Abstract
Fontan circulation is a highly abnormal circulatory state that may affect various organ systems. The effect on body composition is an important factor to assess the condition of the patient. This systematic review assesses body composition and possibly related adverse outcomes in patients with a Fontan circulation, to provide an overview of current insights. Studies evaluating body composition by compartment (either fat mass or lean/muscle mass) in Fontan patients published up to April 2023 were included in this systematic review. Of 1392 potential studies, 18 studies met the inclusion criteria. In total, body composition measurements of 774 Fontan patients were included. Body composition was measured using dual-energy X-ray absorptiometry (DXA) (n = 12), bioelectrical impedance analysis (BIA) (n = 5), computer tomography (CT) (n = 1), or magnetic resonance imaging (MRI) (n = 1). All studies reported a normal body mass index (BMI) in Fontan patients, compared to controls. Five out of nine studies reported significantly higher body fat values, and twelve out of fifteen studies reported significantly lower muscle or lean mass values in the Fontan population compared to the healthy population. Unfavorable body composition in Fontan patients was associated with decreased exercise capacity, worse cardiac function, and adverse outcomes including hospital admissions and death.
Conclusions: Despite having a normal BMI, Fontan patients have an increased fat mass and decreased muscle mass or lean mass compared to the healthy population. This unfavorable body composition was associated with various adverse outcomes, including a decreased exercise capacity and worse cardiac function.
What is Known: • Patients with a Fontan circulation have a decreased exercise capacity compared to healthy peers, an unfavorable body composition might be a contributor to their impaired exercise capacity. | |
What is New: • Fontan patients are predisposed to an unfavorable body composition, characterized by increased fat mass and decreased muscle mass accompanied by a normal BMI compared to the healthy population. • Among others, unfavorable body composition was associated with decreased exercise capacity, cardiac function, and increased morbidity in patients with a Fontan circulation. |
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The Fontan procedure is the preferred treatment strategy in children born with a functional univentricular heart, unsuitable for biventricular repair [1]. Although long-term survival after the Fontan procedure has been improving over the years, patients are still facing increased morbidity and mortality over time [2]. While infancy patients with a single ventricle experience growth impairment, adult Fontan patients show high rates of overweight and obesity [3, 4]. Adiposity is often expressed as body mass index (BMI) [3]. However, when BMI is used as a surrogate of adiposity, it does not take into account the patient’s body fat versus muscle mass. Therefore, the combination of reduced muscle mass and increased body fat may result in “normal” BMI and thereby conceal the presence of increased adiposity [5]. A more accurate way to approximate body composition is by compartment: fat free mass (consisting out of lean mass and bones) and fat mass. As total body lean mass still includes organs (which could be enlarged in Fontan patients), leg lean mass is most likely the best approximation for skeletal muscle, as most muscles are located in the legs. Several studies showed that estimating body composition by compartment by using dual-energy X-ray absorptiometry (DXA) is a better predictor of cardiovascular risk factors and all-cause mortality than just BMI [6,7,8]. Gaining more knowledge on the body composition of Fontan patients is important, as it might be a contributor to their impaired exercise capacity [9]. Having sufficient muscle mass might be especially important in patients with a Fontan circulation [10, 11]. In Fontan patients, the systemic venous return bypasses a subpulmonary ventricle and is directly connected to the pulmonary arteries [12]. Due to the absence of a subpulmonary ventricle to pump blood through the pulmonary vascular bed, cardiac filling is more dependent on the respiratory and peripheral muscle pumps [10]. To the best of our knowledge, no review regarding body composition in patients with a Fontan circulation exists in current literature. This systematic review is aimed at (1) assessing body composition by compartment in patients with a Fontan circulation and (2) investigating the prognostic value of (an unfavorable) body composition in this population.
Methods
Protocol registration and search strategy
This study was conducted according to the PRISMA guidelines [13]. A systematic search was performed in online databases on 13 April 2023. The search is presented in Supplement 1. The searched databases were Embase, Medline Ovid, Web of Science, and Cochrane CENTRAL. The search terms consisted of keywords related to Fontan circulation and body composition values. No filters were applied.
Inclusion and exclusion criteria
All studies were screened on title and abstract by two independent reviewers (JNP and RJB). Studies were included when they described body composition measurements by compartment in patients with a Fontan circulation. The full text of relevant articles was assessed for inclusion in the systematic review. The exclusion criteria were as follows: (a) studies without patients with a Fontan circulation, (b) body composition values of interest (body fat percentage, fat mass (index), lean mass (index), appendicular lean mass (index), or leg lean mass (index)) were not mentioned, (c) body composition values not specifically matched to patients with a Fontan circulation, and (d) results from conference papers and abstracts without a full text available. Discrepancies between the reviewers were discussed and resolved together with a third reviewer (LES).
Data extraction
From the resulting articles, two reviewers (JNP and RJB) extracted all data needed independently using Excel (version 2019). The extracted data from each reviewer was verified by the extracted data from the other reviewer; any discrepancies were discussed together with a third author (LES). The following data were extracted: study characteristics—journal, year of publication, study design, study size (of the patient group and, if present, of the control group), time frame of inclusion, and location or database; patient characteristics—age, age at Fontan completion, sex, Fontan type, ventricle type, and the method used to compare the body composition of the patients with a Fontan circulation (control group or pre-existing reference values); methodology used for measuring the body composition; measurement outcomes—body mass index (BMI), body fat percentage, appendicular lean mass (index), leg lean mass (index), fat mass (index), and lean mass (index); conclusions of studies related to the relationship between body composition and (adverse) outcomes (such as re-interventions and cardiac failure); and conclusions related to the body composition measurements. Studies were divided into groups and summarized based on the age of the study population—adults only, children only, and both adults and children.
Quality assessment appraisal
The Strengthening Reporting of Observational Studies in Epidemiology (STROBE) checklist was used to assess the quality of cohort and cross-sectional studies [14].
Results
Included studies
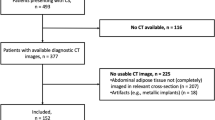
A total of 1392 studies were identified through the search. After removing duplicates and screening on title and abstract, the full text of 29 articles was screened. A total of 18 studies were included in this systematic review [5, 15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31]. This process is presented in Fig. 1.
Quality appraisal
None of the studies were excluded based on quality. All studies met over 75% of the STROBE checklist criteria. The quality assessment is presented in Supplement 2.
Study and patient characteristics
The study designs of all included studies are described in Table 1, and patient characteristics in Table 2. In total, body composition was measured in 774 patients with a Fontan circulation, and 298 healthy participants served as controls. Five studies included children only [15, 16, 24, 27, 28], five studies included adults only [5, 17, 18, 25, 32], and eight studies included both children and adults [19,20,21,22,23, 26, 30, 31]. The mean age of the patients between studies ranged from 1.5 to 30 years; 45.0% of the participants was female. The mean age at Fontan completion was 4.44 years. The percentage of a dominant left ventricle was 52.6%, and the percentage of patients with an open fenestration was 49.8%.
Measurement methods
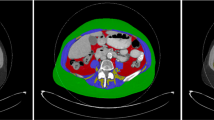
The measurement methods are summarized in Table 1. Twelve studies assessed the body composition using dual-energy X-ray absorptiometry (DXA) [5, 15, 16, 18,19,20,21,22, 27, 28, 30,31,32]. Five studies estimated the body composition using bioelectrical impedance analysis (BIA) [17, 23, 25, 28, 32]. One study assessed the body composition using peripheral quantitative computed tomography (CT) taken at a specific location on the left tibia, corresponding to 66% site of its total length [24]. One study assessed the body composition using liver or abdominal magnetic resonance (MR) at levels thoracic vertebrae 12 (T12) and lumbar vertebrae 3 (L3) [26]. Seven studies recruited control patients [15, 16, 18, 23,24,25, 30]. Nine studies used reference values to compare their patient group [5, 19,20,21,22, 24, 27, 31]. Two studies did not compare the body composition with control patients or reference values [17, 32]. Eight out of eighteen studies [5, 18,19,20,21, 23, 27] used Z-scores. The studies indexed their results on sex and age [5, 18, 19], sex, age, race, height, BMI, and leg-length [20,21,22, 27] or did not mention how they normalized their results [23].
Body composition
Out of the 18 included studies, 17 calculated the BMI of Fontan patients and controls or reference values [5, 15, 16, 18,19,20,21,22,23,24,25,26,27,28, 30,31,32]. These outcomes are documented in Table 3. Nine studies measured fat mass in patients with a Fontan circulation [5, 15, 17, 19, 21, 23, 25, 30, 32], and 15 measured lean/muscle mass in patients with a Fontan circulation [5, 15, 16, 18,19,20,21,22,23,24,25,26,27,28, 31]. Outcomes regarding fat, lean, and muscle mass can also be found in Table 3. All measurement outcomes are summarized in Table 4. Measured BMI was within normal range and not significantly different from control patients or reference values in fifteen out of seventeen studies [5, 15, 16, 18,19,20,21,22,23,24,25,26,27,28, 30,31,32]. Five out of nine studies concluded that patients with a Fontan circulation had a higher fat mass [5, 15, 19, 23, 31]. Four studies concluded that Fontan patients had a comparable lean/muscle mass to controls/reference values [16, 24, 26, 30]. Twelve out of fifteen studies concluded that patients with a Fontan circulation had a reduced (skeletal) muscle mass and/or lower lean mass [5, 15, 18,19,20,21,22,23, 25,26,27, 31].
Correlations between body composition and (adverse) outcomes
Five studies investigated associations between body composition and cardiac function [5, 19, 20, 23, 25]. Tran et al. showed that the degree of muscle deficit is associated with ventricular systolic impairment [5]. This corresponds to the findings of the other four studies. A higher leg lean mass was associated with larger increases of cardiac index and indexed systemic flow during exercise [20]. Higher body fat was associated with poorer New York Heart Association class (III or IV) in study of Shiina et al. [25]. Also, various Fontan complications including cardiac failure (New York Heart Association class III/IV), protein-losing enteropathy, plastic bronchitis, heart transplant, and death were associated with increased adiposity and/or lower muscle mass in the studies of Cao et al. and Powell et al. [19, 23]. Cao et al. demonstrated that every 1% increase in body fat percentage was associated with a 10% increased risk of reaching a Fontan complication. In total, eight studies investigated the relation between body composition and exercise capacity [5, 17, 18, 20, 23, 26]. Higher muscle mass was correlated with higher exercise capacity (Peak VO2) in three studies; higher leg lean mass showed the same association [5, 18, 23, 26]. Avitabile et al. found a correlation between skeletal muscle deficits and a reduced exercise capacity [20]. Patients with an improving exercise capacity over time had a lower body fat percentage compared to patients with a Fontan circulation that diminished in exercise capacity over time [17]. Lastly, Vaikunth et al. also showed that lower leg lean mass was associated with a lower whole body bone mass density [22]. Two studies investigated the effect of exercise training on (leg) lean muscle mass, both showing no change [27, 29].
Discussion
This is the first systematic review to assess the body composition in patients with a Fontan circulation. Overall, studies examining body composition in patients with a Fontan circulation were scarce. A total of 18 studies including 774 patients with a Fontan circulation met the inclusion criteria. All studies reported normal BMI, in contrast to body composition outcomes. The majority of the studies reported a decreased measured muscle mass and increased fat mass in patients with a Fontan circulation. Multiple studies looked at the relationship between body composition and adverse outcomes, showing that an unfavorable body composition in patients with a Fontan circulation was associated with impaired cardiac function, decreased exercise capacity and increased amount of Fontan complications.
Body composition measurement methods
The findings of this systematic review are heterogeneous. Reviewed studies included both children and adults, and different techniques were used to measure body composition. Most studies used DXA or BIA to measure the body composition. The use of DXA to measure different body compartments has been described and validated against the gold standard (whole-body potassium counting) in multiple clinical studies, showing comparable outcomes [34]. As DXA scans are easier, cheaper, and less stressful compared to whole-body potassium counting for the patient, DXA is the recommended measuring methods for assessing body composition in both research and clinical setting [34]. However, the use of DXA is limited to the research/ clinical context due to equipment cost, exposure to radiation (although very low), and lack of portability [35]. BIA has been proven to be one of the most practical methods to estimate body composition, as costs are low, its quick assessment procedures, and accessibility [36]. However, measurements obtained with BIA are less accurate and influenced by sex, ethnicity, weight, and age [37]. Also, diseases which change serum electrolytes, blood flow, and fluid distribution affect the accuracy of BIA measurements, ultimately making BIA less accurate for Fontan patients [37]. MRI and CT were used in only two studies [23, 24]. MRI and CT can measure both whole-body composition and body composition of a certain area. A study from Kullberg et al. showed strong correlations between MRI, CT, and DXA; however, both MRI and CT have major disadvantages [38]. MRI measurements might be highly dependent on used scanning protocols and are very expensive and time-consuming. Although CT is much faster, exposure to radiation is high; in addition, both techniques are very costly. Surprisingly, our systematic review did not find any reporting on the use of air-displacement plethysmography or skinfold measurements in patients with a Fontan circulation.
Body composition outcomes
As mentioned earlier, BMI is the most commonly used measurement to define adiposity [39]. However, BMI can be misleading as a combination of reduced lean mass and increased adiposity can result in a “normal” BMI, as was confirmed by this systematic review. In most included studies, patients with a Fontan circulation had an unfavorable body composition profile characterized by reduced skeletal muscle mass and increased adiposity, despite a normal BMI. The only two studies reporting normal muscle mass compared to the healthy population were performed in children. These findings may have important diagnostic and prognostic implications. In the general population, an unfavorable body composition is associated with various morbidities, including diabetes, cardiovascular disease, cancer, and early death [40,41,42]. Studies included in this systematic review also found an association between unfavorable body composition in Fontan patients and adverse outcomes, including cardiac failure [19, 23]. This is particularly relevant since several studies have shown the importance of the skeletal muscle pump to increase venous return during exercise [18, 20]. The study by Avitabile et al. showed that having a higher leg lean mass was associated with increases in cardiac index during exercise, suggesting that Fontan patients with higher leg lean mass may indeed be better able to augment systemic output during exercise [20]. In addition, all studies investigating the association between (leg) lean mass and exercise capacity included in this systematic review found that a reduced lean mass was associated with worse exercise capacity [5, 18, 23, 26]. While this may be intuitive, these findings stress the importance of maintaining and improving muscle mass in these patients. Causes of muscle mass deficits are poorly defined in patients with a Fontan circulation. Relative deconditioning, chronically elevated central venous pressure, decreased physical activity levels and neurohormonal activation, and malnutrition might be contributing factors [43,44,45]. As prospective studies are currently lacking, the question also remains whether worse Fontan outcomes are caused by less physical activity leading to an unfavorable body composition, or the other way around. A way to improve body composition in the healthy population is by performing moderate to vigorous physical activity [46, 47]. Exercise in patients with a Fontan circulation has been shown to improve exercise capacity, cardiac function and quality of life [9]. While there are few existing data supporting any particular approach, establishing a healthy lifestyle in Fontan patients, is likely to have a substantive positive impact. Recent studies from both Avitabile et al. and Chemello et al. measured body composition respectively before and after lower leg-focused muscle exercise and an 6-month lasting exercise intervention; both studies did not find a significant change [27, 29].
Limitations
Several limitations of the studies included have to be discussed. Patient characteristics were not always reported in detail, and information regarding physical activity levels of the included patients was lacking. The majority of the studies did not include a healthy control group but compared the body composition outcomes of the patients to reference values. Information regarding the exact origin of these reference values and methods used to index mass was often lacking, some studies did not correct their results for height at all which is especially important in studies including children. Some results were indexed very well by certain notable exceptions [20,21,22, 27]. Two studies did not compare body composition outcomes to their healthy population, making it hard to draw definite conclusions from their data [17, 28]. Body composition outcomes of children and adults (in the mixed studies) and males/females were not reported separately; also cohorts were homogeneous. We could not rule out overlap of patients between studies for all studies included in our review. Hansson et al. and Sandberg et al. included patients from the Northern part of Sweden and Stockholm [15, 16]. The patient group of four studies consisted of patients from the Children’s Hospital of Philadelphia [20,21,22, 27]. Three studies used the same registry to collect patient data [5, 19, 31]. Lastly, there was a high inter-study variability for measured outcomes; studies reported raw values, indexed values for height squared, or Z-scores, making absolute values hard to compare.
Future and clinical applications
Future studies should be prospective to not only demonstrate associations but also investigate causes and include homogenous cohorts to minimalize confounders. Patients should be followed longitudinally, as this can provide a better insight into the development of the body composition over time and its role as a predictor for an adverse event. Importantly, means to improve the unfavorable body composition in patients with a Fontan circulation should be explored further.
Conclusions
This systematic review shows that Fontan patients are predisposed to an unfavorable body composition, characterized by increased fat mass and decreased muscle mass accompanied by a normal BMI compared to the healthy population. Among others, unfavorable body composition was associated with decreased exercise capacity, cardiac function, and increased morbidity in patients with a Fontan circulation. Clinical awareness and appropriate management, including motivating patients with a Fontan circulation to maintain a healthy lifestyle, might lead to improved clinical outcomes.
Data availability
The data underlying this article will be shared on reasonable request to the corresponding author.
References
Fontan F, Baudet E (1971) Surgical repair of tricuspid atresia. Thorax 26(3):240–248
Dennis M, Zannino D, du Plessis K, Bullock A, Disney PJS, Radford DJ et al (2018) Clinical outcomes in adolescents and adults after the Fontan procedure. J Am Coll Cardiol 71(9):1009–1017
Payne E, Garden F, d’Udekem Y, McCallum Z, Wightman H, Zannino D et al (2022) Body mass index trajectory and outcome post Fontan procedure. J Am Heart Assoc 11(18):e025931
Andonian C, Langer F, Beckmann J, Bischoff G, Ewert P, Freilinger S et al (2019) Overweight and obesity: an emerging problem in patients with congenital heart disease. Cardiovasc Diagn Ther 9(Suppl 2):S360–S368
Tran D, D’Ambrosio P, Verrall CE, Attard C, Briody J, D’Souza M et al (2020) Body composition in young adults living with a Fontan circulation: the myopenic profile. J Am Heart Assoc 9(8):e015639
Sheibani H, Saberi-Karimian M, Esmaily H, Mouhebati M, Azarpazhooh MR, Divbands G et al (2020) A comparison of body mass index and body fat percentage for predicting cardiovascular disease risk. Translational Metabolic Syndrome Research 3:29–34
Benton MJ, Silva-Smith AL (2018) Accuracy of body mass index versus lean mass index for prediction of sarcopenia in older women. J Frailty Aging 7(2):104–107
Atkins JL, Whincup PH, Morris RW, Lennon LT, Papacosta O, Wannamethee SG (2014) Sarcopenic obesity and risk of cardiovascular disease and mortality: a population-based cohort study of older men. J Am Geriatr Soc 62(2):253–260
Scheffers LE, Berg LEMv, Ismailova G, Dulfer K, Takkenberg JJM, Helbing WA (2020) Physical exercise training in patients with a Fontan circulation: a systematic review. Eur J Prevent Cardiol 2047487320942869
Hjortdal VE, Emmertsen K, Stenbog E, Frund T, Schmidt MR, Kromann O et al (2003) Effects of exercise and respiration on blood flow in total cavopulmonary connection: a real-time magnetic resonance flow study. Circulation 108(10):1227–1231
Cordina R, Celermajer DS, D’Udekem Y (2018) Lower limb exercise generates pulsatile flow into the pulmonary vascular bed in the setting of the Fontan circulation. Cardiol Young 28(5):732–733
van der Ven JPG, van den Bosch E, Bogers A, Helbing WA (2018) State of the art of the Fontan strategy for treatment of univentricular heart disease. F1000Res 7
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP et al (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ 339:b2700
von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP et al (2008) The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol 61(4):344–349
Hansson L, Sandberg C, Öhlund I, Lind T, Sthen Bergdahl M, Wiklund U et al (2021) Vitamin D, liver-related biomarkers, and distribution of fat and lean mass in young patients with Fontan circulation. Cardiol Young
Sandberg C, Frisk E, Hansson L, Isberg A, Rylander Hedlund E, Sjöberg G et al (2020) Impaired knee extension muscle strength in adolescents but not in children with Fontan circulation. Cardiol Young 30(8):1138–1143
Ohuchi H, Negishi J, Miike H, Toyoshima Y, Morimoto H, Fukuyama M et al (2019) Positive pediatric exercise capacity trajectory predicts better adult Fontan physiology rationale for early establishment of exercise habits. Int J Cardiol 274:80–87
Cordina R, O’Meagher S, Gould H, Rae C, Kemp G, Pasco JA et al (2013) Skeletal muscle abnormalities and exercise capacity in adults with a Fontan circulation. Heart 99(20):1530–1534
Cao JY, Tran D, Briody J, Attard C, Hassan EB, Simm P et al (2021) Impact of adiposity on clinical outcomes in people living with a Fontan circulation. Int J Cardiol 329:82–88
Avitabile CM, Goldberg DJ, Leonard MB, Wei ZA, Tang E, Paridon SM et al (2018) Leg lean mass correlates with exercise systemic output in young Fontan patients. Heart 104(8):680–684
Avitabile CM, Leonard MB, Zemel BS, Brodsky JL, Lee D, Dodds K et al (2014) Lean mass deficits, vitamin D status and exercise capacity in children and young adults after Fontan palliation. Heart
Vaikunth SS, Leonard MB, Whitehead KK, Goldberg DJ, Rychik J, Zemel BS et al (2021) Deficits in the functional muscle–bone unit in youths with Fontan physiology. J Pediatr
Powell AW, Wittekind SG, Alsaied T, Lubert AM, Chin C, Veldtman GR et al (2020) Body composition and exercise performance in youth with a fontan circulation: a bio-impedance based study. J Am Heart Assoc 9(24)
Sarafoglou K, Petryk A, Mishra PE, Polgreen LE, Panoskaltsis-Mortari A, Brown R et al (2020) Early characteristics of bone deficits in children with Fontan palliation. Cardiol Young
Shiina Y, Murakami T, Matsumoto N, Okamura D, Takahashi Y, Nishihata Y et al (2018) Body composition, appetite-related hormones, adipocytokines, and heart failure in adult patients with congenital heart disease: a preliminary study. Congenit Heart Dis 13(1):79–84
Possner M, Alsaied T, Siddiqui S, Morales D, Trout AT, Veldtman G (2020) Abdominal skeletal muscle index as a potential novel biomarker in adult Fontan patients. CJC Open 2(2):55–61
Avitabile CM, McBride MG, Zhang X, Ampah S, Goldstein BH, Alsaied T et al (2022) Peak work rate increases with lower extremity-focused exercise training in adolescents with Fontan circulation. J Am Heart Assoc 11(24)
Pyykkönen H, Rahkonen O, Ratia N, Lähteenmäki S, Tikkanen H, Piirilä P et al (2022) Exercise prescription enhances maximal oxygen uptake and anaerobic threshold in young single ventricle patients with Fontan circulation. Pediatr Cardiol 43(5):969–976
Chemello L, Padalino M, Zanon C, Benvegnu L, Biffanti R, Mancuso D et al (2021) Role of transient elastography to stage Fontan-associated liver disease (FALD) in adults with single ventricle congenital heart disease correction. J Cardiovasc Dev Dis 8(10)
Tekerlek H, Saglam M, Kucukdagli AC, Aykan HH, Vardar-Yagli N, Calik-Kutukcu E et al (2023) Assessment of exercise capacity using field walking tests in patients after the Fontan procedure: a case–control study. Heart Lung 60:66–73
Wadey CA, Barker AR, Stuart G, Tran DL, Laohachai K, Ayer J et al (2022) Scaling peak oxygen consumption for body size and composition in people with a Fontan circulation. J Am Heart Assoc 11(24)
Chemello L, Padalino M, Zanon C, Benvegnu’ L, Biffanti R, Mancuso D et al (2021) Role of transient elastography to stage fontan-associated liver disease (Fald) in adults with single ventricle congenital heart disease correction. J Cardiovasc Dev Dis 8(10)
Tran D, D’Ambrosio P, Verrall C, Attard C, Briody J, D’Souza M et al (2019) Body composition abnormalities in adults with a Fontan circulation. Heart Lung Circul 28:S148–S149
Branski LK, Norbury WB, Herndon DN, Chinkes DL, Cochran A, Suman O et al (2010) Measurement of body composition in burned children: is there a gold standard? JPEN J Parenter Enteral Nutr 34(1):55–63
Shepherd JA, Ng BK, Sommer MJ, Heymsfield SB (2017) Body composition by DXA. Bone 104:101–105
Sun G, French CR, Martin GR, Younghusband B, Green RC, Xie YG et al (2005) Comparison of multifrequency bioelectrical impedance analysis with dual-energy X-ray absorptiometry for assessment of percentage body fat in a large, healthy population. Am J Clin Nutr 81(1):74–78
Dehghan M, Merchant AT (2008) Is bioelectrical impedance accurate for use in large epidemiological studies? Nutr J 7:26
Kullberg J, Brandberg J, Angelhed JE, Frimmel H, Bergelin E, Strid L et al (2009) Whole-body adipose tissue analysis: comparison of MRI, CT and dual energy X-ray absorptiometry. Br J Radiol 82(974):123–130
Bays HE, Toth PP, Kris-Etherton PM, Abate N, Aronne LJ, Brown WV et al (2013) Obesity, adiposity, and dyslipidemia: a consensus statement from the National Lipid Association. J Clin Lipidol 7(4):304–383
Peeters A, Barendregt JJ, Willekens F, Mackenbach JP, Al Mamun A, Bonneux L (2003) Obesity in adulthood and its consequences for life expectancy: a life-table analysis. Ann Intern Med 138(1):24–32
Bendor CD, Bardugo A, Pinhas-Hamiel O, Afek A, Twig G (2020) Cardiovascular morbidity, diabetes and cancer risk among children and adolescents with severe obesity. Cardiovasc diabetol 19(1):79
Larsson SC, Burgess S (2021) Causal role of high body mass index in multiple chronic diseases: a systematic review and meta-analysis of Mendelian randomization studies. BMC Med 19(1):320
Tran DL, Gibson H, Maiorana AJ, Verrall CE, Baker DW, Clode M et al (2021) Exercise intolerance, benefits, and prescription for people living with a Fontan circulation: the Fontan Fitness Intervention Trial (F-FIT)-rationale and design. Front Pediatr 9:799125
Ritmeester E, Veger VA, van der Ven JPG, van Tussenbroek G, van Capelle CI, Udink Ten Cate FEA et al (2022) Fontan circulation associated organ abnormalities beyond the heart, lungs, liver, and gut: a systematic review. Front Cardiovasc Med 9:826096
Baldini L, Librandi K, D'Eusebio C, Lezo A (2022) Nutritional management of patients with Fontan circulation: a potential for improved outcomes from birth to adulthood. Nutrients 14(19)
Toth MJ, Beckett T, Poehlman ET (1999) Physical activity and the progressive change in body composition with aging: current evidence and research issues. Med Sci Sports Exerc 31(11 Suppl):S590–S596
Zanovec M, Lakkakula AP, Johnson LG, Turri G (2009) Physical activity is associated with percent body fat and body composition but not body mass index in White and Black college students. Int J Exerc Sci 2(3):175–185
Acknowledgements
The authors wish to thank Sabrina Meertens-Gunput from the Erasmus MC Medical Library for her assistance with the literature search.
Author information
Authors and Affiliations
Contributions
RJB, JP, LES, and WAH had the main role in research protocol design. RJB and JP did the literature search, performed title, and abstract screening and data extraction. LES had the main role in drafting the manuscript. LEB and WAH contributed to interpretation. All authors (RJB, JP, LES, LEB, and WAH) critically revised the manuscript and approved the final version. The corresponding author attests that all listed authors meet authorship and that no others meeting the criteria have been omitted.
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare no competing interests.
Additional information
Communicated by Piet Leroy
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
van den Berg, R.J., Pos, J.N., Scheffers, L.E. et al. Body composition in patients with Fontan physiology: a systematic review. Eur J Pediatr 182, 4309–4321 (2023). https://doi.org/10.1007/s00431-023-05100-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-023-05100-2