Abstract
Evaluation of guidelines in actual practice is a crucial step in guideline improvement. A retrospective evaluation of the Dutch guideline for children with fever without an apparent source (FWS) showed 50% adherence in young infants. We prospectively evaluated adherence to the Dutch guideline and its impact on management in current practice. Prospective observational multicenter cross-sectional study, including children 3 days to 16 years old presented for FWS at one of seven emergency departments in participating secondary and tertiary care hospitals in the Netherlands. Adherence to the Dutch FWS guideline, adapted from the National Institute for Health and Care Excellence (NICE) guideline, was evaluated, and patterns in non-adherence and the impact of non-adherence on clinical outcomes and resource use were explored. Adherence to the guideline was 192/370 (52%). Adherence was lowest in patients categorized as high risk for severe infection (72/187, 39%), compared to the low-risk group (64/73, 88%). Differences in adherence were significant between risk categories (P < 0.001) but not between age categories. In case of non-adherence, less urinalysis, fewer bacterial cultures (blood, urine, and cerebral spinal fluid), and less empirical antibiotic treatment were performed (P < 0.050). Clinical outcomes were not significantly different between the non-adherence and the adherence group, particularly regarding missed severe infections.
Conclusions: We found a high non-adherence rate of 48%, which did not lead to unfavorable clinical outcomes. This substantiates the need for a critical reevaluation of the FWS guideline and its indications for bacterial cultures, viral testing, and antibiotic treatment.
What is Known: • Despite the development of national guidelines, variation in practice is still substantial in the assessment of febrile children to distinguish severe infection from mild self-limiting disease. • Previous retrospective research suggests low adherence to national guidelines for febrile children in practice. | |
What is New: • In case of non-adherence to the Dutch national guideline, similar to the National Institute for Health and Care Excellence (NICE) guideline from the United Kingdom, physicians have used fewer resources than the guideline recommended without increasing missed severe infections. |
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Fever without an apparent source (FWS) is one of the most common reasons for children to visit the Emergency Department (ED) [1]. Most cases of FWS are caused by a mild self-limiting infection, while approximately 6–15% is caused by a severe infection requiring immediate treatment [2]. Clinical presentation is often nonspecific in young children, hampering prompt recognition and adequate management. This diagnostic uncertainty in differentiating severe from self-limiting infections, combined with a higher incidence of severe infection in young infants, leads to high use of ED resources increasing the burden for children presenting with FWS. Likewise, healthcare costs increase, with an almost fivefold higher use of ED resources among infants younger than 3 months compared to children older than 6 months [3]. The Dutch Association of Paediatrics published the national guideline “Fever in secondary care setting in children aged 0–16 years” in 2013, aiming to improve early recognition of severe infections without increasing unnecessary diagnostic testing [4]. The Dutch guideline, adapted from the National Institute for Health and Care Excellence (NICE) of the United Kingdom, provides a step-by-step pathway to assess the risk of infection and subsequently recommends diagnostic testing and treatment.
In general, the purpose of guidelines is to support consistent and effective evidence-based health care and improve clinical outcomes. Practice variation in FWS management, however, remains substantial [5]. A multicenter study reported wide variation in prescriptions of broad-spectrum antibiotics in febrile children between European EDs, of which at least half of the participating EDs had implemented the Dutch or NICE guideline [6]. In a study on the impact of FWS guidelines, the availability of a guideline was not associated with reduced direct costs, and some guidelines did not result in the improvement of clinical outcomes [7]. Thus, the presence of a guideline does not guarantee a positive impact on clinical outcomes. This substantiates the need for guideline evaluation to assess its adherence and applicability in current practice. In turn, this knowledge may reduce unwanted practice variation and ineffective use of guidelines or provide targets for guideline improvement. Evaluation of guideline adherence and outcomes in current practice is a crucial step in guideline development. After the implementation of the Dutch guideline, we retrospectively evaluated guideline adherence, measuring low to moderate adherence in children younger than 3 months without the impact of non-adherence on clinical outcomes [8]. This suggests possibilities for safely reducing diagnostics and treatment in children with FWS. Multicenter prospective evaluation of adherence to the national guideline, including all age groups, is needed to corroborate these findings.
Thus, this prospective multicenter study evaluated the adherence to diagnostic and treatment recommendations of the Dutch national guideline for children aged 0–16 years with FWS. As our secondary aims, we investigated patterns in non-adherence and the impact of non-adherence on clinical outcomes and on the use of diagnostic and therapeutic resources.
Materials and methods
Study design and participants
This prospective observational multicenter study included children presenting with FWS at the ED in one of seven participating secondary and tertiary care hospitals, organized in the Pediatric Research and Evaluation Network Amsterdam, in the North-West region of the Netherlands from December 2020 to May 2022. Inclusion criteria, directly adopted from the national guideline, were (I) children aged 3 days to 16 years; (II) presenting with FWS, defined as a temperature of ≥ 38.0 °C at home or during ED visit, and (IIA) no evident focus of infection after history and physical examination or (IIB) a clinical presentation not fitting the potential focus according to the treating physician [4]. Exclusion criteria were children with hospital-acquired or post-operative fever and children initially presenting with a typical febrile seizure in case of a clear focus for the fever.
Setting
The participating hospitals include one academic tertiary care center, five secondary care teaching hospitals, and one secondary care non-teaching hospital. In the Netherlands, most children are seen by a general practitioner first, in some cases by an emergency physician. Subsequently, all children with fever younger than three months or older children without an apparent source or a sick appearance are referred to the ED for evaluation by a pediatrician or pediatric resident. In this region, the average driving time to primary or secondary care settings should be less than 20 min. National ED visits on average range between 75 and 190 visits per 1000 children [9]. Due to COVID-19 measures, the number of ED and general practitioner visits in 2020 was almost 12% less than in 2019 which mostly normalized after the first wave (December 2020) [9, 10].
FWS guideline definitions
Definitions, specific targeted infections, and age categorization of patients in this study were all in accordance with the national guidelines. Severe infection was defined according to the guidelines as a confirmed Herpes Simplex virus (HSV) encephalitis, bacteriemia, bacterial meningitis, urinary tract infection (UTI), septic arthritis, osteomyelitis, pneumonia, or Kawasaki disease [4]. The guideline recommends separate diagnostic and treatment pathways based on age category of the patient and the risk of severe infection category (Fig. 1). Age categories are defined by the guideline as children younger than 1 month, 1 to 3 months, and older than 3 months, and risk of severe infection is categorized as low (green), intermediate (amber), and high risk (red) (Fig. 1). The risk of severe infection is categorized based on a combination of age, red or amber flags of the NICE traffic light system (supplementary Table 1), Rochester criteria for children younger than 2 months (supplementary Table 2), and the results of initial diagnostic testing.
The Dutch national fever without an apparent source guideline recommendations. Pathway for diagnostic and treatment recommendations per age category as defined by the Dutch FWS guideline and derived from the NICE traffic light system. *Rochester criteria is only applicable in children aged younger than 2 months. CSF cerebral spinal fluid, CRP C-reactive protein, HSV herpes simplex virus, IV intravenous, PCR polymerase chain reaction assay
Initial diagnostic testing includes dipstick urinalysis, C-reactive protein (CRP) and, in children younger than 3 months, white blood cell and differential count (WBC) (Fig. 1). Subsequently, patients younger than 1 month can be categorized as having an intermediate or high risk of severe infection while patients aged 1 to 3 months or older than 3 months can be categorized as having a low, intermediate or high risk of severe infection (Fig. 1). Age younger than 13 days was considered a red flag and therefore always categorized as high risk. Per the age and risk of infection category, the guideline provides recommendations for additional diagnostic testing (bacterial cultures, viral polymerase chain reaction (PCR) testing, cerebral spinal fluid (CSF) analysis, and chest X-rays), hospital admission, and empirical antimicrobial treatment similar to the NICE guideline (Fig. 1). Treatment recommendations include empirical intravenous (IV) antibiotics, oral antibiotics, and IV acyclovir.
When rapid viral testing was positive for influenza or respiratory syncytial virus (RSV) in its endemic season, the guideline states to only perform a diagnostic work-up for a potential severe infection in case of an ill-appearing patient. In the case of a positive rapid viral test and a well-appearing patient, bacterial cultures and empirical antibiotic treatment were not indicated. Since rapid diagnostic testing of severe acute respiratory syndrome coronavirus (SARS-CoV-) 2 was implemented in the course of the study and recommendations for this novel virus were not yet described in the FWS guideline, we calculated adherence for SARS-CoV-2 positive and negative patients separately. Adherence in patients with a positive rapid test for SARS-CoV-2, the coronavirus disease 2019 (COVID-19) cohort, was evaluated similarly to influenza and RSV infection recommendations. For further analyses of patterns and impacts of adherence, patients with a positive SARS-CoV-2 rapid test were excluded.
Data collection
Eligible patients were managed in the ED according to the judgment of the treating physician. After informed consent was obtained, data regarding the ED visit evaluation and management was collected prospectively by the treating physician. These data included patient characteristics, history and physical examination during ED visit, diagnostic testing and treatment, and testing results and clinical outcomes collected seven days after the initial ED visit. Subsequently, adherence of each case to the Dutch FWS guideline was assessed.
Data analysis and outcomes
The primary study outcome was the proportion of cases with full adherence to all the recommendations of the guideline. Non-adherence was subdivided into non-adherence to diagnostic and/or treatment recommendations. Cases with an unclear adherence or diagnosis were discussed in the study team blinded for the hospital and treating physician. Antibiotic treatment performed while this was not recommended was also considered non-adherence. In case CRP or urinalysis was missing and the risk category could not be determined, the risk category was considered as missing data and considered as non-adherence.
For the secondary study outcomes, the adherence group and the non-adherence group were compared in terms of patient characteristics, clinical outcomes, and the use of diagnostic and therapeutic resources. For patterns in non-adherence, the patient characteristics were compared between adherence groups. For the clinical outcomes, we assessed potentially missed severe infections based on reported delayed antibiotic treatment (> 12 h) in confirmed bacterial infections, ED revisits, and (re)admissions within 7 days after the initial visit. Further clinical outcomes included final discharge diagnosis as reported in medical charts (see supplementary material for diagnostic criteria), need for IV fluids, O2 support or intensive care unit (ICU) transfer, mortality, length of admission, and delayed antibiotic treatment (> 12 h) overall. The use of resources was measured as the number of performed tests and treatments per age and risk category in the adherence and the non-adherence groups. For reporting of data, a STROBE data reporting checklist can be found in supplementary materials [11].
Statistical methods
SPSS Statistics version 26.0 (IBM Corp, New York, USA) was used for all analyses. For continuous variables, means with standard deviations or medians with interquartile ranges were calculated. Differences between groups in not-normally distributed variables were analyzed with a Mann–Whitney U-test. Categorical variables were depicted in proportions and differences between proportions were analyzed using Pearson’s Fisher’s exact test. The following potential predictors of non-adherence were identified: age category, risk of severe infection category, and comorbidity. As the guideline did not provide a definition of comorbidity, in this analysis, we defined comorbidity as a chronic underlying condition that is expected to last at least one year [12]. All variables with clinical importance and/or a P < 0.250 in univariable regression analysis were included in the multivariable regression model after checking for collinearity. For all comparisons, an alpha value of < 0.050 was considered statistically significant. The Bonferroni correction method was used to adjust p-values for multiple comparisons. With an expected adherence of 51% based on our previous study, a sample size of n = 384 was required to detect a prevalence of adherence to the guideline with a confidence level of 95% and a margin of error of 5% [8].
Study approval
The study protocol was approved by the Medical Ethics Committee of the Amsterdam University Medical Centers (W20_309 # 20.344), and a waiver for the Medical Research Involving Human Subjects Act was provided. Written informed consent was obtained from parents/guardians and/or children above the legal age of consent.
Results
Patient selection
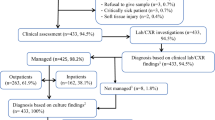
A total of 370 patients were included in the cohort and further analysis of adherence was performed on n = 333 after exclusion of SARS-CoV-2 positive patients identified with rapid viral testing upon arrival at the primary ED visit (Fig. 2).
Patient characteristics (n = 370)
Characteristics, number of performed diagnostic testing and treatment, final diagnoses, and clinical outcomes are shown in Table 1. Most patients were categorized as high risk (201/370, 54%). The overall hospital admission rate was 269/370 (73%) with higher proportions in the high-risk group (169/187, 90%) and medium-risk group (45/57, 80%) compared to low risk (28/73, 38%). Overall, the antibiotic treatment rate was 141/370 (38%), in the high-risk group 115/187 (62%) received antibiotics, in the medium-risk group 16/57 (28%), and 6/73 (8%) in the low-risk group. Of the patients categorized as high risk of severe infection, a lumbar puncture was performed in 88/201 (44%), of which 80/201 (39%) were tested for HSV and 61/201 (30%) patients were empirically treated with IV acyclovir. There were no ICU transfers or deaths in the cohort.
Severe infections
A final diagnosis of bacterial infection was confirmed in 56/370 (15%), a clinical diagnosis of pneumonia in 7/370 (2%) and HSV encephalitis in 2/370 (0.5%) (Table 1). Viral infections were identified in 153/370 (41%). Rapid viral testing identified a viral infection upon presentation in 53/370 (14%). A viral and bacterial coinfection was confirmed in 9/370 (2%). The bacterial infection rate correlated with the risk of severe infection according to the guideline categorization: 2/90 (2%) in the low-risk group compared to 6/62 (10%) in the intermediate and 48/209 (24%) in the high-risk group. Similarly, the bacterial infection rate was higher in patients younger than 1 month compared to the older age categories (Table 1).
Adherence (n = 370)
Full adherence to all recommendations was reported in 192/370 (52%) and after exclusion of patients with positive SARS-CoV-2 rapid testing 167/333 (50%) (Fig. 2). Non-adherence to one recommendation was 67/370 (18%), to two recommendations was 47/370 (13%), to three separate recommendations was 27/370 (7%), and to four or more recommendations was 39/370 (11%).
Patterns of non-adherence (n = 333)
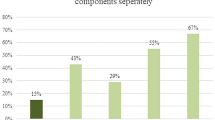
For our secondary aim, we evaluated patterns in non-adherence by describing patient characteristics per adherence group, excluding patients with a positive SARS-CoV-2 rapid test. In case of non-adherence, mostly blood or urine cultures and lumbar punctures were not performed (Fig. 3). Antibiotics were not started in 72/187 (39%) of patients in whom empirical treatment was recommended (Fig. 3). Figure 4 shows adherence per age and risk category. Between participating hospitals, adherence ranged from 39 to 63% with characteristics per site reported in supplementary Table 5. Adherence was lowest in patients younger than 1 month categorized as the intermediate risk of severe infection 5/19 (26%) and highest in patients 1 to 3 months categorized as low risk 37/39 (95%). Differences in adherence were significant between risk categories (P < 0.001) but not between age categories (P = 0.095). In multivariable logistic regression (including age category, risk of severe infection, and comorbidity), only the risk category was an independent predictor for non-adherence: the high-risk category showed an adjusted odds ratio of 11.67 (95% confidence interval 5.18–26.25, P < 0.001) compared to the low-risk category. There were no significant differences between the adherence and the non-adherence group in the number of severe infections or time of ED visit (Table 2).
Adherence per recommendation. Proportions of performed diagnostic and therapeutic recommendations (sample n = 333), with the total bar representing all patients for which CRP (n = 333), urinalysis (n = 333), blood culture (n = 206), urine culture (n = 190), cerebral spinal fluid (CSF) culture (n = 98), admission (n = 244), or antibiotic treatment (n = 187) was recommended according to the FWS guideline. Patients with a positive rapid test for SARS-CoV-2 were excluded from the analysis
Adherence per age and risk category. Adherence depicted in the bars is shown in proportions per risk category and per age category, as categorized according to the FWS guideline (sample n = 333). The number of patients per category was as follows: < 1 month, high risk, n = 82; 1–3 months, high risk, n = 89; > 3 months, high risk, n = 16; < 1 month, intermediate risk, n = 19; 1–3 months, intermediate risk, n = 10; > 3 months, intermediate risk, n = 28; 1–3 months, low risk; n = 39; and > 3 months, low risk, n = 34. Patients with a positive rapid test for SARS-CoV-2 were excluded from the analysis
Impact of non-adherence (n = 333)
To evaluate the impact of non-adherence, we compared the clinical outcomes (Table 2) and the number of performed diagnostic testing and treatment in the adherence group versus the non-adherence group (Tables 3 and 4). The median admission rate was one day shorter in the non-adherence group (P = 0.010). There were no significant differences in mortality, ICU admission, readmission rates, or missed severe infections between the adherence and non-adherence groups (Table 2). If treated according to the guideline, 187 patients would have received antibiotic treatment of which 53 patients were diagnosed with a bacterial infection. In the adherence group, 47% of patients without confirmed bacterial infection received antibiotics therapy while 31% in the non-adherence group received antibiotics.
Regarding missed severe infections, the FWS guideline did not recommend antibiotic treatment in three patients (2%) in the adherence group, who were later diagnosed with a UTI (n = 2) or bacterial meningitis. In the non-adherence group, five patients (3%) did not receive antibiotic treatment while this was recommended. These patients received delayed antibiotic treatment and were later diagnosed with UTI (n = 3), UTI with bacteremia, or bacterial with viral meningitis. In the high-risk category, there were significantly lower rates of blood/urine cultures, lumbar punctures, and antimicrobial treatment in the non-adherence group (Table 3). In the low-risk category, significantly fewer cultures were performed in patients younger than 1 month and urinalysis and admission in patients older than three months (Table 4).
Adherence in COVID-19 cohort (n = 37)
In 26/37 (70%) of the COVID-19 cohort, there was no ill appearance reported, and the other 11/37 (30%) presented with an ill appearance, meaning the presence of a red flag. Adherence was 23/37 (62%) in the COVID-19 cohort. Non-adherence in this cohort consisted of bacterial cultures or empirical antibiotic treatment while there was no ill appearance or incomplete bacterial cultures or antibiotic treatment in case of an ill appearance. Hospital admission rate was 24/37 (65%), and IV antibiotic treatment was 4/37 (11%). One patient was diagnosed with Multisystem Inflammatory Syndrome in Children, one co-infection with influenza was reported, and one bacterial coinfection with a UTI.
Discussion
We found adherence to the Dutch national guideline in half of children presenting with FWS at the ED. Adherence to the guideline was lower in children categorized as high risk of severe infection. In the non-adherence group, significantly fewer urinalysis, bacterial cultures, lumbar punctures, and antimicrobial treatments were performed compared to the adherence group with no differences in missed severe infections.
In our previous retrospective study in infants younger than 3 months, adherence was 51% with fewer cultures and antibiotic treatment performed in case of non-adherence. We were able to corroborate these findings in the current more multicentered and prospectively performed study covering all age groups [8]. Adherence was particularly low in the high-risk groups, as well as the younger age groups, for which the guideline provides more numerous recommendations compared to the older or low-risk patients. While these are the first studies describing adherence to the Dutch guideline, the NICE guideline for FWS similarly showed low adherence across several European EDs in bacterial cultures and antibiotic treatment [13]. Regarding the measurement of NICE-recommended vital signs, a 52% non-adherence was reported [14]. Non-adherence can be explained by several factors concerning the physician’s knowledge, attitudes, and behavior as well as complicated or variating guidelines [15]. A comparison of ten high-income countries showed wide variation between guidelines in definitions of high risk for severe infection [16]. This variation in defining a patient as high risk, and thus indicating cultures and treatment, could play a role in the low adherence in patients categorized as high risk in this study. We deliberately did not include a survey of reasons for non-adherence so as to not affect the behavior of physicians during our evaluation. Particularly in missed severe infections, it is of importance to understand the reasoning behind a physician’s non-adherence. Some patterns of non-adherence could indicate a lack of physician’s awareness which should be targeted for education to improve adherence. For instance, less urinalysis and urine cultures were performed than recommended by the guidelines. Moreover, often urine cultures were not performed after a negative urinalysis while urinalysis of young infants does not have 100% rule-out value for a UTI [17]. As UTIs are the most frequent cause of FWS yet their clinical presentation is remarkably nonspecific, this requires specific attention [18].
Our findings raise the question of whether interventions need to be applied to increase adherence, or if these adherence rates are actually a symptom of decreased applicability of the current FWS guideline or its acceptability for physicians or patients. Physicians did not start antibiotic treatment in the majority of children aged 1 to 3 months categorized as high risk, indicating that physicians applied a higher threshold to antibiotic treatment than the guideline. The presence of one red flag already categorizes as high risk, while in a validation study of the traffic light system, most red flags showed little individual rule-in value for severe infection across multiple datasets [19]. Furthermore, a large meta-analysis calculated roughly half the rate of severe infection in this age group compared to younger infants [20]. The new United States guideline published in 2022 similarly suggested a less defensive approach to well-appearing febrile infants while the 2021 update of the NICE guideline remained to recommend their traffic light system and concurrent recommendations [21, 22]. If all patients were treated according to the guideline, 187 patients would have received antibiotic treatment of which less than a third was diagnosed with a bacterial infection. Importantly, there was no increase in missed severe infections or adverse clinical outcomes in our study due to non-adherence. This substantiates the need for a critical reevaluation of the FWS guideline and its indications for bacterial cultures and treatment. As we reported in our international comparison study, guidelines for febrile children are largely similar across countries and continents, and thus, our results and the need for critical evaluation of guidelines are generalizable to many high-income countries in addition to countries using the NICE guideline [16].
Moreover, rapid viral diagnostic testing, including SARS-CoV-2, RSV, and influenza, revealed a plausible source in 14% of all FWS cases. Although these tests may mostly be of value during their endemic seasons, this illustrates the potential to decrease further bacterial testing and treatment. In line with the low rate of bacterial coinfections in our cohort, other studies showed a significantly lower risk for severe infection in febrile infants positive for viral infections compared with virus-negative infants [23, 24]. As viral PCR testing for enterovirus, although not available as a rapid test, has also shown potential to shorten admission duration and use of antibiotic treatment, evidence-based guidance on viral testing (both rapid and non-rapid methods) should be implemented in the revised FWS guideline [25]. Considering we found a viral cause in our cohort in 41% with low rates of bacterial coinfection, future research efforts in rapid viral testing are needed to decrease ED resource use.
This guideline evaluation study faced several limitations. First, we were not able to register patients presented at the ED who were not recruited by the physician or refused participation. However, considering the distribution of high-risk patients was equal to our previous retrospective sample, the amount of selection bias may therefore be limited [8]. Second, adherence could be overestimated if participation in the study influenced the physician’s behavior. As our primary and secondary outcomes are very comparable to our previous adherence study, which is less vulnerable to participation bias due to its retrospective design, the impact on outcomes may be negligible. Third, our inclusion partly took place during the COVID-19 pandemic, which could have influenced the epidemiology of other pathogens and healthcare-seeking behavior. Fourth, we did not include a random effects model to analyze differences between sites in addition to the adherence per site and site-specific data. Fifth, although methodologically explainable considering participation bias, missing the rationale of physicians for non-adherence is an important limitation in the interpretation of our results.
In conclusion, in our multicenter prospective evaluation of the Dutch guideline for children presenting with FWS the high non-adherence rate did not lead to unfavorable clinical outcomes. In case of non-adherence, physicians have used fewer ED resources than the guideline recommended without increasing missed severe infections. This substantiates the need for a critical reevaluation of the FWS guideline and its indications for bacterial cultures, viral testing, and antibiotic treatment.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Change history
06 May 2024
A Correction to this paper has been published: https://doi.org/10.1007/s00431-024-05594-4
Abbreviations
- COVID-19:
-
Coronavirus disease 2019
- CRP:
-
C-reactive protein
- CSF:
-
Cerebral spinal fluid
- ED:
-
Emergency department
- IV:
-
Intravenous
- HSV:
-
Herpes Simplex virus
- FWS:
-
Fever without an apparent source
- NICE:
-
National Institute for Health and Care Excellence
- PCR:
-
Polymerase chain reaction
- RSV:
-
Respiratory syncytial virus
- SARS-CoV-2:
-
Severe acute respiratory syndrome coronavirus 2
- ICU:
-
Intensive care unit
- UTI:
-
Urinary tract infection
- WBC:
-
White blood cell count
References
Alpern ER, Stanley RM, Gorelick MH, Donaldson A, Knight S, Teach SJ et al (2006) Epidemiology of a pediatric emergency medicine research network: the PECARN Core Data Project. Pediatr Emerg Care 22(10):689–699
Nijman RG, Vergouwe Y, Thompson M, van Veen M, van Meurs AH, van der Lei J et al (2013) Clinical prediction model to aid emergency doctors managing febrile children at risk of serious bacterial infections: diagnostic study. BMJ 346:f1706
Leigh S, Grant A, Murray N, Faragher B, Desai H, Dolan S et al (2019) The cost of diagnostic uncertainty: a prospective economic analysis of febrile children attending an NHS emergency department. BMC Med 17(1):48
Oostenbrink RN, Tuut RG, Venmans MK, Richtlijn L (2013) Koorts in de tweede lijn bij kinderen van 0–16 jaar. Kindergeneeskunde NVK 208. Available at: 2013 https://www.nvk.nl/Portals/0/richtlijnen/koorts/koortsrichtlijn.pdf
Rogers AJ, Kuppermann N, Anders J, Roosevelt G, Hoyle JD Jr, Ruddy RM et al (2019) Practice variation in the evaluation and disposition of febrile infants ≤ 60 days of age. J Emerg Med 56(6):583–591
Hagedoorn NN, Borensztajn DM, Nijman R, Balode A, von Both U, Carrol ED et al (2020) Variation in antibiotic prescription rates in febrile children presenting to emergency departments across Europe (MOFICHE): a multicentre observational study. PLoS Med 17(8):e1003208
Aronson PL, Thurm C, Williams DJ, Nigrovic LE, Alpern ER, Tieder JS et al (2015) Association of clinical practice guidelines with emergency department management of febrile infants ≤ 56 days of age. J Hosp Med 10(6):358–365
Klarenbeek NN, Keuning M, Hol J, Pajkrt D, Plötz FB (2020) Fever without an apparent source in young infants: a multicenter retrospective evaluation of adherence to the Dutch guidelines. Pediatr Infect Dis J 39(12):1075–1080
Gijsen R, Meijerink L, Hulshof T, Reuser M, Kommer G (2023) Zorggebruik op de spoedeisende hulp in kaart gebracht. Notitie Kosten van Ziekten studie. Overview of A&E care use: Rijksinstituut voor Volksgezondheid en Milieu RIVM
Lambooij M, Heins M, Meijer M, Vader S, de Jong J, Janssen L (2022) Het mijden van huisartsenzorg tijdens de coronapandemie. Inzicht in verminderde huisartsenzorg tijdens de coronapandemie. Avoiding GP care during the coronavirus pandemic insight in reduction of GP care during the coronavirus pandemic: Rijksinstituut voor Volksgezondheid en Milieu RIVM
von Elm E, Altman D, Egger M, Pocock S, Gotzsche P, Vandenbroucke J The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies
Simon TD, Cawthon ML, Stanford S, Popalisky J, Lyons D, Woodcox P et al (2014) Pediatric medical complexity algorithm: a new method to stratify children by medical complexity. Pediatrics 133(6):e1647–e1654
Tan CD, van der Walle EEPL, Vermont CL, von Both U, Carrol ED, Eleftheriou I et al (2022) Guideline adherence in febrile children below 3 months visiting European Emergency Departments: an observational multicenter study. Eur J Pediatr 181(12):4199–4209
van de Maat J, Jonkman H, van de Voort E, Mintegi S, Gervaix A, Bressan S et al (2020) Measuring vital signs in children with fever at the emergency department: an observational study on adherence to the NICE recommendations in Europe. Eur J Pediatr 179(7):1097–1106
Cabana MD, Rand CS, Powe NR, Wu AW, Wilson MH, Abboud PA, Rubin HR (1999) Why don’t physicians follow clinical practice guidelines? A framework for improvement Jama 282(15):1458–1465
Graaf S, Keuning MW, Pajkrt D, Plötz FB (2023) Fever without a source in children: international comparison of guidelines. World J Pediatr 19(2):120–128
Esposito S, Rinaldi VE, Argentiero A, Farinelli E, Cofini M, D’Alonzo R et al (2018) Approach to neonates and young infants with fever without a source who are at risk for severe bacterial infection. Mediators Inflamm 2018:4869329
Kaufman J, Temple-Smith M, Sanci L (2019) Urinary tract infections in children: an overview of diagnosis and management. BMJ Paediatr Open 3(1):e000487
Kerkhof E, Lakhanpaul M, Ray S, Verbakel JY, Van den Bruel A, Thompson M et al (2014) The Predictive Value of the NICE “Red Traffic Lights” in Acutely Ill Children. PLoS ONE 9(3):e90847
Biondi EA, Lee B, Ralston SL, Winikor JM, Lynn JF, Dixon A, McCulloh R (2019) Prevalence of bacteremia and bacterial meningitis in febrile neonates and infants in the second month of life: a systematic review and meta-analysis. JAMA Network Open 2(3):e190874
Pantell RH, Roberts KB, Adams WG, Dreyer BP, Kuppermann N, O’Leary ST et al (2021) Clinical practice guideline: evaluation and management of well-appearing febrile infants 8 to 60 days old. Pediatrics 148(2)
National Institute for Health and Care Excellence guideline (2021) Fever in under 5s: assessment and initial management. Available: 2021. https://www.nice.org.uk/guidance/ng143
Mahajan P, Browne LR, Levine DA, Cohen DM, Gattu R, Linakis JG et al (2018) Risk of bacterial coinfections in febrile infants 60 days old and younger with documented viral infections. J Pediatr 203:86-91.e2
Greenfield BW, Lowery BM, Starke HE, Mayorquin L, Stanford C, Camp EA, Cruz AT (2021) Frequency of serious bacterial infections in young infants with and without viral respiratory infections. Am J Emerg Med 50:744–747
Lafolie J, Labbé A, L’Honneur AS, Madhi F, Pereira B, Decobert M et al (2018) Assessment of blood enterovirus PCR testing in paediatric populations with fever without source, sepsis-like disease, or suspected meningitis: a prospective, multicentre, observational cohort study. Lancet Infect Dis 18(12):1385–1396
Acknowledgements
We are thankful for the hard work and enthusiasm of the physicians and medical students supporting patient inclusion and data collection. Finally, we are most grateful to all the parents and children participating in this study.
Funding
This study would not have been possible without the financial support of the Tergooi Scientific Committee.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Following authors contributed to patient inclusion, and data collection: N Klarenbeek, H Bout, A Broer, M Draaijer, N Hollander, C Nusman, E Oostenbroek, M Ridderikhof, M Roelofs, E van Rossum, S Schouten, P Taselaar, K Vasse, J vd Zande and R Zuurbier. Data analysis was performed by M Keuning and M Bijlsma. The first draft of the manuscript was written by M Keuning, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Medical Ethics Committee of the Amsterdam University Medical Centers (W20_309 # 20.344), and a waiver for the Medical Research Involving Human Subjects Act was provided. The study was performed in accordance with the Declaration of Helsinki, and written informed consent was obtained from parents/guardians and/or children above the legal age of consent.
Competing interests
The authors declare no competing interests.
Additional information
Communicated by Tobias Tenenbaum
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised due to author names in the proof were incorrectly adjusted.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Keuning, M.W., Klarenbeek, N.N., Bout, H.J. et al. Prospective multicenter evaluation of adherence to the Dutch guideline for children aged 0–16 years with fever without a source—febrile illness in children (FINCH) study. Eur J Pediatr 183, 2921–2933 (2024). https://doi.org/10.1007/s00431-024-05553-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-024-05553-z