Abstract
Surgical resection for hepatocellular carcinoma (HCC) is burdened with a high recurrence rate and a lack of reliable prognostic factors. The aim of this study was to integrate the HCC pathological features with gene mutations to improve the prognostic role of pathological analysis. This is a monocentric prospective study, including 67 patients resected for HCC. All clinical data and histological features were collected, including tumor grade, architecture, margins, microvascular invasion, and microscopic portal vascular invasion (MPVI). Next-generation sequencing (NGS) was performed using a laboratory-developed multi-gene panel, allowing to amplify 330 amplicons (21.77 kb), covering the relevant targets for solid tumor analysis. The most represented mutations were TERT promoter (n = 41, 61.2%), TP53 (n = 18, 26.9%) and CTNNB1 (n = 17, 25.4%). At follow-up, 13 (19.4%) patients experienced HCC recurrence: at multivariate analysis, tumor dimensions (p = 0.040), MPVI (p = 0.010), and TERT mutation (p = 0.034) correlated with recurrence. Dimensions ≥ 4.5 cm (very close to AJCC stage pT3; 9 recurrences, p = 0.041, odd-ratio = 3.7), MPVI (9 recurrences, p = 0.062, OR = 3.3), and TERT (11 recurrences, p = 0.049, OR = 4.4) correlated with disease-free survival also at univariate analysis. The concomitant occurrence of these three variables was present in 7 cases, among which 5 recurred (p = 0.002, OR = 15.94). In conclusion, NGS analysis in resected HCC could not only be used for future therapies but should be integrated with histopathology to predict the risk of tumor recurrence after surgical resection: TERT mutation is among the strongest predictors of tumor recurrence, together with tumor stage (dimensions) and the occurrence of MPVI, which should always be reported separately from the classic MVI.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Surgical resection is one of the treatments of choice for hepatocellular carcinoma (HCC) in not cirrhotic livers, as well as in very early and early-stage HCCs in cirrhotic livers with good function [1]. According to the European Association for the Study of the Liver (EASL), the recurrence rate of HCC after any therapy—including de novo new HCCs—is still very high (up to 70%), impacting long-term patient prognosis [1, 2]. Compared to other therapeutic options, surgical resection has the advantage of giving more predictive information, due to the availability of tumor tissue and histopathological features associated with HCC aggressiveness, such as grade, architecture, and microvascular invasion (MVI) [3, 4]. Recently, the presence of MVI in the portal veins (microscopic portal vascular invasion, MPVI) was associated with a worse prognosis, in terms of direct correlation with serum alpha-fetoprotein and post-surgical tumor recurrence, compared to “simple” MVI [5]. This demonstrates how histopathological analysis can still be contributory, albeit its role in the prediction of HCC recurrence is still underrated since no standard pathological algorithms exist.
The availability of tumor tissue has the advantage of allowing molecular analyses as well: in the last years, many approaches have been proposed, from microRNAs [6, 7] to gene hypermethylations [8, 9] and mutational profile, especially mutations in the promoter telomerase reverse transcriptase gene (TERT) [10, 11]. It is established that HCC, despite the wide clinical and morphological heterogeneity, is typically not burdened by a high number of mutations, the most common driver mutations being in the TP53, CTNNB1, and TERT-promoter genes [10, 12]. The β-catenin and p53 pathways have been proposed for a molecular classification of HCC [10, 13], but the lack of strong evidence and clinical applications left these findings in the theory. The CTNNB1 gene (encoding for β-catenin) is mutated in approximately one-third of HCC, described as low-grade trabecular-acinar tumors by the original work by Calderaro et al. [13] The frequency of TP53 mutations in HCC is variable according to the series considered in the literature, from 15 to 40%: TP53 mutation characterizes high-grade, more aggressive HCC, and it was correlated to aflatoxin exposure and HBV infection [10, 13]. TERT promoter is far less studied in liver cancers, also because this promoter region is not covered by the exome sequencing methods usually used. However, more than half of HCCs show TERT promoter mutation, and some preliminary studies showed a promising correlation between TERT mutation and worse prognosis in HCC patients [11, 14].
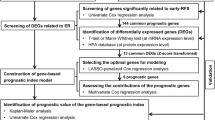
The state-of-the-art routine management of resected HCC patients does not include a tissue algorithm able to combine the usual histopathological variables with molecular biology data (as it is in other human cancers), and the fact that no correlations seem to exist between HCC morphology and mutational status discourages further the research of a more rational approach [15]. The aim of the present study was to integrate the HCC pathological features with gene mutations to find a prognostic tissue algorithm in resected HCC patients, improving the prognostic role of pathological analysis.
Materials and methods
Disclosure of ethical statements
Approval of the research protocol: Approved by the Ethical Committee of the Area Vasta Emilia-Romagna (AVEC), protocol Nr. HCCNGS_2021.
Informed Consent: informed consent was obtained by all enrolled patients.
Registry and the Registration No. of the study/trial:
Animal Studies: N/A.
Research involving recombinant DNA: N/A.
Patient enrollment
This is a monocentric prospective study, in conformity with the ethical guidelines of the 1975 Declaration of Helsinki (and following revisions). All patients submitted to liver resection for HCC were enrolled in 1 year. Exclusion criteria included: the execution of local ablation therapies prior to surgery, final histological diagnosis other than HCC, presence of positive surgical margins (R1), and age < 18 years. Collected clinical data included (see also Table 1): patients’ age and gender, presence of cirrhosis, etiology of liver disease (when known), α-fetoprotein (ng/mL) before surgery, days of hospitalization, days of intensive care unit (ICU) stay, kind of surgery performed (wedge versus segmentectomy, laparotomy versus laparoscopy), clamping minutes (if performed) and transfusion. At least 1 year of follow-up was required; local or distant tumor recurrence was chosen as event, and disease-free survival (DFS) as the study end-point. No additional systemic or local therapies were performed after surgical resection.
Histopathological variables
Surgical specimens from liver resections were sent to the Pathology Unit, where they were sampled according to the routine protocols. Samples were fixed in formalin, embedded in paraffin (FFPE), and routinely processed. For each case, one representative FFPE block was chosen, and sections were cut for the evaluation of the histopathological variables at Haematoxylin–Eosin and for DNA extraction for next-generation sequencing (NGS).
The following histopathological data were collected (Table 1):
-
Tumor dimensions, assessed during the macroscopical examination (in cm).
-
Tumor grade according to Edmondson and Steiner [16] (Grade from 1 to 4) and WHO [17] (good, moderate, and poor differentiation).
-
Tumor architecture, assessed as microtrabecular-acinar, macrotrabecular, or solid: for statistical purposes, and according to our previous data, architecture was also divided in “good architecture”, i.e. microtrabecular and acinar, and “bad architecture”, i.e. when areas of macrotrabecular and/or solid architecture were seen. According to the WHO guidelines, no specific cut-offs for the extension of “bad” areas were applied [17].
-
Presence of infiltrative margins.
-
Presence of overall microvascular invasion (MVI), and—separately—microscopical portal vascular invasion (MPVI) [5].
-
Association with cirrhosis.
Next-generation sequencing
DNA from FFPE specimens was extracted starting from 2 to 4 subsequent sections of 10 μm, using the QuickExtract FFPE DNA extraction kit (LGC Biosearch Technologies, Berlin, Germany), taking into account the areas of interest identified on the control slide stained with haematoxylin and eosin (H&E) by a pathologist.
DNA was quantified using Qubit dsDNA BR assay kit (Thermo Fisher Scientific, Waltham, MA, USA). NGS was performed using a multi-gene panel that allows the amplification of a total of 330 amplicons (human reference sequence hg19/GRCh37, 21.77 kb), including relevant alterations in CTNNB1, TP53, and TERT promoter, as previously described [15, 18]. Sequencing was performed using the Gene Studio S5Primemachine (Thermo Fisher Scientific, Waltham, MA, USA), and raw data analysis was conducted using the IonReporter tool (version 5.18, Thermo Fisher Scientific) and GoldenHelix GenomeBrowse (https://www.goldenhelix.com/products/GenomeBrowse/index.html).
According to the previously reported publication [19], only variants present in at least 5% of the total number of reads were considered. The Varsome tool (https://varsome.com/, accessed in April 2023) [20] was used to evaluate the pathogenicity of each variant.
Statistical analysis
Statistical analysis was performed by means of SPSS® software for Windows, ver. 20. Data are reported as means ± standard deviations, frequencies, and percentages. The chi-square test was used to correlate variables. Multivariate Cox regression analysis was used to assess disease-free survival, using all the clinical and pathological variables listed in the “Materials and methods” section, as well as in Table 1. Univariate analyses were carried out by means of log-rank analysis and the Kaplan–Meier curve. A receiver operator characteristics (ROC) curve was built to assess the best cut-off value for tumor dimensions. A p-value ≤ 0.05 was used to exclude the null hypothesis.
Results
Clinical data and follow-up
Sixty-seven patients satisfied the inclusion criteria, 51 (76.1%) males and 16 (23.9%) females, with a mean age at surgery of 67.8 ± 9.8 years (range 43–85 years). The baseline clinical-pathological characteristics are summarized in Table 1. Thirty (44.8%) patients were cirrhotic; a history of HCV infection was recorded in 23 (34.3%), HBV infection in 8 (11.9%), and NASH in 14 (20.9%). Mean α-fetoprotein before surgery was 7322.09 ng/mL, with a very wide range (1.6–250,753 ng/mL); mean hospital stay was 14.7 ± 10.5 days, mean ICU stay was 1.6 ± 1.5 days. Wedge resection was performed in 60 (89.6%) cases, by laparotomy in 62 (92.5%); mean clamping time was 21.7 ± 31.2 min (range 0–193 min), transfusions were needed in 8 (11.9%) cases.
After a mean follow-up of 445 ± 481 days, 13 (19.4%) patients experienced HCC recurrence, intrahepatic in 9 cases, extrahepatic in 2 cases (one to the lung, one to abdominal lymph nodes), and both in 2; the mean recurrence time was 240 ± 249 days (range 42–900 days).
Histopathological data and mutations
At histopathological analysis, the mean tumor dimension was 5.4 ± 4.2 cm (range 1–17 cm). Only one HCC (1.5%) was grade 1 according to Edmondson (i.e. well-differentiated/G1 according to WHO), 15 (22.4%) were grade 2, 32 (47.8%) were grade 3, and 19 (28.4%) were grade 4 (i.e. poorly differentiated/G3 according to WHO).
As far as tumor architecture is concerned, 32 (47.8%) cases showed a “good architecture”, i.e. microtrabecular and/or acinar, while 35 (52.2%) showed “bad architecture”, defined as areas of macrotrabecular or solid architecture; 4 of these cases were of the macrotrabecular massive subtype [21]. Infiltrative margins were observed in 34 (50.7%) cases.
MVI was present in 55 (82.1%) cases: 24 was of the “conventional” capillary type, while 31 (46.3% of the total) were classified as MPVI.
Next-generation sequencing
The most frequent mutations in our series were TERT promoter (n = 41, 61.2%), TP53 (n = 18, 26.9%), and CTNNB1 (n = 17, 25.4%), with incidences comparable with what was reported in the literature. Concomitant mutations of TERT promoter and TP53 were observed in 11 (16.4%) cases, concomitant mutations of TERT and CTNNB1 in 13 (19.4%).
The incidences of the most frequent mutations of the three genes are summarized in detail in Table 2. TP53 mutations characterized the HCC with worse morphological characteristics since it correlated with macrotrabecular/solid architecture (p = 0.043, chi-square test) and high Edmondson’s grade (p = 0.046). No correlations were found among TERT and CTNNB1 mutations and histopathology (data not shown), but among the clinical variables HCV infection correlated with TERT mutation: 18 out of 23 (78.3%) HCV-positive cases were mutated (p = 0.033, chi-square test, see also Supplementary Table 1).
A combined histopathological-genetic algorithm predictive of HCC recurrence after resection
The influence of clinical variables towards DFS was analyzed to avoid biases: the clinical variable predictive of HCC recurrence was serum α-fetoprotein (p = 0.003, log-rank analysis), as already described in the literature [22]. At any chance, no correlations were found between the clinical variables (including α-fetoprotein) and the molecular biology results. The correlations among the main study variables are summarized in Supplementary Table 1.
Among the histopathological and molecular variables, three correlated with disease-free survival at univariate analysis (Fig. 1): TERT promoter mutation, MPVI, and tumor dimensions. In particular, 11 out of 41 (26.8%) TERT-mutated HCC experienced recurrence, versus 2 out of 26 (7.7%) not mutated cases (p = 0.049; OR = 4.4; 95%CI 0.9–21.8). Nine out of 31 (29.0%) HCC with MPVI experienced recurrence, versus 4 out of 36 (11.1%) HCC without MPVI (p = 0.062; OR = 3.3; 95%CI 0.9–11.9). Concerning tumor dimensions, the ROC curve built to assess the sensitivity and specificity towards HCC recurrence showed an AUC of 0.675: taking 4.5 cm as the cut-off value (which is very close to the 5-cm defining the stage pT3) [23], we found 69% sensitivity and 62% specificity. In particular, 9 out of the 29 (31.0%) HCC ≥ cm 4.5 in dimensions experienced recurrence, versus 4 out of 37 HCC < 4.5 cm (p = 0.041; OR = 3.7; 95%CI 1.0–13.7).
The univariate analyses and the survival curves concerning the other pathological and genetic variables are represented in Supplementary Fig. 1.
The multivariate Cox regression analysis confirmed the correlation of the three variables with DFS (Fig. 2):
-
Tumor dimensions (p = 0.040, log-rank analysis; Exp(B) 1.13)
-
MPVI (p = 0.010; Exp(B) 36.29)
-
TERT promoter mutation (p = 0.034; Exp(B) 6.95).
On the left, a not recurrent case from our series: (a, b) at Haematoxylin–Eosin stain, it is an Edmondson’s grade 2 HCC, with microtrabecular and acinar architecture, no MPVI and (c) wild-type TERT. On the right, a recurrent case: (d, e) a macrotrabecular-massive Edmondson’s grade 3 HCC, with MPVI and (f) characterized by the TERT c.-124C > T mutation
The combination of these variables tended to worsen the overall DFS, and the concomitant occurrence of these three variables, i.e. TERT mutation, MPVI, and dimension more than 4.5 cm was present in 7 cases, among which 5 recurrence cases were recorded (p = 0.002; OR = 15.94; 95%CI 2.6–96.5), all in a relatively short time (Fig. 1).
Discussion
In today’s clinical practice, the pathologist can provide limited information to the surgical team after liver resection for HCC, especially concerning the prediction of DFS. The occurrence of MVI is still considered the most important prognosis predictor [3, 4], while recently the new WHO classification identified some HCC subtypes with worse prognosis, in particular, the massive macrotrabecular subtype, but providing few indications on the specific risk [17]. The application of molecular biology in HCC is still limited to research, with some attempts to reach a “molecular classification” for HCC [10, 13]. Our results showed that the synergic use of histopathological variables and molecular biology, feasible in most tertiary referral centers nowadays, can boost the prognostic value of post-surgical HCC analysis. Particularly, three variables—tumor dimensions, MPVI, and TERT mutation—were shown to be strongly predictive of post-surgical tumor recurrence in our prospective cohort of patients, on both multivariate and univariate analyses, and the combinations among these variables were even stronger (Fig. 3). To our knowledge, this is the first description of the synergic role of these histological and molecular features in resected HCC. Albeit none of these three variables should be a surprise, since they were already described to play a role in HCC biological behavior, they were always studied as independent risk factors, not combined. Other “classic” histological risk factors, such as Edmondson’s grade, architecture, margins, and cirrhosis showed different survival curves, but without reaching statistical significance (Supplementary Fig. 1): a possible explanation is that our study focuses on resected HCCs. Indeed, in our institution, HCC surgical resection is the first therapeutic choice for large advanced tumors, with compensated liver function. This might explain the relatively high prevalence of risk factors in our cohort.
The tumor dimension variable is not a surprise at all, since it is the main driver of local staging systems and therefore of prognosis: in the recent literature, HCC dimensions > 3 cm were described to be an independent risk factor for tumor recurrence after 1 year from the resection, on a large cohort of cases [23]. On the other hand, the cut-off dimension of 5 cm represents the passage from pathological stage 2 to stage 3 in HCCs according to the American Joint Committee on Cancer (AJCC) [24], as well as the criteria for transplantability according to the original Milan’s criteria [25]. The 4.5-cm cut-off that emerged from our series (very close to 5 cm) strongly confirms the literature findings, in addition to indicating the lack of biases in our cohort.
MVI is a well-known prognostic factor for HCC, as it is for many other malignancies [22]: the reported incidence in resected HCC is very variable, according to the different populations, and surgical settings, and considering the sampling biases during pathological examination as well [2, 3]. The tumor invasion of the portal veins—MPVI—was recently described to be a more significant prognostic factor than the “simple” pericapsular MVI [5]: this finding is of utmost importance, not only for the discovery per se but also because MPVI is a much more reproducible histopathological feature than MVI alone, with a better interobserver and intraobserver agreement. Of note, our multivariate and univariate analyses found out MPVI as one of the three predictors of HCC recurrence after resection.
The mutation for the TERT promoter region represents the last prognostic feature found in our cohort. TERT mutations are very frequent in HCC [10, 11], as confirmed by our series which showed more than 60% mutated cases, but the clinical implications are still unclear. The shortening of the telomere length was observed in chronic liver damage and cirrhosis, with the same mechanisms described for senescence [26]. The accumulation of genetic alterations during chronic damage leads to TERT mutation, with its reactivation and the immortalization of the cell, which is a very early event in hepatocarcinogenesis [27]. Some studies correlated TERT mutation with poorer prognosis in advanced HCC, but notably, these cohorts showed exclusively HBV and/or HCV-induced chronic liver disease [11, 14]. This is partly confirmed by our finding that 78% of HCV-related cases had TERT mutation. However, more than half of TERT-mutated cases had no history of viral infection, proving that viral infection correlates with a higher incidence of TERT mutations, but also that this association is not exclusive (see also Supplementary Table 1).
The main limitation of this study is due to the sample size. While it is true that the cohort of samples can be increased in future studies, it should be considered that our results showed that the predictive power of the recurrence event increases from 61% using “traditional” predictive markers (i.e. dimensions and MPVI), to 85% using TERT mutations. With this post hoc evaluation, we calculated a study power of 95%.
In conclusion, none of the described prognostic parameters should represent a novelty for surgeons and clinicians, but our results show that NGS analysis in resected HCC could not only be used for future therapeutic options but should be integrated with histopathological analysis in order to predict the risk of tumor recurrence after surgical resection. Indeed, in resected patients, TERT mutation is among the strongest predictors of tumor recurrence, together with tumor dimensions (i.e. pathological stage) and the occurrence of portal microvascular invasion, which should always be described separately from the classic MVI in the histopathological report.
Data Availability
Data available within the article or its supplementary materials.
References
European Association for the Study of the Liver (2018) EASL clinical practice guidelines: management of hepatocellular carcinoma. J Hepatol 69:182–236
Nevola R, Ruocco R, Criscuolo L et al (2023) Predictors of early and late hepatocellular carcinoma recurrence. World J Gastroenterol 29:1243–1260
Imamura H, Matsuyama Y, Tanaka E et al (2003) Risk factors contributing to early and late phase intrahepatic recurrence of hepatocellular carcinoma after hepatectomy. J Hepatol 38:200–207
Zhang X, Li J, Shen F et al (2018) Significance of presence of microvascular invasion in specimens obtained after surgical treatment of hepatocellular carcinoma. J Gastroenterol Hepatol 33:347–354
Kang I, Jang M, Lee JG et al (2021) Subclassification of microscopic vascular invasion in hepatocellular carcinoma. Ann Surg 274:e1170–e1178
Vasuri F, Fittipaldi S, De Pace V et al (2018) Tissue miRNA 483–3p expression predicts tumor recurrence after surgical resection in histologically advanced hepatocellular carcinomas. Oncotarget 9:17895–17905
Vasuri F, Visani M, Acquaviva G et al (2018) Role of microRNAs in the main molecular pathways of hepatocellular carcinoma. World J Gastroenterol 24:2647–2660
Ng PKS, Lau CPY, Lam EKY et al (2018) Hypermethylation of NF-κB-activating protein-like (NKAPL) promoter in hepatocellular carcinoma suppresses its expression and predicts a poor prognosis. Dig Dis Sci 63:676–686
Yu MC, Lee CW, Lin CH et al (2020) Differential hypermethylation of the VTRNA2-1 promoter in hepatocellular carcinoma as a prognostic factor: Tumor marker prognostic study. Int J Surg 79:282–289
Maloberti T, De Leo A, Sanza V et al (2022) Correlation of molecular alterations with pathological features in hepatocellular carcinoma: literature review and experience of an Italian center. World J Gastroenterol 28:2854–2866
Pezzuto F, Izzo F, De Luca P et al (2021) Clinical significance of telomerase reverse-transcriptase promoter mutations in hepatocellular carcinoma. Cancers (Basel) 13:3771
Lee JS (2015) The mutational landscape of hepatocellular carcinoma. Clin Mol Hepatol 21:220–229
Calderaro J, Couchy G, Imbeaud S et al (2017) Histological subtypes of hepatocellular carcinoma are related to gene mutations and molecular tumour classification. J Hepatol 67:727–738
Oh BK, Kim H, Park YN et al (2008) High telomerase activity and long telomeres in advanced hepatocellular carcinomas with poor prognosis. Lab Invest 88:144–152
Chillotti S, Maloberti T, Degiovanni A et al (2023) Hepatocellular carcinomas with concomitant mutations of TERT, TP53, and CTNNB1: is there a role for artificial intelligence? Crit Rev Oncog 28:31–35
Edmondson HA, Steiner PE (1954) Primary carcinoma of the liver: a study of 100 cases among 48,900 necropsies. Cancer 7:462–503
WHO Classification of Tumours - Digestive System Tumours, 5th edn. IARC: Lyon
Malvi D, Vasuri F, Maloberti T et al (2022) Characterization of pancreatic ductal adenocarcinoma using a next-generationsequencing custom-designed multigene panel. Diagnostics (Basel) 12:1058
De Biase D, Acquaviva G, Visani M et al (2020) Molecular diagnostic of solid tumor using a next generation sequencing custom-designed multi-gene panel. Diagnostics 10:250
Kopanos C, Tsiolkas V, Kouris A et al (2019) VarSome: the human genomic variant search engine. Bioinformatics 35:1978–1980
Vasuri F, Fittipaldi S, Giunchi F et al (2016) Facing the enigma of the vascular network in hepatocellular carcinomas in cirrhotic and non-cirrhotic livers. J Clin Pathol 69:102–108
Costentin C, Audureau E, Park YN, et al (2023) ERS: a simple scoring system to predict early recurrence after surgical resection for hepatocellular carcinoma. Liver Int. https://doi.org/10.1111/liv.15683
Amin MB, Edge SB, Greene FL et al (2017) American Joint Committee on Cancer Manual (AJCC), 8th ed. New York: Springer
Jung SM, Kim JM, Choi GS et al (2019) Characteristics of early recurrence after curative liver resection for solitary hepatocellular carcinoma. J Gastrointest Surg 23:304–311
Mazzaferro V, Regalia E, Doci R et al (1996) Liver transplantation for the treatment of small hepatocellular carcinomas in patients with cirrhosis. N Engl J Med 334:693–699
Kitada T, Seki S, Kawakita N et al (1995) Telomere shortening in chronic liver diseases. Biochem Biophys Res Commun 211:33–39
Quaas A, Oldopp T, Tharun L et al (2014) Frequency of TERT promoter mutations in primary tumors of the liver. Virchows Arch 465:673–677
Funding
Open access funding provided by Alma Mater Studiorum - Università di Bologna within the CRUI-CARE Agreement. This work was partly funded by Fondazione Cassa dei Risparmi di Bologna (Carisbo), Bando Ricerca Medica e Alta Tecnologia, grant Nr. 2021.0144, to Francesco Vasuri, and partly funded by the Italian Ministry of Health, RC-000483/22.
Author information
Authors and Affiliations
Contributions
F.V. performed study concept and design and wrote the paper; S.C., T.M. G.G. and E.A. acquired and analyzed data and provided technical support; M.C. and M.R. provided data interpretation and revised the manuscript; D.d.B. and A.D. performed study concept, analyzed data and revised the manuscript. All authors read and approved the final paper.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Below is the link to the electronic supplementary material.
428_2024_3791_MOESM1_ESM.tif
Supplementary information Suppl. Figure 1. Kaplan-Meier curves of disease-free survival according to the clinical, pathological, and molecular variables which did not enter the multivariate analysis. Other variables (such as tumor grade, architecture, and TP53 mutations) show different curves, but without statistical significance (TIF 2374 KB)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Vasuri, F., Chillotti, S., Maloberti, T. et al. Beyond histology: A tissue algorithm predictive of post-surgical recurrence in hepatocellular carcinomas, including TERT promoter mutation. Virchows Arch (2024). https://doi.org/10.1007/s00428-024-03791-y
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00428-024-03791-y