square = 9.291, p = 0.051)
Baseline patient characteristics
A total of 393 and 366 patients were included in the training cohort and validation cohort, respectively. The baseline characteristics of the patients are shown in Tables 1 and 2. In the training cohort, there were 288 males (73.3%) and 105 females (26.7%). The median follow-up time was 61 months. During the long-term follow-up, 123 patients (31.3%) experienced disease progression, and 63 patients (16.0%) died. In the validation cohort, there were 258 males (70.5%) and 108 females (29.5%). The median follow-up time was 59 months. During the long-term follow-up, 110 patients (30.1%) experienced disease progression, and 60 patients (16.4%) died. Table 1 shows the correlations between SII during treatment and patient clinical characteristics in the two cohorts. In training cohort, SII during treatment was significantly correlated with age, tumor stage and metastasis (p < 0.05). However, there was no significant correlation in validation cohort. Table 2 shows the correlations between PLR during treatment and patient clinical characteristics in the two cohorts. In training cohort, PLR during treatment was significantly correlated with EBV DNA status, tumor stage and metastasis (p < 0.05). In validation cohort, there was no correlation between PLR during treatment and EBV DNA status, tumor stage and metastasis. In addition, the baseline characteristics for the training cohort and validation cohort are shown in Supplementary Table 1. The results showed that there was no significant difference in baseline characteristics between the two cohorts.
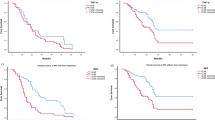
Kaplan–Meier method and log-rank test
Kaplan–Meier survival curves based on SII during treatment and PLR during treatment for survival analysis of training and validation cohorts are shown in Figs. 2 and 3. In the training cohort, the higher SII group demonstrated poorer PFS (p < 0.001) and OS (p < 0.001) compared to the lower SII group. And the higher PLR group demonstrated poorer PFS (p = 0.002) and OS (p = 0.033) compared to the lower PLR group. The survival results of SII during treatment were confirmed in the validation cohort (all p < 0.001). However, in the validation cohort, the higher PLR group were not significant associated to poorer PFS (p = 0.071) and OS (p = 0.314). Therefore, only SII during treatment was included in subsequent univariate and multivariate analyses.
Univariate and multivariate Cox regression analysis
In the univariate Cox regression model, age (p = 0.016), AJCC stage (p < 0.001), node stage (p = 0.003), metastasis (p = 0.024), EBV DNA (p = 0.001) and SII during treatment (p < 0.001) were significantly associated with PFS in training cohort. Age (p = 0.007), AJCC stage (p = 0.030), tumor stage (p = 0.025), metastasis (p = 0.017), EBV DNA (p = 0.007) and SII during treatment (p < 0.001) were significantly associated with PFS in validation cohort. Age (p < 0.001), AJCC stage (p < 0.001), node stage (p = 0.032), metastasis (p = 0.010) and SII during treatment (p < 0.001) were significantly associated with OS in training cohort. Age (p < 0.001), AJCC stage (p = 0.026), tumor stage (p = 0.016), metastasis (p < 0.001), EBV DNA (p = 0.003) and SII during treatment (p = 0.001) were significantly associated with OS in validation cohort (Table 3). All variables reaching statistical significance in univariate analysis were included in multivariate Cox regression analysis.
In the multivariate Cox regression model, the EBV DNA and SII during treatment were still independent risk factors in NPC patients for PFS in the training cohort and validation cohort (all p < 0.05). The age and SII during treatment were still found to be independent risk factors in NPC patients for OS in the training cohort and validation cohort (all p < 0.05) (Table 4).
Relationship between uncontrolled rate and clinical characteristics
We further assessed which clinical characteristics were risk factors for uncontrolled occurrence. In the univariate logistic regression analysis, the AJCC stage (p = 0.046), metastasis (p = 0.040), EBV DNA (p = 0.035) and SII during treatment (p = 0.008) were risk factors for uncontrolled in training cohort. The age (p = 0.002) and SII during treatment (p = 0.003) were risk factors for uncontrolled in validation cohort (Table 5).
In the multivariate logistic regression analysis, only the SII during treatment was the risk factor for the uncontrolled in the training cohort and validation cohort (all p < 0.05) (Table 6). The graph for uncontrolled rate of SII during treatment subgroups is shown in Fig. 4.
ROC curves analysis
By comparing the ROC curves, the SII during treatment demonstrated slightly smaller area under the curve (AUC) values than EBV DNA for predicting NPC progression in training cohort. However, the SII during treatment demonstrated larger area under the curve (AUC) values than EBV DNA for predicting NPC progression in validation cohort. For predicting NPC mortality, the SII during treatment demonstrated larger area under the curve (AUC) values than age in training cohort, however, the SII during treatment demonstrated slightly smaller area under the curve (AUC) values than age in validation cohort (Fig. 5).
Discussion
In recent years, important progress in comprehensive therapies including chemotherapy, radiotherapy, targeted therapy, and immunotherapy has significantly improved survival time and quality of life for NPC patients (Lee et al. 2015; Chen et al. 2019). There are still around 10% of patients who have residual disease or develop recurrent disease which we called uncontrolled in this study, and these patients have extremely poor overall survival (Liu et al. 2019). Therefore, finding a prognosticator that can predict uncontrolled occurrence has great clinical value for NPC patients.
Inflammation is one of the seven characteristics of cancer, causing approximately 25% of new cancer cases worldwide (Schetter et al. 2010). There are increasing data showing that inflammation is closely related with tumorigenesis, proliferation, angiogenesis, metastasis, and other processes (Mantovani et al. 2008; Hanahan and Weinberg 2011). The mechanism by which high inflammatory parameters lead to poor prognosis in cancer patients remains controversial. The prognostic value of the inflammatory parameters can be explained by the role of its components. Circulating neutrophils secreted large arginase, nitric oxide, and ROS which can cause T cell activation disorder (Kusumanto et al. 2003; Müller et al. 2009; Moses and Brandau 2016). Lymphocytes play critical roles in the host immune response through inhibiting the proliferation and metastasis of cancer cells (Marra et al. 2014). Platelets in tumor patients can protect circulating tumor cells (CTCs) from shear stresses in the circulation, induce CTCs epithelial-mesenchymal transition (EMT), and promote the penetration of CTCs to metastatic sites (Labelle et al. 2011; Gil-Bernabe et al. 2012; Placke et al. 2012). NPC is typically characterized by the infiltration of inflammatory cells, which has an important role in inflammation. Accordingly, the cooperation between these inflammatory cells in the microenvironment of tumor inflammation may contribute to the tumorigenesis and cancer progression.
In this study, we found that high SII during treatment were closely related to worse 5-year PFS and OS in NPC patients, and this result was verified by the validation cohort. As a new and widely used prognostic indicator, previous studies have confirmed that pre-treatment SII have independent prognostic value in several solid tumors including NPC (Hu et al. 2014; Jiang et al. 2017; De Giorgi et al. 2019; Ji and Wang 2020). But to the best of our knowledge, the performance of the SII during treatment for predicting prognosis in NPC patients has not been investigated. In addition, we considered that the changes of inflammation/immune status during treatment should not be ignored, because it can help judge the sensitivity of the patient’s treatment. These findings confirmed that the SII during treatment could also have independent prognostic value like the pre-treatment SII in patients with NPC. And this is consistent with the poor prognosis of patients with high inflammation, high coagulation, and low lymphocytes as currently considered by scholars (Kusumanto et al. 2003; Marra et al. 2014; Moses and Brandau 2016). Regretfully, whether the prognostic value of SII during treatment was greater than that of EBV DNA and age was not confirmed in the validation cohort. This result needs to be further explored in future studies.
Another important finding from our study was that the high SII during treatment group had higher uncontrolled rate than the low SII during treatment group. Although statistical analysis of EBV DNA in the training cohort also yielded the same result, after verification in the validation cohort, only the SII during treatment still remained the statistical difference. Uncontrolled was an easily overlooked link in clinical practice and is of great significance to the integral prognosis of patients. Nonlocal failure, which the definition is similar to uncontrolled had been confirmed to be related to immune-inflammatory response in non-small-cell lung cancer (Cannon et al. 2015). It was reported that the nonlocal failure rate of patients in the high PLR (platelet-to-lymphocyte ratio) group was significantly higher than that of the patients in the low PLR group. In previous studies, the use of anti-inflammatory drugs can benefit cancer patients with high SII status (Kim et al. 2013; van Staalduinen et al. 2016). Our study found that the higher the SII during treatment, the higher the uncontrolled rate. Combining the above content, we considered that the SII during the treatment could give us predictions about the prognosis and treatment failure, and help us better evaluate the treatment effect. At present, the TNM staging of nasopharyngeal carcinoma can only reflect the size and progression of the tumor from an anatomical point of view, and cannot identify high-risk patients more effectively (Lee et al. 2012; Pan et al. 2016). Peripheral blood cells must always be monitored during treatment to evaluate the side effects of the patient's treatment. According to our study, we found changes in SII during treatment are closely related to prognosis and uncontrolled rate of NPC patients. Considering the above results, we hope that by monitoring the SII during the treatment combined with the risk stratification of patients in the same stage will help in the decision for high-risk patients to further improve the radiotherapy and chemotherapy regimens, or increase targeted therapy or even further immunotherapy. This study can assist TNM staging without increasing the burden on patients and treatment risks, and assist clinicians in obtaining better clinical decision-making, and formulate personalized treatment for patients by using the results of peripheral blood cells monitoring during treatment.
Our study had made some improvements compared with previous studies. To the best of our knowledge, we were the first to study the prognostic value of SII in NPC patients during treatment. In addition, we explored the possible risk factors for uncontrolled occurrence of NPC patients. However, our study has some limitations, this study is a retrospective study, and there may be potential deviations. Therefore, the follow-up still needs to conduct more large-scale prospective, multicenter, randomized clinical trials for further verification and research.
Conclusion
In summary, our study demonstrated that SII during treatment was an independent prognostic predictor for PFS and OS in NPC patients, and could provide a prognostic and risk value for uncontrolled occurrence of NPC patients. Therefore, through monitoring SII during treatment, we can better evaluate the treatment effect and formulate personalized treatment.
Data availability
The data used to support the findings of this study are available from the corresponding author upon request.
References
Balkwill F, Mantovani A (2010) Cancer and inflammation: implications for pharmacology and therapeutics. Clin Pharmacol Ther 87(4):401–406
Camp RL, Dolled-Filhart M, Rimm DL (2004) X-tile: a new bio-informatics tool for biomarker assessment and outcome-based cut-point optimization. Clin Cancer Res 10(21):7252–7259
Cannon NA, Meyer J, Iyengar P et al (2015) Neutrophil-lymphocyte and platelet-lymphocyte ratios as prognostic factors after stereotactic radiation therapy for early-stage non–small-cell lung cancer. J Thorac Oncol 10(2):280–285
Chen YP, Chan A, Le QT et al (2019) Nasopharyngeal carcinoma. Lancet 394(10192):64–80
Chua MLK, Tan SH, Kusumawidjaja G et al (2016) Neutrophil-to-lymphocyte ratio as a prognostic marker in locally advanced nasopharyngeal carcinoma: a pooled analysis of two randomised controlled trials. Eur J Cancer 67:119–129
De Giorgi U, Procopio G, Giannarelli D et al (2019) Association of systemic inflammation index and body mass index with survival in patients with renal cell cancer treated with nivolumab. Clin Cancer Res 25(13):3839–3846
Fang T, Wang Y, Yin X et al (2020) Diagnostic sensitivity of NLR and PLR in early diagnosis of gastric cancer. J Immunol Res 2020:1–9
Gil-Bernabe AM, Ferjancic S, Tlalka M et al (2012) Recruitment of monocytes/macrophages by tissue factor-mediated coagulation is essential for metastatic cell survival and premetastatic niche establishment in mice. Blood 119(13):3164–3175
Hanahan D, Weinberg RA (2011) Hallmarks of cancer: the next generation. Cell 144(5):646–674
Hu B, Yang X, Xu Y et al (2014) Systemic immune-inflammation index predicts prognosis of patients after curative resection for hepatocellular carcinoma. Clin Cancer Res 20(23):6212–6222
Ji Y, Wang H (2020) Prognostic prediction of systemic immune-inflammation index for patients with gynecological and breast cancers: a meta-analysis. World J Surg Oncol. https://doi.org/10.1186/s12957-020-01974-w
Jiang W, Chen Y, Huang J et al (2017) Systemic immune-inflammation index predicts the clinical outcome in patients with nasopharyngeal carcinoma: a propensity score-matched analysis. Oncotarget 8(39):66075–66086
Kim AK, Dziura J, Strazzabosco M (2013) Nonsteroidal anti-inflammatory drug use, chronic liver disease, and hepatocellular carcinoma: the egg of Columbus or another illusion? Hepatology 58(2):819–821
Kusumanto YH, Dam WA, Hospers GA, Meijer C, Mulder NH (2003) Platelets and granulocytes, in particular the neutrophils, form important compartments for circulating vascular endothelial growth factor. Angiogenesis 6(4):283–287
Labelle M, Begum S, Hynes RO (2011) Direct signaling between platelets and cancer cells induces an epithelial-mesenchymal-like transition and promotes metastasis. Cancer Cell 20(5):576–590
Lee AWM, Ng WT, Chan LK et al (2012) The strength/weakness of the AJCC/UICC staging system (7th edition) for nasopharyngeal cancer and suggestions for future improvement. Oral Oncol. 48(10):1007–1013
Lee AWM, Ma BBY, Ng WT, Chan ATC (2015) Management of nasopharyngeal carcinoma: current practice and future perspective. J Clin Oncol 33(29):3356–3364
Liu YP, Li H, You R et al (2019) Surgery for isolated regional failure in nasopharyngeal carcinoma after radiation: Selective or comprehensive neck dissection. Laryngoscope 129(2):387–395
Lolli C, Caffo O, Scarpi E et al (2016) Systemic immune-inflammation index predicts the clinical outcome in patients with mCRPC treated with abiraterone. Front Pharmacol. https://doi.org/10.3389/fphar.2016.00376
Mantovani A, Allavena P, Sica A, Balkwill F (2008) Cancer-related inflammation. Nature 454(7203):436–444
Mao Y, Tang L, Chen L et al (2016) Prognostic factors and failure patterns in non-metastatic nasopharyngeal carcinoma after intensity-modulated radiotherapy. Chin J Cancer. https://doi.org/10.1186/s40880-016-0167-2
Marra P, Mathew S, Grigoriadis A et al (2014) IL15RA Drives antagonistic mechanisms of cancer development and immune control in lymphocyte-enriched triple-negative breast cancers. Cancer Res 74(17):4908–4921
Moses K, Brandau S (2016) Human neutrophils: their role in cancer and relation to myeloid-derived suppressor cells. Semin Immunol 28(2):187–196
Müller I, Munder M, Kropf P, Hänsch GM (2009) Polymorphonuclear neutrophils and T lymphocytes: strange bedfellows or brothers in arms? Trends Immunol 30(11):522–530
Nantajit D, Lin D, Li JJ (2015) The network of epithelial–mesenchymal transition: potential new targets for tumor resistance. J Cancer Res Clin 141(10):1697–1713
Pan JJ, Ng WT, Zong JF et al (2016) Proposal for the 8th edition of the AJCC/UICC staging system for nasopharyngeal cancer in the era of intensity-modulated radiotherapy. Cancer-Am Cancer Soc 122(4):546–558
Placke T, Salih HR, Kopp H (2012) GITR ligand provided by thrombopoietic cells inhibits NK cell antitumor activity. J Immunol 189(1):154–160
Schetter AJ, Heegaard NHH, Harris CC (2010) Inflammation and cancer: interweaving microRNA, free radical, cytokine and p53 pathways. Carcinogenesis 31(1):37–49
Sung H, Ferlay J, Siegel RL et al (2021) Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA: Cancer J Clin 71(3):209–249
Valero C, Zanoni DK, McGill MR et al (2019) Pretreatment peripheral blood leukocytes are independent predictors of survival in oral cavity cancer. Cancer-Am Cancer Soc 126(5):994–1003
van Staalduinen J, Frouws M, Reimers M et al (2016) The effect of aspirin and nonsteroidal anti-inflammatory drug use after diagnosis on survival of oesophageal cancer patients. Brit J Cancer 114(9):1053–1059
Wu F, Wang R, Lu H et al (2014) Concurrent chemoradiotherapy in locoregionally advanced nasopharyngeal carcinoma: treatment outcomes of a prospective, multicentric clinical study. Radiother Oncol 112(1):106–111
Yuan X, Zhang L, Huang Y et al (2021) Induction of interleukin-6 by irradiation and its role in epithelial mesenchymal transition and radioresistance of nasopharyngeal carcinoma cells. Head Neck 43(3):757–767
Zeng X, Liu G, Pan Y, Li Y (2020) Development and validation of immune inflammation–based index for predicting the clinical outcome in patients with nasopharyngeal carcinoma. J Cell Mol Med 24(15):8326–8349
Acknowledgements
The authors thank all the staff in the Department of Otorhinolaryngology Head and Neck Surgery of NanFang Hospital for their support during the study.
Funding
This work was supported by the National Natural Science Foundation of China [grant number 81902774]; the Natural Science Foundation of Guangdong Province [grant number 2020A1515010176]; the Medical Scientific Research Foundation of Guangdong Province of China [grant number A2020078]; and the Science and Technology Planning Project of Guangzhou [grant number 202102010041].
Author information
Authors and Affiliations
Contributions
Study concepts: FW. Study design: XL, XP. Data acquisition: XY, LC, JL, HF, YY, WL. Quality control of data and algorithms: HH, SW, JL. Data analysis and interpretation: XY, HH, HF. Statistical analysis: XY, DL, HF, ZC. Manuscript preparation: XY. Manuscript editing: XY, XP, XL. Manuscript review: FW. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethical approval
This retrospective study was approved by the Ethics Committee of Nanfang Hospital of Southern Medical University (Ethical review approval no.: NFEC-2017-165).
Consent to participate
All individual participants included in the study obtained informed consent on first admission.
Consent to publish
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Yuan, X., Feng, H., Huang, H. et al. Systemic immune-inflammation index during treatment predicts prognosis and guides clinical treatment in patients with nasopharyngeal carcinoma. J Cancer Res Clin Oncol 149, 191–202 (2023). https://doi.org/10.1007/s00432-022-04506-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00432-022-04506-z