Abstract
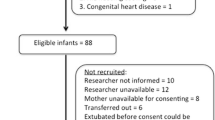
Our aim was to compare the work of breathing (WOB) during synchronised nasal intermittent positive pressure ventilation (SNIPPV) and heated humidified high flow nasal cannula (HHHFNC) when used as post-extubation support in preterm infants. A randomised crossover study was undertaken of nine infants with a median gestational age of 27 (range 24–31) weeks and post-natal age of 7 (range 2–50) days. Infants were randomised to either SNIPPV or HHHFNC immediately following extubation. They were studied for 2 h on one mode and then switched to the other modality and studied for a further 2-h period. The work of breathing, assessed by measuring the pressure time product of the diaphragm (PTPdi), and thoracoabdominal asynchrony (TAA) were determined at the end of each 2-h period. The infants’ inspired oxygen requirement, oxygen saturation, heart rate and respiratory rate were also recorded. The median PTPdi was lower on SNIPPV than on HHHFNC (232 (range 130–352) versus 365 (range 136–449) cmH2O s/min, p = 0.0077), and there was less thoracoabdominal asynchrony (13.4 (range 8.5–41.6) versus 36.1 (range 4.3–50.4) degrees, p = 0.038).
Conclusion: In prematurely born infants, SNIPPV compared to HHHFNC post-extubation reduced the work of breathing and thoracoabdominal asynchrony.
What is Known: • The work of breathing and extubation failure are not significantly different in prematurely-born infants supported by HHHFNC or nCPAP. • SNIPPV reduces inspiratory effort and increases tidal volume and carbon dioxide exchange compared to nCPAP in prematurely born infants. | |
What is New: • SNIPPV, as compared to HHHFNC, reduced the work of breathing in prematurely-born infants studied post-extubation. • SNIPPV, as compared to HHHFNC, reduced thoracoabdominal asynchrony in prematurely born infants studied post-extubation. |

Similar content being viewed by others
Abbreviations
- AB:
-
Abdominal movement
- ABdiff:
-
Difference between inspiratory and expiratory abdominal positions at mid-RC excursion
- ABmax:
-
Maximum abdominal excursion
- BPD:
-
Bronchopulmonary dysplasia
- CPAP:
-
Continuous positive airway pressure
- FiO2 :
-
Inspired oxygen fraction
- HHHFNC:
-
Heated humidified high flow nasal cannula
- PdI:
-
Transdiaphragmatic pressure
- PEEP:
-
Positive end expiratory pressure
- Pgas:
-
Gastric pressures
- PIP:
-
Peak inspiratory pressures
- Poes:
-
Oesophageal pressure
- PTPdi :
-
Pressure time product of the diaphragm
- RC:
-
Rib cage movement
- RIP:
-
Respiratory inductance plethysmography
- SNIPPV:
-
Synchronised nasal intermittent positive pressure ventilation
- TAA:
-
Thoracoabdominal asynchrony
- WOB:
-
Work of breathing
References
Chang HY, Claure N, D’ugard C, Torres J, Nwajei P, Bancalari E (2011) Effects of synchronization during nasal ventilation in clinically stable preterm infants. Pediatr Res 69:84–89
Dysart K, Miller TL, Wolfson MR, Shaffer TH (2009) Research in high flow therapy: mechanisms of action. Respir Med 103:1400–1405
Fischer H, Buehrer C (2013) Avoiding endotracheal ventilation to prevent bronchopulmonary dysplasia: a meta-analysis. Pediatrics 132:e1351–e1360
Fischer HS, Roehr CC, Proquitte H, Hammer H, Wauer RR, Schmalisch G (2009) Is volume and leak monitoring feasible during nasopharyngeal continuous positive airway pressure in neonates? Intensive Care Med 35:1934–1941
Gizzi C, Montecchia F, Panetta V, Castellano C, Mariani C, Campelli M, Papoff P, Moretti C, Agostino R (2015) Is synchronised NIPPV more effective than NIPPV and NCPAP in treating apnoea of prematurity (AOP)?. A randomised cross-over trial. Arch Dis Child Fetal Neonatal Ed 100:F17–F23
Hermeto F, Martins BM, Ramos JR, Bhering CA, Sant'Anna GM (2009) Incidence and main risk factors associated with extubation failure in newborns with birth weight< 1,250 grams. J Pediatr 85:397–402
Huang L, Mendler MR, Waitz M, Schmid M, Hassan MA, Hummler HD (2015) Effects of synchronization during noninvasive intermittent mandatory ventilation in preterm infants with respiratory distress syndrome immediately after extubation. Neonatology 108:108–114
Lampland AL, Plumm B, Meyers P, Worwa CT, Mammel MC (2009) Observational study of humidified high-flow nasal cannula compared with nasal continuous positive airway pressure. J Pediatr 154:177–182
Lavizzari A, Veneroni C, Colnaghi M, Ciuffini F, Zannin E, Fumagalli M, Mosca F, Dellacà RL (2014) Respiratory mechanics during NCPAP and HHHFNC at equal distending pressures. Arch Dis Child Fetal Neonatal Ed 99:F315–F320
Leymyre B, Davis PG, De Paoli AG, Kirpalani H (2017) Nasal intermittent positive pressure ventilation (NIPPV) versus nasal continuous positive airway pressure (NCPAP) for preterm neonates after extubation. Cochrane Database Syst Rec 2:CD003212
Mahmoud RA, Roehr CC, Schmalisch G (2011) Current methods of non-invasive ventilatory support for neonates. Paediatr Respir Rev 12:196–205
Moretti C, Gizzi C, Papoff P, Lampariello S, Capoferri M, Calcagnini G, Bucci G (1999) Comparing the effects of nasal synchronized intermittent positive pressure ventilation (nSIPPV) and nasal continuous positive airway pressure (nCPAP) after extubation in very low birth weight infants. Early Hum Dev 56:167–177
Moretti C, Papoff P, Gizzi C, Montecchia F, Giannini L, Fassi C, Midulla F, Agostino R, Sanchez-Luna M (2013) Flow-synchronized nasal intermittent positive pressure ventilation in the preterm infant: development of a project. JPNIM 2:e020211
Ojha S, Gridley E, Dorling J (2013) Use of heated humidified high-flow nasal cannula oxygen in neonates: a UK wide survey. Acta Paediatr 102:249–253
Owen LS, Manley BJ (2016) Nasal intermittent positive pressure ventilation in preterm infants: equipment, evidence, and synchronization. Sem Fetal Neonatal Med 21:146–153
Owen LS, Morley CJ, Davis PG (2008) Neonatal nasal intermittent positive pressure ventilation: a survey of practice in England. Arch Dis Child Fetal Neonatal Ed 93:F148–F150
Owen LS, Morley CJ, Dawson JA, Davis PG (2011) Effects of non-synchronised nasal intermittent positive pressure ventilation on spontaneous breathing in preterm infants. Arch Dis Child Fetal Neonatal Ed 96:F422–F428
Ramos-Navarro C, Sanchez-Luna M, Sanz-Lopez E, Maderuelo-Rodriguez E, Zamora-Flores E (2016) Effectiveness of synchronized noninvasive ventilation to prevent intubation in preterm infants. AJP Rep 6:e264–e271
S.E. Ltd. Create a blocked randomisation list. 2016. Available from: https://www.sealedenvelope.com/simple-randomiser/v1/lists
Shetty S, Hickey A, Rafferty GF, Peacock JL, Greenough A (2016) Work of breathing during CPAP and heated humidified high-flow nasal cannula. Arch Dis Child Fetal Neonatal Ed 101:F404–F407
Shetty S, Sundaresan A, Hunt K, Desai P, Greenough A (2016) Changes in the use of humidified high flow nasal cannula oxygen. Arch Dis Child Fetal Neonatal Ed 101:F371–F372
Wilkinson D, Andersen C, O’Donnell CP, De Paoli AG, Manley BJ (2016) High flow nasal cannula for respiratory support in preterm infants. Cochrane Database Syst Rev 2:CD006405
Funding
Dr. Hunt was supported by the Charles Wolfson Charitable Trust and additionally by SLE. Dr. Elinor Charles was supported by the Isaac Shapera Fund. The research was supported by the National Institute for Health Research (NIHR) Biomedical Research Centre based at Guy’s and St Thomas’ NHS Foundation Trust and King’s College London. The views expressed are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health. Professor Janet Peacock is an NIHR Senior Investigator. The Guilia ventilated was loaned to us by Gineviri Medical Technologies (see comments re competing interests).
Author information
Authors and Affiliations
Contributions
AG, KAH and GFR designed the study. EC and KAH collected the data. JFP, EC, KAH and AG analysed the data. All authors were involved in the production of the manuscript and approved the final version.
Corresponding authors
Ethics declarations
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Conflict of interest
Professor Greenough has held grants from various manufacturers (Abbot Laboratories, MedImmune) and ventilator manufacturers (SLE). Professor Greenough has received honoraria for giving lectures and advising various manufacturers (Abbot Laboratories, MedImmune) and ventilator manufacturers (SLE). Professor Greenough is currently receiving a non-conditional educational grant from SLE. The Guilia ventilator was loaded to us by Ginevri Medical Technologies; they have not been involved in the data collection analysis or production of the manuscript.
Informed consent
Infants whose parents gave informed written consent were enrolled into the study.
Additional information
Communicated by Patrick Van Reempts
Elinor Charles and Katie A Hunt are joint first authors.
Rights and permissions
About this article
Cite this article
Charles, E., Hunt, K.A., Rafferty, G.F. et al. Work of breathing during HHHFNC and synchronised NIPPV following extubation. Eur J Pediatr 178, 105–110 (2019). https://doi.org/10.1007/s00431-018-3254-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-018-3254-3