Abstract
We retrospectively reviewed the data of 140 female pediatric patients with rare mitochondrial diseases (MDs) confirmed using muscle biopsy. We evaluated patients who were diagnosed with central precocious puberty (PP) with early pubertal development to determine whether PP is a clinical manifestation of MDs. We also examined the clinical, auxiological, laboratory, and radiological parameters after 1 year of gonadotropin-releasing hormone treatment for central PP. Among the 140 girls with MDs, 29 had early pubertal development and underwent endocrine evaluation. Ten (7.1%) patients were diagnosed with central PP; the prevalence of central PP was higher than was that previously thought. Patients with central PP exhibited bone age advancement over 1 year and increased sex hormone levels despite their young age at diagnosis. Serum estradiol levels were significantly higher in younger patients than in older patients (P = 0.004). Patients with central PP treated with gonadotropin-releasing hormone had favorable outcomes, and their pubertal development was suppressed for 1 year.
Conclusion: Central PP may be a manifestation of endocrine dysfunction in young girls with MDs.
What is Known: • The general characteristics of mitochondrial diseases include developmental delays and retarded growth. • Precocious puberty has rarely been suggested as a clinical manifestation of mitochondrial diseases. What is New: • Among the 140 girls with mitochondrial diseases, 10 (7.1%) were diagnosed with central precocious puberty. • Serum estradiol levels were significantly higher in younger patients than in older patients. |

Similar content being viewed by others
Abbreviations
- E2:
-
Estradiol
- FSH:
-
Follicular-stimulating hormone
- GnRH:
-
Gonadotropin-releasing hormone
- LH:
-
Luteinizing hormone
- MD:
-
Mitochondrial disease
- PP:
-
Precocious puberty
References
Lee YM (2012) Mitochondrial diseases. J Epilepsy Res 2(1):1–4. https://doi.org/10.14581/jer.12001
Ardissone A, Lamantea E, Invernizzi F, Zeviani M, Genitrini S, Moroni I, Uziel G (2014) Mitochondrial diseases in childhood. Curr Mol Med 14(8):1069–1078. https://doi.org/10.2174/1566524014666141010155317
Gropman AL (2004) The neurological presentations of childhood and adult mitochondrial disease: established syndromes and phenotypic variations. Mitochondrion 4(5–6):503–520. https://doi.org/10.1016/j.mito.2004.07.009
Kim SH, Huh K, Won S, Lee KW, Park MJ (2015) A significant increase in the incidence of central precocious puberty among Korean girls from 2004 to 2010. PLoS One 10(11):e0141844. https://doi.org/10.1371/journal.pone.0141844
Kim YJ, Kwon A, Jung MK, Kim KE, Suh J, Chae HW, Kim DH, Ha S, Seo GH, Kim HS (2019) Incidence and prevalence of central precocious puberty in Korea: an epidemiologic study based on a national database. J Pediatr 208:221–228. https://doi.org/10.1016/j.jpeds.2018.12.022
Berberoglu M (2009) Precocious puberty and normal variant puberty: definition, etiology, diagnosis and current management. J Clin Res Pediatr Endocrinol 1(4):164–174. https://doi.org/10.4274/jcrpe.v1i4.3
Nissenkorn A, Zeharia A, Lev D, Fatal-Valevski A, Barash V, Gutman A, Harel S, Lerman-Sagie T (1999) Multiple presentation of mitochondrial disorders. Arch Dis Child 81(3):209–214. https://doi.org/10.1136/adc.81.3.209
Al-Gadi IS, Haas RH, Falk MJ, Goldstein A, McCormack SE (2018) Endocrine disorders in primary mitochondrial disease. J Endocr Soc 2(4):361–373. https://doi.org/10.1210/js.2017-00434
Bernier FP, Boneh A, Dennett X, Chow CW, Cleary MA, Thorburn DR (2002) Diagnostic criteria for respiratory chain disorders in adults and children. Neurology 59(9):1406–1411
Lee PA (1999) Central precocious puberty. An overview of diagnosis, treatment, and outcome. Endocrinol Metab Clin N Am 28(4):901–918 xi
Latronico AC, Brito VN, Carel JC (2016) Causes, diagnosis, and treatment of central precocious puberty. Lancet Diabetes Endocrinol 4(3):265–274. https://doi.org/10.1016/S2213-8587(15)00380-0
Ahn Y, Choi S, Sohn M (2013) Adiposity of Korean school-age children measured by national and international growth charts. Res Nurs Health 36(1):16–25. https://doi.org/10.1002/nur.21510
Yim CH, Kim GH, Eun BL (2017) Usefulness of the Korean Developmental Screening Test for infants and children for the evaluation of developmental delay in Korean infants and children: a single-center study. Korean J Pediatr 60(10):312–319. https://doi.org/10.3345/kjp.2017.60.10.312
van den Ouweland JM, Lemkes HH, Ruitenbeek W, Sandkuijl LA, de Vijlder MF, Struyvenberg PA, van de Kamp JJ, Maassen JA (1992) Mutation in mitochondrial tRNA(Leu)(UUR) gene in a large pedigree with maternally transmitted type II diabetes mellitus and deafness. Nat Genet 1(5):368–371. https://doi.org/10.1038/ng0892-368
Luoma P, Melberg A, Rinne JO, Kaukonen JA, Nupponen NN, Chalmers RM, Oldfors A, Rautakorpi I, Peltonen L, Majamaa K, Somer H, Suomalainen A (2004) Parkinsonism, premature menopause, and mitochondrial DNA polymerase gamma mutations: clinical and molecular genetic study. Lancet 364(9437):875–882. https://doi.org/10.1016/S0140-6736(04)16983-3
Lamperti C, Diodato D, Lamantea E, Carrara F, Ghezzi D, Mereghetti P, Rizzi R, Zeviani M (2012) MELAS-like encephalomyopathy caused by a new pathogenic mutation in the mitochondrial DNA encoded cytochrome c oxidase subunit I. Neuromuscul Disord 22(11):990–994. https://doi.org/10.1016/j.nmd.2012.06.003
Le Moal J, Rigou A, Le Tertre A, De Crouy-Channel P, Leger J, Carel JC (2018) Marked geographic patterns in the incidence of idiopathic central precocious puberty: a nationwide study in France. Eur J Endocrinol 178(1):33–41. https://doi.org/10.1530/EJE-17-0379
Papadimitriou A, Nicolaidou P, Fretzayas A, Chrousos GP (2010) Clinical review: constitutional advancement of growth, a.k.a. early growth acceleration, predicts early puberty and childhood obesity. J Clin Endocrinol Metab 95(10):4535–4541. https://doi.org/10.1210/jc.2010-0895
Lucaccioni L, Trevisani V, Marrozzini L, Bertoncelli N, Predieri B, Lugli L, Berardi A, Iughetti L (2020) Endocrine-disrupting chemicals and their effects during female puberty: a review of current evidence. Int J Mol Sci 21(6). https://doi.org/10.3390/ijms21062078
Bulus AD, Asci A, Erkekoglu P, Balci A, Andiran N, Kocer-Gumusel B (2016) The evaluation of possible role of endocrine disruptors in central and peripheral precocious puberty. Toxicol Mech Methods 26(7):493–500. https://doi.org/10.3109/15376516.2016.1158894
Brix N, Ernst A, Lauridsen LLB, Parner ET, Arah OA, Olsen J, Henriksen TB, Ramlau-Hansena CH (2020) Childhood overweight and obesity and timing of puberty in boys and girls: cohort and sibling-matched analyses. Int J Epidemiol 49:834–844. https://doi.org/10.1093/ije/dyaa056
Schaefer AM, Walker M, Turnbull DM, Taylor RW (2013) Endocrine disorders in mitochondrial disease. Mol Cell Endocrinol 379(1–2):2–11. https://doi.org/10.1016/j.mce.2013.06.004
Wolny S, McFarland R, Chinnery P, Cheetham T (2009) Abnormal growth in mitochondrial disease. Acta Paediatr 98(3):553–554. https://doi.org/10.1111/j.1651-2227.2008.01148.x
Wheeler MD, Styne DM (1990) Diagnosis and management of precocious puberty. Pediatr Clin N Am 37(6):1255–1271
Chen M, Eugster EA (2015) Central precocious puberty: update on diagnosis and treatment. Paediatr Drugs 17(4):273–281. https://doi.org/10.1007/s40272-015-0130-8
Brauner R, Couto-Silva AC, Chemaitilly W, Adan L, Trivin C (2005) Central precocious puberty in girls: prediction of the etiology. Arch Pediatr 12(11):1661–1664. https://doi.org/10.1016/j.arcped.2005.09.003
Chow J, Rahman J, Achermann JC, Dattani MT, Rahman S (2017) Mitochondrial disease and endocrine dysfunction. Nat Rev Endocrinol 13(2):92–104. https://doi.org/10.1038/nrendo.2016.151
Selin AA, Lobysheva NV, Nesterov SV, Skorobogatova YA, Byvshev IM, Pavlik LL, Mikheeva IB, Moshkov DA, Yaguzhinsky LS, Nartsissov YR (2016) On the regulative role of the glutamate receptor in mitochondria. Biol Chem 397(5):445–458. https://doi.org/10.1515/hsz-2015-0289
Jackson JG, O’Donnell JC, Takano H, Coulter DA, Robinson MB (2014) Neuronal activity and glutamate uptake decrease mitochondrial mobility in astrocytes and position mitochondria near glutamate transporters. J Neurosci 34(5):1613–1624. https://doi.org/10.1523/JNEUROSCI.3510-13.2014
Brook CG (1999) Mechanism of puberty. Horm Res 51(Suppl 3):52–54. https://doi.org/10.1159/000053162
Stojilkovic SS, Krsmanovic LZ, Spergel DJ, Catt KJ (1994) Gonadotropin-releasing hormone neurons: intrinsic pulsatility and receptor-mediated regulation. Trends Endocrinol Metab 5(5):201–209
Chiu CF, Wang CJ, Chen YP, Lo FS (2020) Pathological and incidental findings in 403 Taiwanese girls with central precocious puberty at initial diagnosis. Front Endocrinol (Lausanne) 11:256. https://doi.org/10.3389/fendo.2020.00256
Roth C, Schmidberger H, Lakomek M, Witt O, Wuttke W, Jarry H (2001) Reduction of gamma-aminobutyric acid-ergic neurotransmission as a putative mechanism of radiation induced activation of the gonadotropin releasing-hormone-pulse generator leading to precocious puberty in female rats. Neurosci Lett 297(1):45–48
Author information
Authors and Affiliations
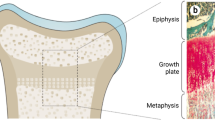
Contributions
HWC researched, wrote, and reviewed the manuscript. JHN conceptualized the study and collected data. AK prepared the tables and figure. HSK contributed to the discussion and reviewed the manuscript. YML researched and reviewed/edited the manuscript. YML is guarantor of this work and, as such, had complete access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. All authors have reviewed the manuscript and have approved the submitted and published versions.
Corresponding author
Ethics declarations
All procedures were approved by the Institutional Review Board (IRB) of Gangnam Severance Hospital, Seoul, South Korea (IRB number 3-2015-0135). Informed consent was obtained from the parent/legal guardian of all patients, and all methods were performed in accordance with the relevant guidelines and regulations of the IRB.
Conflict of interest
The authors declare that there are no conflicts of interest.
Additional information
Communicated by Peter de Winter
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Chae, HW., Na, JH., Kwon, A. et al. Central precocious puberty may be a manifestation of endocrine dysfunction in pediatric patients with mitochondrial disease. Eur J Pediatr 180, 425–432 (2021). https://doi.org/10.1007/s00431-020-03804-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-020-03804-3