Abstract
Bronchiolitis is a common cause of hospitalization in infants. The long-lasting impact of hygiene and social behavior changes during the pandemic on this disease is debated. We investigated the prevalence of hospitalized cases, clinical severity, and underlying risk factors before and during pandemic. The study was conducted in 27 hospitals in Italy and included infants hospitalized for bronchiolitis during the following four periods: July 2018-March 2019, July 2020-March 2021, July 2021-March 2022, and July 2022-March 2023. Data on demographics, neonatal gestational age, breastfeeding history, underlying chronic diseases, presence of older siblings, etiologic agents, clinical course and outcome were collected. A total of 5330 patients were included in the study. Compared to 2018–19 (n = 1618), the number of hospitalizations decreased in 2020–21 (n = 121). A gradual increase was observed in 2021–22 (n = 1577) and 2022–23 (n = 2014). A higher disease severity (need and length of O2-supplementation, need for non-invasive ventilation, hospital stay) occurred in the 2021–22 and, especially, the 2022–23 periods compared to 2018–19. This tendency persisted after adjusting for risk factors associated with bronchiolitis severity.
Conclusions: Compared to adults, COVID-19 in infants is often asymptomatic or mildly symptomatic and rarely results in hospitalization. This study indicates that the pandemic has indirectly induced an increased burden of bronchiolitis among hospitalized infants. This shift, which is not explained by the recognized risk factors, suggests the existence of higher infant vulnerability during the last two seasons.
What is known: • The pandemic led to a change in epidemiology of respiratory diseases • Large data on severity of bronchiolitis and underlying risk factors before and during COVID-19 pandemic are scarce | |
What is new: • Compared to pre-pandemic period, hospitalizations for bronchiolitis decreased in 2020–21 and gradually increased in 2021–22 and 2022–23 • Compared to pre-pandemic period, higher disease burden occurred in 2021–22 and, especially, in 2022–23. This tendency persisted after adjusting for risk factors associated with bronchiolitis severity • The interplay among viruses, preventive measures, and the infant health deserves to be further investigated |
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
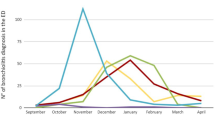
Bronchiolitis, a lower respiratory tract infection affecting the small airways, is a common cause of hospitalization in infancy [1]. In the Northern Hemisphere, bronchiolitis typically occurs from October to March and is a recognized burden for hospital services [2,3,4]. A drastic reduction in bronchiolitis cases was observed during the first pandemic year (2020–21) [5, 6]. Social distancing, reduction of day care attendance, hygienic practices such as handwashing with antiseptic gels, and the use of protective masks by adults and older children are believed to be responsible for this shift [7]. During the second year of the pandemic (2021–22), an increased number of bronchiolitis with more severe cases often occurring before the autumn-winter season has been observed [8, 9]. Some authors hypothesized that the limited exposure to microorganisms during the first pandemic year led to a higher number of severe cases than suggested by historical data [8]. However, other factors that emerged during the pandemic have also been claimed to favor this shift. First, a drastic change in respiratory syncytial virus epidemiology, the main cause of bronchiolitis [10, 11]. Second, a decrease in breastfeeding practice, a protective factor against severe bronchiolitis [12,13,14]. Finally, older siblings, who had not been exposed to respiratory viruses during the initial pandemic phase, might have facilitated an increased viral transmission after the relaxation of preventive measures in the following years [15, 16].
Limited epidemiological data support these hypotheses [10]. Furthermore, little evidence is available on bronchiolitis during the season 2022–23. We conducted a multicenter study on infants hospitalized for bronchiolitis in the Lombardy region (Italy), which is considered the first COVID-19 epicenter in Europe. The primary aim of this study was to assess the prevalence and clinical severity of hospitalized cases before and during the pandemic. The secondary aim was to test whether main known risk factors explain the possible changes in bronchiolitis severity.
Methods
The IRIDE (“Investigating bRonchiolitis epidemiology During the pandemic Emergency”) study is a multicenter observational cohort study conducted in 27 hospitals in Lombardy, Italy. These hospitals, whose list is given in the supplementary online material (Table S1), account for > 80% of hospital bed capacity for pediatric patients in Lombardy. Eligible for the study were infants aged < 24 months, hospitalized for at least 12 h with a diagnosis of bronchiolitis and discharged by one of the hospitals participating in the study during the following four periods: July 2018—March 2019 (pre-pandemic period), July 2020—March 2021, July 2021—March 2022, and July 2022—March 2023. Since the outbreak of SARS-CoV-2 and the first restrictive measures to limit its spread occurred in Lombardy at the beginning of 2020, the period 2019–2020 was not considered. On the other hand, the three pandemic periods considered in this study were characterized by a gradual decrease in preventive and hygiene measures against viral circulation [16, 17]. Bronchiolitis cases not requiring hospitalization were excluded. To prevent patients transferred from one hospital to another from being enrolled twice, each center could recruit only those patients who had been discharged from their own facility.
The following ICD-9 codes were initially used: 46,611 (respiratory syncytial virus bronchiolitis), 46,619 (bronchiolitis caused by other infectious agents), 4801 (pneumonia due to respiratory syncytial virus), 0796 (respiratory syncytial virus infection), 51,881 (respiratory failure in children), 77,084 and 77,089 (respiratory failure in neonates). Subsequently, the clinical charts were retrieved, and only subjects with a history of acute respiratory tract infection of the upper airways in the previous days, followed by an acute onset of cough, diffuse crackles, and respiratory distress, were retained [4, 18]. For included subjects, the following data were retrospectively extracted from the clinical records: age at admission, sex, neonatal gestational age and body weight, any breastfeeding and duration of exclusive breastfeeding, number of older siblings, underlying chronic diseases that predispose to severe bronchiolitis (including bronchopulmonary dysplasia and severe congenital heart disease), occurrence of radiologically confirmed diagnosis of pneumonia during the bronchiolitis episode, infectious agent detected by nasopharyngeal aspirate, need and duration of O2-supplementation, use of non-invasive ventilation support (including Bi-PAP and C-PAP), need and duration of intensive care, need for invasive ventilation support, use of extracorporeal membrane oxygenation (ECMO), length of the whole hospital stay. Furthermore, fatal cases were also considered. All data were gathered and de-identified at each study center. They were then collected using REDCap tools hosted at the Ospedale Maggiore, Policlinico, Milan, Italy. The study was approved by the Ethical Committee of the coordinating center (Comitato Etico Milano Area2, Milan, code 186796, date of approval April 26, 2023) and by the other participating centers.
Statistical analysis
The distribution of continuous variables was visually tested using histograms and density plots. Parametric data were presented as mean and standard deviations and non-parametric data as median and interquartile range [IQR]. Categorical data were presented as absolute and relative frequencies. ANOVA and Kruskal-Wallis test were used to compare continuous variables, and Fisher exact test or Chi-squared test were used to compare categorical variables, as appropriate. The Bonferroni correction was used for multiple comparisons.
Mixed effect regression models were used to study differences in outcomes between the study periods, with the hospital as a random effect. Models’ results are expressed as linear coefficients or odds ratios for continuous and categorical outcomes, respectively, with 95% CI and p-values. Categorical outcomes included the need for O2-supplementation, use of non-invasive or invasive ventilation and the need for intensive care. Continuous outcomes included the length of O2-supplementation, intensive care stay and overall hospitalization. The four study periods (2018–19, 2020–21, 2021–22 and 2022–23) were tested as predictive variable. All models were adjusted for typical (age, sex, gestational age at birth, underlying chronic disease and positive testing for respiratory syncytial virus) and recently recognized (history of breastfeeding and number of older siblings) confounders of bronchiolitis severity. The models were performed both including all patients and then including only patients 12 months of age or less. Statistical significance was set at p < 0.05. The R software (R Foundation for Statistical Computing, Vienna, Austria) was used for the analysis.
Results
A total of 5330 patients hospitalized for bronchiolitis were included in the study. The median age of the included subjects was 2.3 [IQR 1.0–5.0] months, and 57% were males. The mean neonatal gestational age was 38.2 (± 2.7) weeks, and 957 (76%) had a history of breastfeeding. A total of 2479 (47%) patients had at least one older sibling, while 371 (6.9%) had an underlying chronic disease. A pneumonia was diagnosed in 905 (17%) infants. Respiratory syncytial virus was detected in 3292 (62%) cases. During hospitalization, 3712 (70%) patients required O2-supplementation, 2293 (43%) received non-invasive ventilation support, 78 (1.6%) required invasive ventilation support, and 6 (0.1%) were treated with ECMO. Three patients died in 2018–19 and one in 2021–22.
Data divided for the four study periods are reported in Table 1. The results of comparison between 2018–19 and the other periods are detailed in the online Supplementary Material.
Considering the main outcomes of the analysis, differences among the four periods were observed for the need and length of O2-supplementation, the need for and length of intensive care, and the length of the whole hospitalization. No difference was observed in the need for invasive ventilation support or ECMO (Table 2).
The results of the multiple models investigating the relation between bronchiolitis course and the pandemic periods after adjusting for typical and more recently recognized confounders are reported in Tables 3 and 4, respectively. The periods 2021–22 and 2022–23 were significantly associated with a higher need and length of O2-supplementation, increased use of non-invasive ventilation, and a longer hospitalization. No association among periods and the use of invasive ventilation support, and the need or length of intensive care was observed. The results of the models including exclusively patients 12 months of age or less (n = 4914) provided similar results (data are given in the online supplementary material, Tables S2 and S3).
Discussion
The IRIDE study investigated the epidemiology and clinical course of bronchiolitis in hospitalized infants during the pre-pandemic and pandemic periods. The study reveals a relevant reduction in bronchiolitis cases during the season 2020–21. More interestingly, it shows an increase in the number of hospitalizations, in the need and length of O2-supplementation, in the use of non-invasive ventilation, and a longer hospital stay in 2021–22 and, especially, in 2022–23 as compared to the pre-pandemic season. This tendency persists after adjusting for both typical risk factors for severe bronchiolitis such as young age, male sex, low neonatal gestational age, underlying chronic disease and the positivity for respiratory syncytial virus, and more recently recognized risk factors such as a decrease in breastfeeding and the presence of older siblings. Moreover, the number of patients requiring intensive care increased in 2021–22 and 2022–23. Nonetheless, the number of patients requiring invasive ventilation support and the length of intensive care stay did not change.
The drastic reduction in bronchiolitis during the season 2020–21 has been described in previous studies and confirms the efficacy of various preventive measures, such as social distancing, reduction of day care attendance, handwashing, and the use of masks [19, 20]. After the relaxation of pandemic-related measures, there was a significant increase in bronchiolitis burden in 2021–22 and 2022–23. Our data are supported by the literature, which confirms that the typical risk factors for severe bronchiolitis do not account for the observed tendency [13, 21, 22]. Decrease in breastfeeding and the presence of older siblings might also be new potential modulators of bronchiolitis severity [13, 21]. This comprehensive large-scale study shows for the first time that neither the main typical nor the newly recognized risk factors fully explain the higher burden of bronchiolitis observed in the pediatric wards during 2021–22 and 2022–23. It might be argued that the increased percentage of infants requiring O2-supplementation or non-invasive ventilation depends on a change in clinical practice over time (e.g., a higher threshold for hospitalization and a higher availability of devices for ventilation, respectively). However, the dramatic increase in the absolute number of infants requiring O2-supplementation from 2018–19 to 2012–22 (+ 21%) and 2022–23 (+ 60%) and of infants requiring intensive care (+ 54% and + 80%, respectively) does not support the latter hypothesis. Furthermore, recommendations for hospitalization and management did not vary during the study period in Italy [23]. This unexplained greater impact of bronchiolitis compared to the pre-pandemic period suggests the existence of higher vulnerability among infants. Notably, this vulnerability appears to persist for at least two bronchiolitis seasons. This hypothesis is in line with the findings of another study with a similar sample size including children affected with RSV infection in Spain [24].
The bronchiolitis burden was stronger in 2022–23 than in 2021–22. We have no clear-cut explanation for this finding. It is tempting to assume that a further relaxation of restrictive measures in 2022–23 accounts, at least in part, for this observation.
The number of patients requiring intensive care increased in 2021–22 and in 2022–23 compared to that of the pre-pandemic period. Nonetheless, the number of patients requiring invasive ventilation support and the length of intensive care stay remained stable. The results of the regression analysis suggest that low neonatal gestational age and underlying chronic diseases played a crucial role in the increased need for intensive care [25, 26].
This study has some limitations. It relied on retrospective design. ICD-10 codes were not used as they are not yet implemented for discharge diagnosis coding in Italy. Additionally, the use of ICD codes for case identification might not have captured all cases accurately. To counterbalance this risk, we used a wide range of codes and, then, all diagnoses were reviewed according to well-established criteria. Furthermore, our analysis focused uniquely on hospitalized infants. This decision was made because during the first two pandemic years, many infants with mild diseases that were previously managed uniquely by primary care physicians were directed to the emergency units. This redirection was partly due to organizational challenges in providing care to infants with a potential SARS-CoV-2 infection outside the hospital setting [27, 28]. Therefore, including infants who were not hospitalized might overestimate cases requiring emergency care during the first pandemic phases. The management of bronchiolitis may differ among centers. Mixed effects models were employed to reduce the potential for this issue. The study strengths lie in its large sample size, the high number of involved centers, and the collection of individual clinical and laboratory data. Furthermore, the main risk factors for severe bronchiolitis were considered. Finally, we did not have data on the immunological profile (e.g., levels of immunoglobulins) or changes in the respiratory microbiome over the four study periods. Therefore, the hypothesis of higher vulnerability remains only speculative.
Conclusions
Compared to adults, COVID-19 in infants is often asymptomatic or mildly symptomatic and rarely results in hospitalization [28, 29]. The IRIDE study indicates that the pandemic has indirectly induced an increased prevalence and severity of bronchiolitis requiring hospitalization. This shift, which is not explained by the main typical or newly recognized risk factors for severe bronchiolitis, suggests the existence of higher infant vulnerability during the last two seasons.
Availability of data and material
Upon reasonable request to the corresponding author.
Code availability
Not applicable.
Change history
07 August 2024
A Correction to this paper has been published: https://doi.org/10.1007/s00431-024-05707-z
Abbreviations
- COVID-19:
-
Coronavirus Disease 2019
- ECMO:
-
Extracorporeal Membrane Oxygenation
References
Meissner HC (2016) Viral Bronchiolitis in Children. N Engl J Med 374:62–72
Florin TA, Plint AC, Zorc JJ (2017) Viral bronchiolitis. Lancet 389:211–224
Carugno M, Dentali F, Mathieu G et al (2018) PM10 exposure is associated with increased hospitalizations for respiratory syncytial virus bronchiolitis among infants in Lombardy. Italy Environ Res 166:452–457
Milani GP, Cafora M, Favero C et al (2022) PM2.5, PM10 and bronchiolitis severity: A cohort study. Pediatr Allergy Immunol 33:e13853
Van Brusselen D, De Troeyer K, Ter Haar E et al (2021) Bronchiolitis in COVID-19 times: a nearly absent disease? Eur J Pediatr 180:1969–1973
Guitart C, Bobillo-Perez S, Alejandre C et al (2022) Bronchiolitis, epidemiological changes during the SARS-CoV-2 pandemic. BMC Infect Dis 22:84
Susana RM (2020) Bronchiolitis in the year of COVID-19. Arch Argent Pediatr 118:222–223
Hatter L, Eathorne A, Hills T et al (2021) Respiratory syncytial virus: paying the immunity debt with interest. Lancet Child Adolesc Health 5:e44–e45
Tuzger N, Milani GP, Folino F et al (2023) Referrals for Recurrent Acute Otitis Media With and Without Spontaneous Tympanic Membrane Perforation Through COVID-19: A Cross-Sectional Comparative Study. Pediatr Infect Dis J 42:e356–e357
Abu-Raya B, Viñeta Paramo M, Reicherz F et al (2023) Why has the epidemiology of RSV changed during the COVID-19 pandemic? EClinicalMedicine 61:102089
Chuang YC, Lin KP, Wang LA et al (2023) The Impact of the COVID-19 Pandemic on Respiratory Syncytial Virus Infection: A Narrative Review. Infect Drug Resist 16:661–675
Milani GP, Porro A, Agostoni C et al (2022) Breastfeeding during a Pandemic. Ann Nutr Metab 1–9
Dowse G, Perkins EJ, Stein HM et al (2023) Born into an isolating world: family-centred care for babies born to mothers with COVID-19. EClinicalMedicine 56:101822
Agostoni C, Guz-Mark A, Marderfeld L et al (2019) The Long-Term Effects of Dietary Nutrient Intakes during the First 2 Years of Life in Healthy Infants from Developed Countries: An Umbrella Review. Adv Nutr 10:489–501
Stera G, Pierantoni L, Masetti R et al (2021) Impact of SARS-CoV-2 Pandemic on bronchiolitis hospitalizations: the experience of an Italian tertiary center. Children (Basel) 8(7)
Berdah L, Romain AS, Rivière S, Schnuriger A, Perrier M, Carbajal R, Lorrot M, Guedj R, Corvol H (2022) Retrospective observational study of the influence of the COVID-19 outbreak on infants’ hospitalisation for acute bronchiolitis. BMJ Open 12:e059626
Facchin G, Bella A, Del Manso M et al (2023) Decline in reported measles cases in Italy in the COVID-19 era, January 2020 - July 2022: The need to prevent a resurgence upon lifting non-pharmaceutical pandemic measures. Vaccine 41:1286–1289
Milani GP, Bollati V, Ruggiero L et al (2021) Bronchiolitis and SARS-CoV-2. Arch Dis Child 106:999–1001
Ramos La Cuey B, Saloni-Gomez N, Ilundain López de Munain A et al (2023) The long-term boomerang effect of COVID-19 on admissions for non-COVID diseases: the ECIEN-2022 study. Eur J Pediatr. Online ahead of print
Di Mattia G, Nenna R, Mancino E et al (2021) During the COVID-19 pandemic where has respiratory syncytial virus gone? Pediatr Pulmonol 56:3106–3109
Mineva GM, Purtill H, Dunne CP et al (2023) Impact of breastfeeding on the incidence and severity of respiratory syncytial virus (RSV)-associated acute lower respiratory infections in infants: a systematic review highlighting the global relevance of primary prevention. BMJ Glob Health 8(2)
Bardsley M, Morbey RA, Hughes HE et al (2023) Epidemiology of respiratory syncytial virus in children younger than 5 years in England during the COVID-19 pandemic, measured by laboratory, clinical, and syndromic surveillance: a retrospective observational study. Lancet Infect Dis 23:56–66
Baraldi E, Lanari M, Manzoni P, Rossi GA, Vandini S, Rimini A, Romagnoli C, Colonna P, Biondi A, Biban P, Chiamenti G, Bernardini R, Picca M, Cappa M, Magazzù G, Catassi C, Urbino AF, Memo L, Donzelli G, Minetti C, Paravati F, Di Mauro G, Festini F, Esposito S, Corsello G. Inter-society consensus document on treatment and prevention of bronchiolitis in newborns and infants. Ital J Pediatr 40:65
Garcia-Maurino C, Brenes-Chacón H, Halabi KC, Sánchez PJ, Ramilo O, Mejias A (2023) Trends in Age and Disease Severity in Children Hospitalized With RSV Infection Before and During the COVID-19 Pandemic. JAMA Pediatr e235431. Epub ahead of print
Hasegawa K, Pate BM, Mansbach JM, Macias CG, Fisher ES, Piedra PA, Espinola JA, Sullivan AF, Camargo CA Jr (2015) Risk factors for requiring intensive care among children admitted to ward with bronchiolitis. Acad Pediatr 15:77–81
Manti S, Staiano A, Orfeo L et al (2023) UPDATE - 2022 Italian guidelines on the management of bronchiolitis in infants. Ital J Pediatr 49:19
Solarino B, Aricò M (2020) Covid-19 pandemic and pediatric healthcare policy in Italy: time for a change. Pediatr Rep 12:8823
Zimmermann P, Pittet LF, Finn A, Pollard AJ, Curtis N (2022) Should children be vaccinated against COVID-19? Arch Dis Child 107:e1
Cozzi G, Sovtic A, Garelli D et al (2023) SARS-CoV-2-related bronchiolitis: a multicentre international study. Arch Dis Child 108:e15
Acknowledgements
None.
IRIDE study group
Roberta Barachetti, Ospedale Sant’Anna di Como, Como, Italy; Claudia Pagliotta, Ospedale Sant’Anna di Como, Como, Italy; Silvia Gulden, Ospedale Sant’Anna di Como, Como, Italy; Francesco Maria Risso, Neonatal intensive care unit, Ospedali Civili di Brescia, Brescia, Italy; Michael Colpani, Neonatal intensive care unit, Ospedali Civili di Brescia, Brescia, Italy; Salvatore Aversa, Neonatal intensive care unit, Ospedali Civili di Brescia, Brescia, Italy; Paolo Tagliabue, S.C. Neonatologia e Terapia Intensiva Neonatale, IRCCS Fondazione San Gerardo dei Tintori, Monza, Italy; Federico Cattaneo, S.C. Neonatologia e Terapia Intensiva Neonatale, IRCCS Fondazione San Gerardo dei Tintori, Monza, Italy; Roberta Corbetta, S.C. Neonatologia e Terapia Intensiva Neonatale, IRCCS Fondazione San Gerardo dei Tintori, Monza, Italy; Maria Luisa Ventura, S.C. Neonatologia e Terapia Intensiva Neonatale, IRCCS Fondazione San Gerardo dei Tintori, Monza, Italy; Stefano Ghirardello, S.C. Neonatologia e Terapia Intensiva Neonatale, Fondazione IRCCS Policlinico San Matteo, Pavia, Italy; Ilaria De Lucia, S.C. Neonatologia e Terapia Intensiva Neonatale, Fondazione IRCCS Policlinico San Matteo, Pavia, Italy; Francesca Garofoli, S.C. Neonatologia e Terapia Intensiva Neonatale, Fondazione IRCCS Policlinico San Matteo, Pavia, Italy; Luca Mancini, Pediatria, Asst Grande Ospedale Metropolitano Niguarda di Milano, Milan, Italy; Giulia Angela Carla Pattarino, Pediatria, Asst Grande Ospedale Metropolitano Niguarda di Milano, Milan, Italy; Costantino De Giacomo, Pediatria, Asst Grande Ospedale Metropolitano Niguarda di Milano, Milan, Italy; Salvatore Barberi, ASST Rhodense Rho and Garbagnate Milanese, Italy; Mario Vernich, ASST Rhodense Rho and Garbagnate Milanese, Italy; Elisabetta Veronelli, ASST Rhodense Rho and Garbagnate Milanese, Italy; Emanuela Brazzoduro, ASST Rhodense Rho and Garbagnate Milanese, Italy; Ilaria Bottino, ASST Brianza - Ospedale Pio XI Desio, Italy; Tiziana Varisco, ASST Brianza - Ospedale Pio XI Desio, Italy; Patrizia Calzi, ASST Brianza - Ospedale Pio XI Desio, Italy; Alessandro Porta, ASST Ovest Milanese, Ospedale Fornaroli di Magenta, Italy; Paola Alga, ASST Ovest Milanese, Ospedale Fornaroli di Magenta, Italy; Laura Cozzi, ASST Ovest Milanese, Ospedale Fornaroli di Magenta, Italy; Francesca Lizzoli, ASST Ovest Milanese, Ospedale Fornaroli di Magenta, Italy; Lorenzo D'Antiga, SS Pediatria Internistica, SC Pediatria generale, ASST Papa Giovanni XXIII, Bergamo, Italy; Angelo Mazza, SS Pediatria Internistica, SC Pediatria generale, ASST Papa Giovanni XXIII, Bergamo, Italy; Fabiana Di Stasio, SS Pediatria Internistica, SC Pediatria generale, ASST Papa Giovanni XXIII, Bergamo, Italy; Gian Luigi Marseglia, Pediatria, Fondazione IRCCS Policlinico San Matteo, Pavia, Italy, Italy; Mascolo Amelia, Pediatria, Fondazione IRCCS Policlinico San Matteo, Pavia, Italy, Italy; Matea Jankovic, Pediatria, Fondazione IRCCS Policlinico San Matteo, Pavia, Italy; Lidia Decembrino, ASST Pavia, Ospedale Civile di Vigevano, Italy; Dario Pantaleo, ASST Pavia, Ospedale Civile di Vigevano, Italy; Chiara Vimercati, UO Pediatria, Ospedale San Gerardo Di Monza, Italy; Martha Caterina Faraguna, UO Pediatria, Ospedale San Gerardo Di Monza, Italy; Francesca Cattaneo, UO Pediatria, Ospedale San Gerardo Di Monza, Italy; Irene Lepri, UO Pediatria, Ospedale San Gerardo Di Monza, Italy; Laura Pogliani, ASST OVEST MI Ospedale di Legnano; Liana Bevilacqua, ASST OVEST MI Ospedale di Legnano; Luca Bernardo, ASST FateBeneFratelli Macedonio Melloni - Presidio Ospedaliero Macedonio Melloni di Milano, Italy; Sergio Arrigoni, ASST FateBeneFratelli Macedonio Melloni - Presidio Ospedaliero Macedonio Melloni di Milano, Italy; Giuseppe Mercurio, ASST FateBeneFratelli Macedonio Melloni - Presidio Ospedaliero Macedonio Melloni di Milano, Italy; Costanza Paramithiotti, SC Pediatria, Presidio San Paolo, ASST Santipaolocarlo, Milan, Italy; Elisabetta Salvatici, SC Pediatria, Presidio San Paolo, ASST Santipaolocarlo, Milan, Italy; Giuseppe Banderali, SC Pediatria, Presidio San Paolo, ASST Santipaolocarlo, Milan, Italy; Alberto Fabio Podestà, ASST Santi Paolo Carlo, Ospedale San Carlo di Milano, Milan, Italy; Elisa Dusi, ASST Santi Paolo Carlo, Ospedale San Carlo di Milano, Milan, Italy; Teresa Vivaldo, ASST Santi Paolo Carlo, Ospedale San Carlo di Milano, Milan, Italy; Sonia Bianchini, ASST Santi Paolo Carlo, Ospedale San Carlo di Milano, Milan, Italy; Paolo Del Barba, IRCCS Ospedale San Raffaele, Milan, Italy; Graziano Barera, IRCCS Ospedale San Raffaele, Milan, Italy; Claudia Aracu, IRCCS Ospedale San Raffaele, Milan, Italy; Stefano Martinelli, S.C. Neonatologia e Terapia Intensiva Neonatale, ASST Grande Ospedale Metropolitano Niguarda di Milano, Milan, Italy; Alice Proto, S.C. Neonatologia e Terapia Intensiva Neonatale, ASST Grande Ospedale Metropolitano Niguarda di Milano, Milan, Italy; Marco Fossati, S.C. Neonatologia e Terapia Intensiva Neonatale, ASST Grande Ospedale Metropolitano Niguarda di Milano, Milan, Italy; Lorella Rossi, ASST Valtellina-Alto Lario, Presidio Ospedaliero Di Sondrio, Italy; Emilio Palumbo, ASST Valtellina-Alto Lario, Presidio Ospedaliero Di Sondrio, Italy; Marta Odoni, Gruppo San Donato, Policlinico Ponte San Pietro di San Pietro, Italy; Ilaria Dalla Verde, Gruppo San Donato, Policlinico Ponte San Pietro di San Pietro, Italy; Ahmad Kantar, Gruppo San Donato, Policlinico Ponte San Pietro di San Pietro, Italy; Paola Sindico, ASST Mantova, A. O. Istituti Ospitalieri Carlo Poma di Mantova, Mantua, Italy; Grazia Morandi, ASST Mantova, A. O. Istituti Ospitalieri Carlo Poma di Mantova, Mantua, Italy; Valeria Fasolato, ASST Mantova, A. O. Istituti Ospitalieri Carlo Poma di Mantova, Mantua, Italy; Germana Viscogliosi, Pediatria, Fondazione Poliambulanza Istituto Ospedaliero di Brescia, Italy; Nunzia Managanelli, Pediatria, Fondazione Poliambulanza Istituto Ospedaliero di Brescia, Italy; Giuseppe Riva, Pediatria, Fondazione Poliambulanza Istituto Ospedaliero di Brescia, Italy; Chryssoula Tzialla, ASST Pavia - Ospedale Civile di Voghera, Italy; Roberta Giacchero, ASST Lodi, Ospedale Maggiore di Lodi, Italy; Caterina Sabatini, ASST Lodi, Ospedale Maggiore di Lodi, Italy; Elena Rossi, ASST Lodi, Ospedale Maggiore di Lodi, Italy; Cesare Antonio Ghitti, ASST Bergamo Est - Ospedale Pesenti Fenaroli Di Alzano Lombardo, Italy; Ilaria Pacati, ASST Bergamo Est - Ospedale Pesenti Fenaroli Di Alzano Lombardo, Italy; Raffaele Badolato, ASST Degli Spedali Civili di Brescia, Brescia, Italy; Laura Dotta, ASST Degli Spedali Civili di Brescia, Brescia, Italy; Antonella Meini, ASST Degli Spedali Civili di Brescia, Brescia, Italy; Ilia Bresesti, ASST Settelaghi, Ospedale “F. Del Ponte”, Varese, Italy; Antonio Francone, ASST Settelaghi, Ospedale “F. Del Ponte”, Varese, Italy; Anna Maria Plebani, ASST Settelaghi, Ospedale “F. Del Ponte”, Varese, Italy; Massimo Agosti, ASST Settelaghi, Ospedale “F. Del Ponte”, Varese, Italy; Marco Sala, ASST della Brianza, Ospedale di Vimercate, Italy; Simona Santucci, ASST della Brianza, Ospedale di Vimercate, Italy; Chiara Cuzzupè, ASST della Brianza, Ospedale di Vimercate, Italy; Cristina Bellan, Terapia Intensiva Neonatale - ASST Bergamo Est Ospedale Bolognini Seriate Italy; Federica Pontiggia, Terapia Intensiva Neonatale - ASST Bergamo Est Ospedale Bolognini Seriate Italy;Alice Romero, Pediatric Department, "Vittore Buzzi" Children's Hospital, Università degli Studi di Milano, Milan, Italy; Chiara Perazzi, Pediatric Department, "Vittore Buzzi" Children's Hospital, Università degli Studi di Milano, Milan, Italy; Anna Banfi, Pediatric Department, "Vittore Buzzi" Children's Hospital, Università degli Studi di Milano, Milan, Italy; Gianvincenzo Zuccotti, Pediatric Department, "Vittore Buzzi" Children's Hospital, Milan, Italy, Department of Biomedical and Clinical Sciences, Università degli Studi di Milano, Milan, Italy; Gianluca Lista, Division of Neonatology, "Vittore Buzzi" Children's Hospital, Milan, Italy
Funding
Open access funding provided by Università degli Studi di Milano within the CRUI-CARE Agreement. The study was partially supported by a grant of the Italian ministry of Health (Ricerca Corrente 2022).
Author information
Authors and Affiliations
Consortia
Contributions
GPM, AR, CA, PM, GC, NP, LP, FM developed the concept of the IRIDE study. AB, MC, RC, CP and the investigators of the IRIDE study group performed data extraction. GPM, AR, CA, PM, GC, NP, AB, MC, RC, CP and the investigators of the IRIDE study group participated in data extraction, verification and interpretation. NP was responsible for data cleaning and analyses. PM, FM supervised all aspects of the study. GPM wrote the first draft and all authors contributed to redrafting the manuscript. All authors critically reviewed the manuscript for important intellectual content. All authors approved the final manuscript as submitted.
Corresponding author
Ethics declarations
Disclaimer
The funding agencies had no role in study design, data collection, analysis or interpretation, or writing of the report.
Ethics approval
The study was approved by the Ethical committee of Milan Area2 and was conducted in accordance with the Declaration of Helsinki.
Consent to participate
Not required for this study.
Consent for publication
All authors gave their consent for publication. No further consent is required.
Conflicts of interest
The authors declare no competing interests.
Additional information
Communicated by Daniele De Luca
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Milani, G.P., Ronchi, A., Agostoni, C. et al. Long-lasting effects of COVID-19 pandemic on hospitalizations and severity of bronchiolitis. Eur J Pediatr 183, 1751–1758 (2024). https://doi.org/10.1007/s00431-023-05395-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-023-05395-1