Abstract
Health-Related Quality of Life (HRQoL) after Pediatric Intensive Care Unit (PICU) admission is considered a valuable outcome measure. Yet, data on HRQoL after PICU admission are scarce and often collected in heterogeneous patient groups. The current study aimed to evaluate HRQoL in children with bronchiolitis 6 months after PICU admission, which represents a homogenous patient group. This study was conducted at the Radboud University Medical Centre in the Netherlands. Children admitted to the PICU between November 2019 and April 2020 were eligible. HRQoL was assessed with the “TNO-AZL Preschool children Quality of Life” (TAPQOL) questionnaire and compared to Dutch normative data. Lower scores represent worse HRQoL. HRQoL was assessed in 34 children (response rate 81%), mean age at assessment was 7.6 months (SD 2.5 months), and median length of stay was 5 days (range 1–17). Parents reported significant lower scores on stomach problems (p < 0.001; d = 0.8) and lung problems (p < 0.001; d = 1.2) and significant higher scores on appetite (p < 0.001; d = 0.6) and problem behavior (p < 0.001; d = 0.5) compared to normative data. Effect sizes were moderate to large.
Conclusion: Significant differences in several HRQoL domains were found after PICU admission for bronchiolitis compared to normative data. Whereas the domains lung and stomach problems showed significantly impaired scores, most domains revealed HRQoL levels comparable with healthy peers. This study may contribute to the optimization of HRQoL PICU outcomes by highlighting specific HRQoL domains to focus on at admission and during follow-up.
What is Known: • With the decline in PICU mortality, HRQoL became an important outcome measure. Yet, the currently limited number of studies on HRQoL outcomes often involve heterogeneous patient groups. • Bronchiolitis is one of the most frequent reasons for PICU admission, and although a significant part of children admitted for bronchiolitis has a medical history, compared with other reasons for PICU admission, this patient group is relatively homogeneous in terms of age, disease course, and treatment. | |
What is New: • In the present study, six months after PICU admission for bronchiolitis, children scored differently on multiple HRQoL domains compared to healthy peers. • Significantly impaired HRQoL scores were reported on lung and stomach problems in comparison to normative data. |
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The development of the Pediatric Intensive Care Unit (PICU) has contributed to the substantial decline in mortality of children with critical illness [1, 2]. As PICU mortality has become relatively rare over the last decades [1, 3], being 3.8% on Dutch PICU’s nowadays [4], this outcome measure was no longer sufficient to evaluate critical care. Furthermore, the traditional focus on mortality reduction has been broadened to optimization of outcome after PICU admission [5]. Children often experience long-term physical, cognitive, emotional, and social problems post PICU admission, summarized as Post Intensive Care Syndrome in pediatrics (PICS-p) [5]. PICS-p became an important phenomenon since the publication of the PICS-p framework in 2012 [6] and further stimulated the focus on long-term outcome after PICU admission [5].
Patient-Reported Outcome Measures (PROMs) are nowadays a keystone in research and high-quality patient care. A frequently used PROM is Health-Related Quality of Life (HRQoL). HRQoL encompasses the subjective evaluation of physical, social, and emotional functioning. In childhood, HRQoL is influenced by other factors than in adult life, for instance, by developmental capacities [1]. After critical illness, HRQoL measurement can consider the self-perceived impact of illness and PICU admission on the different domains of young children’s lives. Therefore, it adds valuable depth to the measurement of possible sequelae [7]. Aspesberro and colleagues underlined the relevance of HRQoL by stating that “maximising long-term HRQoL might represent the most important goal of medicine in general and intensive care in particular” [1]. Taking HRQoL into account when researching PICS-p expands the understanding of the actual impact on the child’s life.
In the field of pediatric intensive care, the value of long-term HRQoL has been recognized. A review of 78 studies assessing children’s HRQoL after PICU admission suggests a significant impact of critical illness on HRQoL [1]. More specific, pre-planned prospective parts of two large randomized controlled trials revealed significantly lower HRQoL scores among children up to 24 months after PICU admission compared to a normative population in one hand and a matched healthy control group on the other [8,9,10]. Although there is increased knowledge on sequelae after critical illness, much less is known about long-term effects of PICU admission specifically in young children [7]. Moreover, since available data are heterogeneous in terms of age, disease course, and treatment, the effect of PICU admission on post-discharge HRQoL remains unclear, hindering the translation of existing data into clinical practice. By evaluating HRQoL in a relatively homogeneous patient group, the impact of PICU admission on HRQoL might be clarified.
Bronchiolitis is an acute respiratory tract infection and is one of the most common non-elective indication for PICU admission [11]. Bronchiolitis is often a clinical diagnosis and can be caused by multiple viral pathogens. Research to date into long-term outcome after PICU admission for bronchiolitis is scarce [11, 12]. As bronchiolitis usually causes admission in previously healthy children during the first 5 months of life [13], this concerns a homogenous patient group regarding mainly age and treatment and to a lesser extent history. Thus, with the relatively high incidence of bronchiolitis and the importance of HRQoL as outcome measure, a relevant research issue is raised [11, 14].
The primary aim of the current study was to evaluate HRQoL in children 6 months after PICU admission for bronchiolitis. Based on the aforementioned studies on HRQoL in different PICU populations, we hypothesized that HRQoL would be lower in these children as compared to normative data. This research can help optimize PICU treatment by giving specific attention to the affected domains during admission and follow-up.
Materials and methods
Participants
This prospective cohort study is part of the “Long-tErM Outcome after broNchiolitis”-trial (LEMON-trial, CMO file 202–6527). It has been conducted in the eight-bed general tertiary PICU of the Radboud University Medical Centre (Radboudumc) in the Netherlands. Children admitted between November 2019 and April 2020 were eligible for participation. This timeframe encloses one “bronchiolitis season” in the Netherlands and was for the vast majority before the start of the Covid-19 pandemic. The local Medical Ethics Committee has approved the study protocol. Informed consent was obtained from all participating parents.
Procedure
Parents were approached 6 months (range 3–7) after PICU discharge. Contact details from all parents were extracted from the electronic patient record without opening the patient file. Parents were contacted by telephone and were given the option to complete the questionnaire either by telephone or digitally.
Patient characteristics were obtained from the patient record. The Pediatric Risk of Mortality Score III (PRISM-III) and Pediatric Index of Mortality score (PIM2) were obtained from a pre-existing database [15, 16]. Parents were asked if their child had been re-admitted to a hospital and, if so, for what reason. Parental demographic data were collected as well.
Health-related quality of life measure
The TNO-AZL Preschool children Quality of Life (TAPQOL) questionnaire is a scientifically widely used and validated questionnaire to evaluate the domains of HRQoL in pre-school children [17]. For children up to 1.5 years old, the instrument contains 32 items clustered into nine domains: stomach problems, skin problems, lung problems, sleeping, appetite, positive mood, anxiety, liveliness, and problem behavior. The definition of each domain can be found in Supplementary material. To determine HRQoL, most items consist of two sub-questions. The first one assesses the existence of a complaint or functional limitation during the past 3 months. The second question assesses the child’s reaction to that problem. On the domains liveliness, positive mood, problem behavior, and anxiety, there is no second sub-question, because these domains already include an emotional dimension. As HRQoL is defined as a multi-dimensional construct, no total score is calculated.
The TAPQOL was developed and validated for children of at least 1-year old but proved to have adequate psychometric properties in younger children [17,18,19]. Criterion validity has been reported good for all domains in the questionnaire, confirming that it can distinguish between healthy and less healthy children [20].
Statistical analysis
Data management and analysis were performed using SPSS version 26.0. Following the scoring instructions of the TAPQOL, the scores per domain were summed and transformed into 0 (worst possible health state) to 100 (best possible health state) scale scores. Likewise, missing data were imputed on the basis of the TAPQOL manual [20]. This guideline allows domains with at least four items to have one item missing, whereby scores of the other three items are extrapolated to a total scale score. As data were skewed, the Mann–Whitney U test was performed to compare the scores to normative data. Cohen's d effect sizes were determined to assess the magnitude of the differences in mean scores between the patient group and the normative population. Effect sizes were calculated by dividing the difference in the mean scores, by the standard deviation (SD) of the normative group. Effect sizes < 0.5 were considered small, ≥ 0.5 moderate and ≥ 0.8 large [21]. The original dataset of the normative Dutch group was provided by the TAPQOL manual [20].
Results
Study population
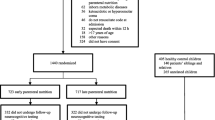
The flowchart of inclusion is depicted in Fig. 1.
Table 1 shows the child, parent, and admission characteristics. Ten children (29%) had a medical history, including congenital neurological disease (n = 1), congenital cardiac disease (n = 2), palatoschisis (n = 1), prematurity (n = 5), and extreme prematurity (n = 1). One child had congenital cerebellar ataxia, also known as Joubert Syndrome. This child had a congenital cardiac disease as well, which was considered part of the syndrome. Therefore, this child is categorized as having a congenital neurological disease. Five of the nine children who were hospitalized during the follow-up interval had no medical history, and in these cases, the admission was due to a respiratory problem. The other admissions were in relation to each child’s described medical history.
Health-related quality of life scores
The results obtained from the TAPQOL questionnaire are presented in Table 2. One parent did not fully complete the questionnaire on three domains, resulting in a study group containing 33 instead of 34 children in these domains.
Discussion
The current study described HRQoL in children 6 months after PICU admission for bronchiolitis as reported by their parents. Statistically significant worse HRQoL scores were reported on lung and stomach problems compared to normative data. Effect sizes on these domains were large. Furthermore, in comparison to normative data, better HRQoL scores were found on appetite and behavior problems with moderate effect sizes.
The current study results align with earlier research using a multi-domain HRQoL measure after critical illness [9, 10, 23]. These studies established the significant impact of critical illness on HRQoL by comparing patients to a normative group [9, 10, 23]. Results in these studies were presented in specific age groups but not in specific diseases. In a recent study, Hordijk and colleagues found the majority of HRQoL domains to be significantly lower after PICU admission, with moderate to large effect sizes, compared to normative data [9]. These scores were found in a large cohort of young children (n = 390, median age 0.4 years) with heterogeneous reasons for PICU admission, for example, cardiac surgery. In the current study, fewer domains showed significant impairment, which could be explained by the relatively good prognosis of bronchiolitis—including low mortality and generally recovery without sequelae—compared to the children in the study of Hordijk et al. Further, the instrument used by Hordijk and colleagues contains different HRQoL domains [9], and these domains are not completely comparable to the domains described in the current study. Regarding this issue, the study of Knoester and colleagues [23] allows a more precise comparison to our study since the TAPQOL was also used in their study. Similar to our results, significant more lung problems were found (after 3 and 9 months) in the youngest subgroup (1–6 years) after PICU admission. In general, the reported impaired HRQoL domains are in line with the described earlier studies.
The domains appetite and problem behavior are scored higher in the current study group than in the normative population, which might be explained by response shift. Response shift is an important subject in HRQoL studies and has earlier been described in the same TAPQOL domains [23]. It refers to a change in an individual’s internal standard or personal values, comparable to an internal “recalibration” [24]. In the current study, the scores might have been influenced by reprioritizing concerns of parents due to the experienced stress when their child was struck by critical illness. A second explanation for these higher scored domains could be the distinction in age between the study group and normative group (mean age 2.5 years). The development of children is age-specific. Therefore, it is imaginable that young children score better on appetite and behavior problems than older children, independent of PICU admission. Previous studies confirm this theory, as healthy children up to 1-year old score higher on the appetite and problem behavior domains than healthy children above 1-year old [17, 25].
Comparing our results to studies using other HRQoL measures [26,27,28,29] is complicated due to the wide variety in HRQoL instruments, lack of consistency on the HRQoL definition, lack of consensus on which instrument is most appropriate in pediatrics, and the frequent provision of a single-score summary HRQoL classification [24, 30]. For example, studies conducting the Health Utility Index (HUI) stated that approximately 80% of children have a “good” QoL 1–3 years after PICU admission [26, 29]. This considered, we cannot conclude whether our results are in agreement with these earlier studies or not, which underlines the need for concurrence on pediatric HRQoL instruments.
As part of this study, psychological problems in parents were evaluated [31]. Prevalence of Post-Traumatic Stress Disorder (PTSD), anxiety, and depression were found to be higher in the study group compared to Dutch normative data. These psychological problems might affect how parents complete questionnaires about their children’s HRQoL. Furthermore, negative long-term physical outcomes in children after a PICU admission might influence psychological well-being of parents. This interaction is an area requiring further research.
Limitations and strengths
The current study has a number of limitations that should be taken into account. First, HRQoL was measured at a single time point after discharge. After PICU admission, (HR)QoL seems to improve over time [23, 32,33,34]. Since time between discharge and outcome assessment varies in our study (range 3–7 months), the presented results may underestimate and overestimate the effect on HRQoL after three and 7 months, respectively. Another consequence of conducting a single measurement is the absence of a baseline HRQoL. Because the pre-morbid state is an important factor of HRQoL [2], this is a shortcoming of this study.
Second, there is a possibility of selection bias. In comparison to the general Dutch population, the mothers of the children that participated in our study had a higher educational level [35]. In the study of de Laat et al. [36], mothers with low levels of education reported more psychosocial problems in their children compared to highly educated mothers. Based on that study, it could be possible that the prevalence of psychosocial problems, and thereby the effect on HRQoL in the current patient group is underestimated. Nevertheless, the high response rate in the current study generally contributes to reliability by reducing the chance of selection bias.
Third, the results in this study are influenced by limitations of the used questionnaire and its application. The TAPQOL is validated for children from the age of 6 months. Yet, few children in this study were younger than this age. Since these were small numbers and the margin between their age and 6 months included at most a few weeks (i.e., 5 children between 5.5 and 6 months of age and 3 children between 5.0 and 5.5 children of age), the same reference values were used for these children as for the entire group. In addition, the TAPQOL is known to show ceiling effects, and the domain “stomach problems” has rather weak reliability (α = 0.39–0.51) [17, 18, 25]. Furthermore, part of the questionnaires was administered by phone. Parents may provide more socially desirable answers over the phone, which may have influenced our results. Moreover, the usage of proxy report by the TAPQOL can cause bias, as the mental HRQoL of the parents is correlated to the HRQoL they report for their child [9]. The psychological condition of the parents in this study could have been altered due to the critical illness of their child, the COVID-19 crisis during the measurement period, or both. Nevertheless, parents are the most closely involved people in a young child’s life, making them the most reliable source of information [9].
Fourth, due to the relatively small sample size, determinants of HRQoL were not investigated, which may cause bias. For example, length of stay and severity of illness influence the HRQoL after PICU stay [9, 33, 34]. However, the homogeneity in our study group minimizes this possibility.
Implications
The evolving phenomenon known as PICS-p typically focuses on physical, cognitive, emotional, and social health. Taking HRQoL into account when researching PICS-p expands the understanding of the actual impact on the child's life [7]. Our study can strengthen the already initiated change into focusing on long-term PICU outcomes. Acknowledgement of long-term outcomes might be helpful to initiate timely interventions to reduce morbidity. This in an excellent fit with the recently started national PICU follow-up program in the Netherlands.
To develop a complete picture of HRQoL after PICU admission for bronchiolitis, standardized measurements over time, with an instrument specially designed for young children, are needed. If risk factors for impaired HRQoL could be identified, close follow-up could be set out for those children most in need.
Conclusion
Six months after PICU admission for bronchiolitis, children in the current study group are found to score significantly different on multiple HRQoL domains compared to Dutch normative data. Significantly impaired HRQoL scores were reported on lung and stomach problems in comparison to the normative group. Despite the fact that bronchiolitis is known for its relatively good prognosis nowadays, the present study shows that it can still influence HRQoL 6 months after PICU discharge. Recognition of long-term outcomes may be useful for timely identification of children at risk of deterioration in HRQoL after PICU admission and for taking measures to reduce morbidity.
Availability of data and material
The dataset generated during this study is available from the corresponding author on reasonable request.
Code availability
SPSS version 26.0 was utilized to run statistical analysis.
Abbreviations
- HRQoL:
-
Health-Related Quality of Life
- HUI:
-
Health utility index
- PICS-p :
-
Post Intensive Care Syndrome in pediatrics
- PICU:
-
Pediatric Intensive Care Unit
- PIM2:
-
Pediatric Index of Mortality score 2
- PRISM-III:
-
Pediatric Risk of Mortality Score III
- PROM:
-
Patient-Reported Outcome Measure
- Radboudumc:
-
Radboud University Medical Centre
- SD:
-
Standard deviation
- TAPQOL:
-
TNO-AZL Preschool children Quality of Life
References
Aspesberro F, Mangione-Smith R, Zimmerman JJ (2015) Health-related quality of life following pediatric critical illness. Intensive Care Med 41(7):1235–1246. https://doi.org/10.1007/s00134-015-3780-7
Knoester H, Grootenhuis MA, Bos AP (2007) Outcome of paediatric intensive care survivors. Eur J Pediatr 166(11):1119–1128. https://doi.org/10.1007/s00431-007-0573-1
Butt W, Shann F, Tibballs J, Williams J, Cuddihy L, Blewett L, Farley M (1990) Long-term outcome of children after intensive care. Crit Care Med 18(9):961–965. https://doi.org/10.1097/00003246-199009000-00011
Visser I, PICE Working Group (2011) Pediatric intensive care evaluation annual report. Rotterdam: PICE foundation
Manning JC, Pinto NP, Rennick JE, Colville G, Curley MAQ (2018) Conceptualizing post intensive care syndrome in children-the PICS-p framework. Pediatr Crit Care Med 19(4):298–300. https://doi.org/10.1097/pcc.0000000000001476
Needham DM, Davidson J, Cohen H, Hopkins RO, Weinert C, Wunsch H, Zawistowski C, Bemis-Dougherty A, Berney SC, Bienvenu OJ et al (2012) Improving long-term outcomes after discharge from intensive care unit: report from a stakeholders’ conference. Crit Care Med 40(2):502–509. https://doi.org/10.1097/CCM.0b013e318232da75
Watson RS, Choong K, Colville G, Crow S, Dervan LA, Hopkins RO, Knoester H, Pollack MM, Rennick J, Curley MAQ (2018) Life after critical illness in children-toward an understanding of pediatric post-intensive care syndrome. J Pediatr 198:16–24. https://doi.org/10.1016/j.jpeds.2017.12.084
Hordijk J, Verbruggen S, Vanhorebeek I, Güiza F, Wouters P, Van den Berghe G, Joosten K, Dulfer K (2020) Health-related quality of life of children and their parents 2 years after critical illness: pre-planned follow-up of the PEPaNIC international, randomized, controlled trial. Crit Care 24(1):347. https://doi.org/10.1186/s13054-020-03059-2
Hordijk J, Verbruggen S, Vanhorebeek I, Van den Berghe G, Utens E, Joosten K, Dulfer K (2020) Health-related quality of life of children and their parents 6 months after children’s critical illness. Qual Life Res 29(1):179–189. https://doi.org/10.1007/s11136-019-02347-x
Vet NJ, de Wildt SN, Verlaat CW, Mooij MG, Tibboel D, de Hoog M, Buysse CM (2016) Short-term health-related quality of life of critically ill children following daily sedation interruption. Pediatr Crit Care Med 17(11):e513–e520. https://doi.org/10.1097/pcc.0000000000000956
Bem RA, Bont LJ, van Woensel JBM (2020) Life-threatening bronchiolitis in children: eight decades of critical care. Lancet Respiratory Med 8(2):142–144. https://doi.org/10.1016/s2213-2600(19)30445-x
Shein SL, Slain KN, Clayton JA, McKee B, Rotta AT, Wilson-Costello D (2017) Neurologic and functional morbidity in critically ill children with bronchiolitis. Pediatr Crit Care Med 18(12):1106–1113. https://doi.org/10.1097/pcc.0000000000001337
Meissner HC (2016) Viral bronchiolitis in children. N Engl J Med 374(1):62–72. https://doi.org/10.1056/NEJMra1413456
Principi T, Fraser DD, Morrison GC, Farsi SA, Carrelas JF, Maurice EA, Kornecki A (2011) Complications of mechanical ventilation in the pediatric population. Pediatr Pulmonol 46(5):452–457. https://doi.org/10.1002/ppul.21389
Pollack MM, Patel KM, Ruttimann UE (1996) PRISM III: an updated pediatric risk of mortality score. Crit Care Med 24(5):743–752. https://doi.org/10.1097/00003246-199605000-00004
Slater A, Shann F, Pearson G (2003) PIM2: a revised version of the paediatric index of mortality. Intensive Care Med 29(2):278–285. https://doi.org/10.1007/s00134-002-1601-2
Bunge EM, Essink-Bot ML, Kobussen MP, van Suijlekom-Smit LW, Moll HA, Raat H (2005) Reliability and validity of health status measurement by the TAPQOL. Arch Dis Child 90(4):351–358. https://doi.org/10.1136/adc.2003.048645
Fekkes M, Theunissen NC, Brugman E, Veen S, Verrips EG, Koopman HM, Vogels T, Wit JM, Verloove-Vanhorick SP (2000) Development and psychometric evaluation of the TAPQOL: a health-related quality of life instrument for 1–5-year-old children. Qual Life Res 9(8):961–972. https://doi.org/10.1023/a:1008981603178
Theunissen NC, Veen S, Fekkes M, Koopman HM, Zwinderman KA, Brugman E, Wit JM (2001) Quality of life in preschool children born preterm. Dev Med Child Neurol 43(7):460–465. https://doi.org/10.1017/s0012162201000846
Fekkes M, Bruil J, Vogels T (2003) TAPQOL-manual Leiden. TNO Prevention and Health
Cohen J (1988) Statistical power analysis for the bevaioral sciences. Academy Press, New York
Kunst AE, Dalstra JAA, Bos V, Machenbach JP (2005) Ontwikkeling en toepassing van indicatoren van sociaal-economische status binnen het Gezondheidsstatistisch Bestand. In U. M. C. R. Afdeling Maatschappelijke Gezondheidszorg (Ed.): Centraal Bureau voor de Statisiek
Knoester H, Bronner MB, Bos AP, Grootenhuis MA (2008) Quality of life in children three and nine months after discharge from a paediatric intensive care unit: a prospective cohort study. Health Qual Life Outcomes 6:21. https://doi.org/10.1186/1477-7525-6-21
De Civita M, Regier D, Alamgir AH, Anis AH, Fitzgerald MJ, Marra CA (2005) Evaluating health-related quality-of-life studies in paediatric populations: some conceptual, methodological and developmental considerations and recent applications. Pharmacoeconomics 23(7):659–685. https://doi.org/10.2165/00019053-200523070-00003
Schepers SA, van Oers HA, Maurice-Stam H, Huisman J, Verhaak CM, Grootenhuis MA, Haverman L (2017) Health related quality of life in Dutch infants, toddlers, and young children. Health Qual Life Outcomes 15(1):81. https://doi.org/10.1186/s12955-017-0654-4
Ambuehl J, Karrer A, Meer A, Riedel T, Schibler A (2007) Quality of life of survivors of paediatric intensive care. Swiss Med Wkly 137(21–22):312–316
Gemke RJ, Bonsel GJ, van Vught AJ (1995) Long-term survival and state of health after paediatric intensive care. Arch Dis Child 73(3):196–201. https://doi.org/10.1136/adc.73.3.196
Jones S, Rantell K, Stevens K, Colwell B, Ratcliffe JR, Holland P, Rowan K, Parry GJ (2006) Outcome at 6 months after admission for pediatric intensive care: a report of a national study of pediatric intensive care units in the United kingdom. Pediatrics 118(5):2101–2108. https://doi.org/10.1542/peds.2006-1455
Taylor A, Butt W, Ciardulli M (2003) The functional outcome and quality of life of children after admission to an intensive care unit. Intensive Care Med 29(5):795–800. https://doi.org/10.1007/s00134-003-1690-6
Horsman J, Furlong W, Feeny D, Torrance G (2003) The health utilities index (HUI): concepts, measurement properties and applications. Health Qual Life Outcomes 1:54. https://doi.org/10.1186/1477-7525-1-54
van Benthum MV, van Dijk T, Maas-van Schaaijk NM, van Zwol A (2022) Psychological problems in parents of children with bronchiolitis following paediatric intensive care unit (PICU) admission. Acta Paediatr 111(5):1054–1055. https://doi.org/10.1111/apa.16272
Choong K, Fraser D, Al-Harbi S, Borham A, Cameron J, Cameron S, Cheng J, Clark H, Doherty T, Fayed N et al (2018) Functional recovery in critically ill children, the “WeeCover” multicenter study. Pediatr Crit Care Med 19(2):145–154. https://doi.org/10.1097/pcc.0000000000001421
Morrison AL, Gillis J, O’Connell AJ, Schell DN, Dossetor DR, Mellis C (2002) Quality of life of survivors of pediatric intensive care. Pediatr Crit Care Med 3(1):1–5. https://doi.org/10.1097/00130478-200201000-00001
Polic B, Mestrovic J, Markic J, Mestrovic M, Capkun V, Utrobicic I, Jukica M, Radonic M (2013) Long-term quality of life of patients treated in paediatric intensive care unit. Eur J Pediatr 172(1):85–90. https://doi.org/10.1007/s00431-012-1843-0
Statistical Office of the European Communities, Level of education of the mother (% of specified population) (2019) EUROSTAT: regional statistics. Accessed 14 June 2022 https://ec.europa.eu/eurostat/statistics-explained/index.php?title=File:Level_of_education_of_the_mother,_2019_(%25_of_specified_population).png
de Laat SA, Essink-Bot ML, van Wassenaer-Leemhuis AG, Vrijkotte TG (2015) Preterm birth and low socioeconomic status: more psychosocial problems at age 5–6? Ned Tijdschr Geneeskd 160:D34
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Tessel van Dijk and Milou V. van Benthum. Annelies van Zwol and Nienke M. Maas-van Schaaijk supervised the study. The first draft of the manuscript was written by Tessel van Dijk, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee of the Radboud University Medical Centre (file 202–6527) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from the parents.
Competing interests
The authors declare no competing interests.
Additional information
Communicated by Peter de Winter
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
van Dijk, T., van Benthum, M.V., Maas-van Schaaijk, N.M. et al. Health-related quality of life 6 months after pediatric intensive care unit admission for bronchiolitis: a prospective single-center cohort study. Eur J Pediatr 182, 403–409 (2023). https://doi.org/10.1007/s00431-022-04700-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-022-04700-8