Abstract
Faster resolution of hypoxaemic or hyperoxaemic events in preterm infants may reduce long-term neurodevelopmental impairment. Automatic titration of inspiratory oxygen increases time within the oxygen saturation target range and may provide a more prompt response to hypoxic and hyperoxic events. We assessed routinely performed follow-up at 2 years of age after the implementation of automated oxygen control (AOC) as standard care and compared this with a historical cohort. Neurodevelopmental outcomes at 2 years of age were compared for infants born at 24–29 weeks gestational age before (2012–2015) and after (2015–2018) the implementation of AOC as standard of care. The primary outcome was a composite outcome of either mortality or severe neurodevelopmental impairment (NDI), and other outcomes assessed were mild-moderate NDI, Bayley-III composite scores, cerebral palsy GMFCS, and CBCL problem behaviour scores. A total of 289 infants were included in the pre-AOC epoch and 292 in the post-AOC epoch. Baseline characteristics were not significantly different. Fifty-one infants were lost to follow-up (pre-AOC 6.9% (20/289), post-implementation 10.6% (31/292). The composite outcome of mortality or severe NDI was observed in 17.9% pre-AOC (41/229) vs. 24.0% (47/196) post-AOC (p = 0.12). No significant differences were found for the secondary outcomes such as mild-moderate NDI, Bayley-III composite scores, cerebral palsy GMFCS, and problem behaviour scores, with the exception of parent-reported readmissions until the moment of follow-up which was less frequent post-AOC than pre-AOC.
Conclusion: In this cohort study, the implementation of automated oxygen control in our NICU as standard of care for preterm infants led to no statistically significant difference in neurodevelopmental outcome at 2 years of age.
What is Known: • Neurodevelopmental outcome is linked to hypoxemia, hyperoxaemia and choice of SpO2 target range. • Automated titration of inspired oxygen may provide a faster resolution of hypoxaemic and hyperoxaemic events. | |
What is New: • This cohort study did not find a significant difference in neurodevelopmental outcome at two years of age after implementing automated oxygen control as standard of care. |
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Maintaining appropriate oxygenation in preterm infants admitted to the neonatal intensive care unit (NICU) has proved challenging but of importance to outcome. Neonatal morbidity and mortality are linked to hypoxemia, hyperoxaemia, and choice of SpO2 target range [1,2,3]. Post hoc analysis of the Canadian Oxygen Trial data associated adverse neurodevelopmental outcome with hypoxia, in particular hypoxic episodes lasting more than 1 min [4]. Hunt et al. reported similar evidence in their report of home-monitored preterm and term infants: Having five or more apneic/bradycardic events was associated with a 5.6-point lower mental development index [5]. Neither study showed a significant difference for episodes under 1 min. These results could indicate that faster resolution of hypoxaemic or hyperoxaemic events may reduce long-term neurodevelopmental impairment (NDI).
Automatic titration of inspired oxygen (FiO2) can provide a more prompt response to these events than when titration is done manually by bedside staff. With the aim of keeping SpO2 in a specified target range, an automated oxygen controller (AOC) built into the respirator continually evaluates on the measured SpO2 and makes changes in FiO2 where necessary. Beside potential benefits to workload, it has been demonstrated that several commercially available controllers increase the time preterm infants spent within the target range while used for 2–24 h periods, and prolonged episodes of hypoxemia and hyperoxaemia are reduced [6,7,8,9,10,11,12,13]. This was also reflected in a study [14] done in our centre while using an AOC as standard of care. However, to date, evidence on clinically relevant neonatal outcome is scarce [15] and lacking altogether beyond the neonatal period.
In August 2015, AOC was implemented as standard of care in the NICU of the Leiden University Medical Center (LUMC). Recently, we reported the effect of this implementation on the clinical outcome of preterm infants during admission [15]. Implementation did not lead to a change in mortality or rate of retinopathy of prematurity (ROP), necrotising enterocolitis (NEC), intraventricular haemorrhage (IVH), periventricular leukomalacia (PVL), or bronchopulmonary dysplasia (BPD), but there was less invasive ventilation in the post-implementation cohort. Thus far, none of the studies comparing manual oxygen control with AOC have reported the effect on long-term neurodevelopmental outcome. We therefore aimed to compare the neurodevelopmental outcome of preterm infants born before and after the implementation of AOC as standard care with routinely performed 2-year follow-up assessment.
Materials and methods
Study design
A retrospective study was conducted in the NICU of the LUMC, a tertiary-level perinatal centre with annually around 100 intensive care admissions of infants born before 30 weeks of gestation. A statement of no objection (G19.075) for obtaining and publishing the anonymised data was provided by the ethical board of the LUMC.
Infants admitted to the NICU between May 1, 2012, and December 31, 2018, and born between 24 and 29 weeks and 6 days of gestation were included in the analysis. Infants were excluded from the study if they were admitted > 24 h after birth, required no invasive or non-invasive respiratory support during their admission, or had major congenital abnormalities.
The pre-implementation cohort included patients admitted between May 1, 2012, and June 17, 2015, that received FiO2 manually titrated by bedside staff according to local guidelines. The post-implementation cohort consisted of infants admitted from October 18, 2015, to December 2018, taking into consideration a washout period of 4 months.
Data collection
All data were obtained from our patient data management systems (Metavision; IMDsoft, Tel Aviv, Israel and HiX; ChipSoft, Amsterdam, The Netherlands). Infants were invited for follow-up at 24 months corrected age for assessment by a neonatologist, paediatric physiotherapist, and paediatric psychologist. Respectively, they were responsible for the general and neurological examination, the assessment of motor function, and the assessment of cognitive functioning. The primary outcome was a composite outcome of mortality or severe NDI. Secondary outcomes were as follows: mild to moderate NDI, early mortality (mortality until 1 month after corrected term age), late mortality (mortality between 1 month after corrected term age and 2-year follow-up), motor and cognitive development scores, visual impairment, hearing loss, cerebral palsy, behavioural functioning, and number of readmissions. Severe NDI was defined as at least one of the following: cerebral palsy (Gross Motor Function Classification System (GMFCS) [16] ≥ level 3), Bayley-III-NL cognitive or motor scores less than two standard deviations under the mean, severe bilateral visual impairment or blindness, and/or bilateral sensorineural hearing loss or deafness needing hearing aids or cochlear implants. Mild to moderate NDI was defined as cerebral palsy GMFCS level 1 or 2, Bayley-III-NL cognitive or motor scores below one standard deviation under the mean, and mild visual and/or hearing impairment. Motor and cognitive development were assessed using the Bayley Scales of Infant and Toddler Development Third Edition, Dutch version (Bayley-III-NL) [17, 18]. As the minimum cognitive composite score using the Bayley III is 55, children failing to achieve this were nominally assigned a score of 54. Bayley III floor motor composite score is 46; hence, children failing to achieve this were nominally assigned a score of 45 [19]. Visual impairment was classified as mild (needing treatment by an ophthalmologist or orthoptist), impaired vision with the ability to see, or blind. Hearing loss was defined as mild, neurosensory hearing loss, or deaf. Behavioural outcome was assessed using the Child Behavioural Checklist (CBCL 1.5–5 years) completed by parents [20]. A classification of level 3 or higher on the GFMCS was considered severe [16]. When data could not be collected from the patient data management systems, the Dutch Perinatal and Neonatal register (Landelijke Neonatale Registratie) or other follow-up centres (university hospitals, revalidation centres) were consulted to complement the data.
Oxygen titration
During almost the entire study period, the AVEA ventilator (Vyaire, Yorba Linda CA, USA) was used for respiratory support; after August 2015, this involved AOC by the CLiO2 (Closed Loop of inspired Oxygen) controller [8]. As of November 2018, newly born preterm infants were supported by the SLE6000 ventilator (SLE, London, UK) with the OxyGenie option for AOC [21]. Following recent European guidelines [22], in November 2014, we changed the SpO2 target range in our NICU from 85–95% to 90–95%.
Data analysis
Data are reported as mean (SD), median (range), or number (percentage) as appropriate, with standard tests for normality. Statistical comparison was executed using an independent t-test, a Mann–Whitney U test, and a chi-square or Fisher’s exact test as appropriate. Statistical analyses were performed using IBM SPSS Statistics for Windows, version 25 (IBM, Armonk, New York, USA). Two-sided P values of < 0.05 were considered statistically significant.
Results
Patient characteristics and neonatal period
In the period of 2012–2018, 588 infants were born in the LUMC or transferred to the NICU within 24 h after birth, 293 infants in the pre-implementation period (pre-AOC) versus 295 infants in the post-implementation cohort (post-AOC). There were no differences in baseline characteristics (Table 1). In the neonatal period, there were similar rates of IVH, PVL, and laser coagulation for ROP. More details on the neonatal period can be found in our previous study [15]. Three children were excluded from analysis due to major congenital abnormalities affecting neurodevelopment (2 pre-AOC, 1 post-AOC), and 4 were excluded because they moved to a different country (2 pre-AOC, 2 post-AOC), leaving 289 infants in the pre-AOC group and 292 infants in the post-AOC group. We were unable to obtain any follow-up data for 51 infants (pre-AOC 6.9% (20/289), post-implementation 10.6% (31/292), baseline characteristics Supplemental (Table 1–2).
Outcomes at 2-year follow-up
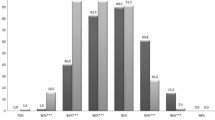
The composite primary outcome of mortality or severe NDI occurred in 17.9% (41/229; Table 2) before the implementation of AOC versus 24.0% (47/196) after implementation (p = 0.12). The majority was related to neonatal death (10.2% (30/289) vs. 10.8% (32/292) p = 0.82). After the neonatal period 0.4% (1/259) vs. 0.8% (2/259; p = 0.56), children died. Severe NDI was observed in 5.1% (10/198) before vs. 8.0% (13/162) after the implementation of AOC (p = 0.25). Mild to moderate NDI was detected in 38.5% (82/213) infants pre-AOC vs. 43.8% (78/178) after implementation (p = 0.29).
The median Bayley-III composite motor score was 97 (89–107) pre-AOC and 98 (89–109) post-AOC (p = 0.18). The composite cognitive score was 96 (87–101) vs. 96 (91–105) (p = 0.23). No significant differences were found in rates of scores between 1 and 2 SD under the mean (score 70–85) and below − 2 SD under the mean (score < 70), for motor nor cognitive. Motor scores, respectively, for pre- vs. post-implementation cohorts: 12.6% (25/199) of the children had scores between 1 and 2 SD under the mean and 2.5% (5/199) below − 2 SD vs. 12.8% (25/195, p = 0.94) and 5.6% (11/195, p = 0.12) after implementation. Cognitive scores in the pre-implementation group were found in 13.9% (31/232) between 1 and 2 SD under the mean and under 2 SD under the mean in 3.0% (7/232) vs. 12.7% (26/204, p = 0.85) and 3.4% (7/204, p = 0.81), respectively. We found no significant differences between groups in externalising (51 ± 10 vs. 50 ± 10, p = 0.69) or internalising (47 [41–55] vs. 47 [41–55], p = 0.59) problem behaviour scores.
Neurological examination, cerebral palsy GMFCS scores, visual impairment, and hearing loss yielded no significant differences. However, parents did report significantly fewer readmissions until the moment of follow-up in the post-AOC group (p = 0.002).
Discussion
This is the first study to report data on long-term neurodevelopmental follow-up at 2 years corrected age in very preterm infants treated with automated oxygen titration as standard of care compared with manual oxygen titration as standard of care. Implementation of automated oxygen titration did not lead to a change in mortality or neurodevelopmental outcome at 2 years. Although earlier studies [6,7,8,9,10,11,12,13,14] demonstrate an increase in time within the target range when using automated oxygen titration, we were not able to demonstrate an effect on neurodevelopmental outcome in this large cohort.
To date, there is little data on clinically relevant outcome of infants receiving automated oxygen titration. There is no data available on neurodevelopmental outcome after usage of AOC, and data on follow-up of preterm infants from non-AOC studies are difficult to compare with, because they involved non-standard interventions [23, 24], infants born almost 15 years ago [25, 26], or had a study population that had markedly different characteristics [27, 28]. The outcomes of both groups in our study are similar to the outcome of a previous cohort study from our centre [26].
The reason for fewer readmissions after the implementation of automated oxygen titration is not apparent from our data. Rates of BPD, ROP, and other morbidity potentially requiring re-hospitalisation are similar, although we did find fewer ventilation days in our previous study for the post-AOC cohort [29].
A failure to demonstrate an impact on neurodevelopmental outcome after implementing automated titration can have several causes. In the previous study on achieved target range time in our NICU, we demonstrated that although infants spent more time within the target range overall, this was mainly attributed to a reduction in time above the target range. In fact, using the CLiO2 controller led to a 6% increase of time spent under the SpO2 target range (90–95%). This increase was mainly just below the (85–90%) target range while still having a similar proportion of hypoxaemia (< 80%). If indeed more time spent under the target range is where neurodevelopmental improvement can be gained, the lack of improvement in this area could explain the lack of impact on neurodevelopmental outcome. Furthermore, as reported before, it could be that outcome is more largely influenced by the frequency and duration of hypoxia and hypoxic events [30], which were not investigated in our previous study nor in most other automated oxygen controller studies. Also, preterm infants can experience many potentially harmful stimuli and events before being tested at 2 years of corrected age, in particular during the neonatal phase. Oxygenation deviations during respiratory support may play only a minor role in the eventual neurodevelopmental outcome, meaning only very large randomised studies are able to demonstrate a statistically significant difference. Thirdly, neonatal care is a rapidly developing field with frequent changes to standard of care. Some of these unmeasured factors may influence the results in either direction. Finally, some of the adverse outcomes are relatively rare. If the effect of automated oxygen control is modest, a large clinical trial would be needed to observe an effect. Our study has a relatively modest convenience sample of 581 infants. Currently, the FiO2-C trial randomises between automated oxygen control or manual titration during the entire NICU stay and will investigate the effect on clinical and neurodevelopmental outcomes at 24 months of corrected age [29]. As their reported sample size is 2340 participants and because it is a prospective interventional study, it is better equipped to observe an effect. However, all commercially available devices are allowed, which may diminish the effect. The study is projected to run until December 2022.
A change in target range from 85–95% to 90–95% may influence the time spent in (mild) hypoxia. In our case, one would expect that the 76% (223/293) infants in the pre-implementation group born before November 2014 spent more time in the 85–90% range, as the lower limit was changed from 85 to 90%. The achieved proportion of time in the 85–90% range based on 1 min-values of the pre- and post-implementation data show no difference while infants received oxygen (pre-AOC 10.9 [8.6–13.5]%, post-AOC 10.4 [7.7–12.7]%, p = 0.09) and a 1.8% difference when considering the entire period of respiratory support (pre-AOC 5.5 [1.7–9.8]%, post-AOC 3.7 [1.6–7.6]%, p = 0.002; unpublished data). Van Zanten et al. reported before that the change of lower limit led to a reduction in achieved time within the 80–90% range in our unit, but time spent in hypoxia (SpO2 < 80%) was not different [31].
One of the inherent limitations of a retrospective design is the rate of missing data (loss to follow-up in this study: pre-AOC 6.9%, post-AOC 10.6%), which is unfortunately frequently high in follow-up research. The majority of missing children were transferred to another university NICU in the neonatal phase and had subsequent follow-up there; therefore, we expect them to be missing at random and not related to neurodevelopmental outcome. However, children lost to follow-up may be under treatment in a special care facility and therefore not missing at random. Parents may be less inclined to present their child for follow-up when they already receive regular tests in such a facility. To limit biased results due to missing such children, we requested data for all children tested elsewhere. Another strength of the study is that we have a relatively large cohort in which we had few exclusion criteria, meaning the results are generalisable to other NICUs in a similar setting. Furthermore, children are tested by trained professionals as part of a standardized national follow-up programme, improving the repeatability and reliability of the assessment of neurodevelopmental outcome. There may be several confounders in the study which we have not been able to adjust for, such as the type of automated oxygen controller, gestational age, and bronchopulmonary dysplasia. Despite most data being collected prospectively during standard follow-up, minimising recall bias, missing values for one of the outcomes was still relatively common. This precludes us from adjusting for these confounders and is a limitation of this study.
Besides fewer parent-reported readmissions, no change in outcome occurred after the implementation of automated oxygen control. It is reassuring that outcomes did not deteriorate and that outcome of our follow-up is similar to earlier reported data. Our results show no signs children are affected negatively by using an automated oxygen controller, whereas there are benefits for staff workload.
Conclusion
In this cohort study, the implementation of automated oxygen control in our NICU as standard of care for preterm infants led to no significant difference in neurodevelopmental outcome at 2 years of age.
Data Availability
Data are available on reasonable request.
Abbreviations
- AOC:
-
Automated oxygen controller
- BPD:
-
Bronchopulmonary dysplasia
- BSID-III-NL:
-
Bayley Scales of Infant and Toddler Development-Third Edition – NL
- CBCL:
-
Child Behaviour Checklist
- FiO2 :
-
Fraction of inspiratory oxygen
- GMFCS:
-
Gross Motor Function Classification System
- IVH:
-
Intraventricular haemorrhage
- NDI:
-
Neurodevelopmental impairment
- NEC:
-
Necrotising enterocolitis
- NICU:
-
Neonatal intensive care unit
- PVL:
-
Periventricular leukomalacia
- ROP:
-
Retinopathy of prematurity
- SpO2 :
-
Oxygen saturation measured by pulse-oximetry
References
Askie LM, Darlow BA, Finer N, Schmidt B, Stenson B, Tarnow-Mordi W, Davis PG, Carlo WA, Brocklehurst P, Davies LC, Das A, Rich W, Gantz MG, Roberts RS, Whyte RK, Costantini L, Poets C, Asztalos E, Battin M, Halliday HL, Marlow N, Tin W, King A, Juszczak E, Morley CJ, Doyle LW, Gebski V, Hunter KE, Simes RJ (2018) Association between oxygen saturation targeting and death or disability in extremely preterm infants in the neonatal oxygenation prospective meta-analysis collaboration. JAMA 319(21):2190–2201. https://doi.org/10.1001/jama.2018.5725
Di Fiore JM, Bloom JN, Orge F, Schutt A, Schluchter M, Cheruvu VK, Walsh M, Finer N, Martin RJ (2010) A higher incidence of intermittent hypoxemic episodes is associated with severe retinopathy of prematurity. J Pediatr 157(1):69–73. https://doi.org/10.1016/j.jpeds.2010.01.046
Imanishi Y, Hirata K, Nozaki M, Mochizuki N, Hirano S, Fukushima Y, Hatsukawa Y, Wada K (2020) Effect of fluctuation of oxygenation on the development of severe retinopathy of prematurity in extremely preterm infants. J Perinatol 40(3):515–521. https://doi.org/10.1038/s41372-019-0571-y
Poets CF, Roberts RS, Schmidt B, Whyte RK, Asztalos EV, Bader D, Bairam A, Moddemann D, Peliowski A, Rabi Y, Solimano A, Nelson H (2015) Association between intermittent hypoxemia or bradycardia and late death or disability in extremely preterm infants. JAMA 314(6):595–603. https://doi.org/10.1001/jama.2015.8841
Hunt CE, Corwin MJ, Baird T, Tinsley LR, Palmer P, Ramanathan R, Crowell DH, Schafer S, Martin RJ, Hufford D, Peucker M, Weese-Mayer DE, Silvestri JM, Neuman MR, Cantey-Kiser J (2004) Cardiorespiratory events detected by home memory monitoring and one-year neurodevelopmental outcome. J Pediatr 145(4):465–471. https://doi.org/10.1016/j.jpeds.2004.05.045
Claure N, Bancalari E, D’Ugard C, Nelin L, Stein M, Ramanathan R, Hernandez R, Donn SM, Becker M, Bachman T (2011) Multicenter crossover study of automated control of inspired oxygen in ventilated preterm infants. Pediatrics 127(1):e76-83. https://doi.org/10.1542/peds.2010-0939
Claure N, D'Ugard C, Bancalari E (2009) Automated adjustment of inspired oxygen in preterm infants with frequent fluctuations in oxygenation: a pilot clinical trial. J Pediatr 155(5):640–645 e641–642. https://doi.org/10.1016/j.jpeds.2009.04.057
Claure N, Gerhardt T, Everett R, Musante G, Herrera C, Bancalari E (2001) Closed-loop controlled inspired oxygen concentration for mechanically ventilated very low birth weight infants with frequent episodes of hypoxemia. Pediatrics 107(5):1120–1124. https://doi.org/10.1542/peds.107.5.1120
Van Kaam AH, Hummler HD, Wilinska M, Swietlinski J, Lal MK, te Pas AB, Lista G, Gupta S, Fajardo CA, Onland W, Waitz M, Warakomska M, Cavigioli F, Bancalari E, Claure N, Bachman TE (2015) Automated versus manual oxygen control with different saturation targets and modes of respiratory support in preterm infants. J pediatr 167(3):545–550 e541–542. https://doi.org/10.1016/j.jpeds.2015.06.012
Van Zanten HA, Kuypers KLAM, Stenson BJ, Bachman TE, Pauws SC, te Pas AB (2017) The effect of implementing an automated oxygen control on oxygen saturation in preterm infants. Arch Dis Child Fetal Neonatal Ed 102 (5):F395-F399. https://doi.org/10.1136/archdischild-2016-312172
Waitz M, Schmid MB, Fuchs H, Mendler MR, Dreyhaupt J, Hummler HD (2015) Effects of automated adjustment of the inspired oxygen on fluctuations of arterial and regional cerebral tissue oxygenation in preterm infants with frequent desaturations. J Pediatr 166(2):240–244 e241. https://doi.org/10.1016/j.jpeds.2014.10.007
Lal M, Tin W, Sinha S (2015) Automated control of inspired oxygen in ventilated preterm infants: crossover physiological study. Acta Paediatr 104(11):1084–1089. https://doi.org/10.1111/apa.13137
Plottier GK, Wheeler KI, Ali SK, Fathabadi OS, Jayakar R, Gale TJ, Dargaville PA (2017) Clinical evaluation of a novel adaptive algorithm for automated control of oxygen therapy in preterm infants on non-invasive respiratory support. Arch Dis Child Fetal Neonatal Ed 102(1):F37–F43. https://doi.org/10.1136/archdischild-2016-310647
Van Zanten HA, Kuypers K, Stenson BJ, Bachman TE, Pauws SC, Te Pas AB (2017) The effect of implementing an automated oxygen control on oxygen saturation in preterm infants. Arch Dis Child Fetal Neonatal Ed 102(5):F395–F399. https://doi.org/10.1136/archdischild-2016-312172
Salverda HH, Oldenburger NJ, Rijken M, Pauws SC, Dargaville PA, Te Pas AB (2021) The effect of automated oxygen control on clinical outcomes in preterm infants: a pre- and post-implementation cohort study. Eur J Pediatr 180(7):2107–2113. https://doi.org/10.1007/s00431-021-03982-8
Palisano R, Rosenbaum P, Walter S, Russell D, Wood E, Galuppi B (1997) Development and reliability of a system to classify gross motor function in children with cerebral palsy. Dev Med Child Neurol 39(4):214–223. https://doi.org/10.1111/j.1469-8749.1997.tb07414.x
Steenis LJP, Verhoeven M, Hessen DJ, van Baar AL (2015) Performance of Dutch children on the Bayley III: a comparison study of US and Dutch norms. PLoS ONE 10(8):e0132871. https://doi.org/10.1371/journal.pone.0132871
Bayley N (2009) Bayley-III: Bayley scales of infant and toddler development. Giunti OS
Van Baar A, Steenis L, Verhoeven M, Hessen DJ (2014) Bayley Scales of Infant and Toddler Development, technische handleiding BSID-III-NL. 3rd edition. Netherlands. Pearson Assessment
Achenbach T, Rescorla L (2000) Manual for the ASEBA Preschool forms & profiles. University of Vermont, Research Center for Children, Youth & Families, Burlington
Dargaville PA, Sadeghi Fathabadi O, Plottier GK, Lim K, Wheeler KI, Jayakar R, Gale TJ (2017) Development and preclinical testing of an adaptive algorithm for automated control of inspired oxygen in the preterm infant. Arch Dis Child Fetal Neonatal Ed 102(1):F31-f36. https://doi.org/10.1136/archdischild-2016-310650
Sweet DG, Carnielli V, Greisen G, Hallman M, Ozek E, Te Pas A, Plavka R, Roehr CC, Saugstad OD, Simeoni U, Speer CP, Vento M, Visser GHA, Halliday HL (2019) European consensus guidelines on the management of respiratory distress syndrome - 2019 update. Neonatology 115(4):432–450. https://doi.org/10.1159/000499361
Roelants JA, Vlaardingerbroek H, van den Akker CHP, de Jonge RCJ, van Goudoever JB, Vermeulen MJ (2018) Two-year follow-up of a randomized controlled nutrition intervention trial in very low-birth-weight infants. JPEN J Parenter Enteral Nutr 42(1):122–131. https://doi.org/10.1177/0148607116678196
van Klink JM, Slaghekke F, Balestriero MA, Scelsa B, Introvini P, Rustico M, Faiola S, Rijken M, Koopman HM, Middeldorp JM, Oepkes D, Lopriore E (2016) Neurodevelopmental outcome at 2 years in twin-twin transfusion syndrome survivors randomized for the Solomon trial. Am J Obstet Gynecol 214(1):113.e111-117. https://doi.org/10.1016/j.ajog.2015.08.033
de Waal CG, Weisglas-Kuperus N, van Goudoever JB, Walther FJ (2012) Mortality, neonatal morbidity and two year follow-up of extremely preterm infants born in the Netherlands in 2007. PLoS ONE 7(7):e41302. https://doi.org/10.1371/journal.pone.0041302
Jansen L, Peeters-Scholte C, van den Berg-Huysmans AA, van Klink JMM, Rijken M, van Egmond-van Dam JC, Vermeiren R, Steggerda SJ (2021) Longitudinal follow-up of children born preterm: neurodevelopment from 2 to 10 years of age. Front Pediatr 9:674221. https://doi.org/10.3389/fped.2021.674221
Lo J, McGinley JL, Fox LM, Spittle AJ (2015) Challenges of neurodevelopmental follow-up for extremely preterm infants at two years. Early Human Dev 91(12):689–694. https://doi.org/10.1016/j.earlhumdev.2015.09.012
Tollenaar LSA, Lopriore E, Slaghekke F, Oepkes D, Middeldorp JM, Haak MC, Klumper F, Tan R, Rijken M, Van Klink JMM (2020) High risk of long-term neurodevelopmental impairment in donor twins with spontaneous twin anemia-polycythemia sequence. Ultrasound in obstetrics & gynecology : the official journal of the International Society of Ultrasound in Obstetrics and Gynecology 55(1):39–46. https://doi.org/10.1002/uog.20846
University Hospital Tuebingen (2018) Effects of closed-loop automatic control of FiO2 in extremely preterm infants. https://ClinicalTrials.gov/show/NCT03168516
Martin RJ, Wang K, Koroglu O, Di Fiore J, Kc P (2011) Intermittent hypoxic episodes in preterm infants: do they matter? Neonatology 100(3):303–310. https://doi.org/10.1159/000329922
van Zanten HA, Pauws SC, Stenson BJ, Walther FJ, Lopriore E, te Pas AB (2018) Effect of a smaller target range on the compliance in targeting and distribution of oxygen saturation in preterm infants. Arch Dis Child Fetal Neonatal Ed 103(5):F430-F435. https://doi.org/10.1136/archdischild-2016-312496
Author information
Authors and Affiliations
Contributions
Hylke Salverda, Nathalie Oldenburg, and Arjan Te Pas conceived the study. Hylke Salverda, Nathalie Oldenburg, and Jeanine van Klink conducted the study and collected data. Hylke Salverda analysed the data and wrote the first draft of the manuscript. Hylke Salverda and Jeanine van Klink interpreted the data. Monique Rijken and Ratna Tan performed neonatal follow-up. All authors reviewed the manuscript, provided revisions, and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval
This is an observational study. The ethical board of the Leiden University Medical Center provided a statement of no objection for obtaining and publishing the anonymised data.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
AtP has received an unrestricted research grant from SLE Limited; they had no role in the study design nor in the collection, analysis, and interpretation of data, writing of the report, and decision to submit the paper for publication.
Additional information
Communicated by Daniele De Luca.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Salverda, H.H., Oldenburger, N.J., Rijken, M. et al. Automated oxygen control for very preterm infants and neurodevelopmental outcome at 2 years−a retrospective cohort study. Eur J Pediatr 182, 1593–1599 (2023). https://doi.org/10.1007/s00431-023-04809-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-023-04809-4