Abstract
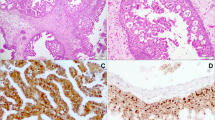
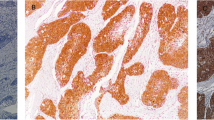
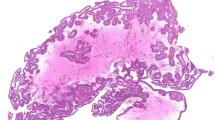
The aim of this study was to investigate the role of human papillomavirus (HPV) in sinonasal inverted papilloma (SIP) and sinonasal oncocytic papilloma (SOP) from a single institution and whether p16 can serve as a surrogate marker for HPV infection. This study included 49 subjects with SIP and 36 subjects with SOP. Formalin-fixed paraffin-embedded tissues were used to extract genomic DNA, and HPV detection was performed by utilizing a valid nested polymerase chain reaction approach that can detect all known HPV subtypes. Immunohistochemistry was used to evaluate the expression of p16 in all tumor sections. The presence of HPV DNA was found in 6.1% (3/49) of the SIP patients and 11.1% (4/36) of the SOP patients. All identified HPV subtypes in SIP were high-risk HPV, including HPV-16 (two patients) and HPV-58 (one patient). Regarding SOP, there were three patients positive for HPV-16 and one with low-risk HPV (type 6). In total, 11/49 (22.4%) SIP lesions and 10/36 (27.8%) SOP lesions were considered p16 positive, with p16 staining in more than 70% of tumor cells. There was only one SIP and one SOP that were positive for both HPV (high-risk HPV type 16) and p16 staining. HPV does not play an etiologic role in inverted papilloma or oncocytic papilloma of the sinonasal region. p16 immunostaining should not be used as a surrogate marker to evaluate the HPV infection status in these lesions.


Similar content being viewed by others
References
El-Naggar AK, JKC C, Grandis JR, Takata T, Slootweg PJ (2017) WHO classification of head and neck tumours. IARC, Lyon
Thompson LDR, Franchi A (2018) New tumor entities in the 4th edition of the World Health Organization classification of head and neck tumors: nasal cavity, paranasal sinuses and skull base. Virchows Arch 472(3):315–330
Bishop JA (2017) OSPs and ESPs and ISPs, Oh My! An update on sinonasal (Schneiderian) papillomas. Head Neck Pathol 11(3):269–277
Udager AM et al (2015) High-frequency targetable EGFR mutations in sinonasal squamous cell carcinomas arising from inverted sinonasal papilloma. Cancer Res 75(13):2600–2606
Wang H et al (2019) EGFR and KRAS mutations in Chinese patients with sinonasal inverted papilloma and oncocytic papilloma. Histopathology
Wang X, Huang X, Zhang Y (2018) Involvement of human papillomaviruses in cervical cancer. Front Microbiol 9:2896
Zhao RW, Guo ZQ, Zhang RX (2016) Human papillomavirus infection and the malignant transformation of sinonasal inverted papilloma: a meta-analysis. J Clin Virol 79:36–43
Syrjanen KJ (2003) HPV infections in benign and malignant sinonasal lesions. J Clin Pathol 56(3):174–181
Mohajeri S et al (2018) Human papillomavirus: an unlikely etiologic factor in sinonasal inverted papilloma. Laryngoscope 128(11):2443–2447
Rooper LM, Bishop JA, Westra WH (2017) Transcriptionally active high-risk human papillomavirus is not a common etiologic agent in the malignant transformation of inverted Schneiderian papillomas. Head Neck Pathol 11(3):346–353
Sahnane N et al (2018) Comprehensive analysis of HPV infection, EGFR exon 20 mutations and LINE1 hypomethylation as risk factors for malignant transformation of sinonasal inverted papilloma to squamous cell carcinoma. Int J Cancer
Vorasubin N et al (2013) Schneiderian papillomas: comparative review of exophytic, oncocytic, and inverted types. Am J Rhinol Allergy 27(4):287–292
Syrjanen K, Syrjanen S (2013) Detection of human papillomavirus in sinonasal papillomas: systematic review and meta-analysis. Laryngoscope 123(1):181–192
Lin H, Lin D, Xiong XS (2016) Roles of human papillomavirus infection and stathmin in the pathogenesis of sinonasal inverted papilloma. Head Neck 38(2):220–224
Liu Y et al (2017) Role of the Akt/mTOR signaling pathway in human papillomavirus-associated nasal and sinonasal inverted papilloma. Acta Biochim Biophys Sin Shanghai 49(12):1067–1074
Sham CL et al (2012) Prevalence of human papillomavirus, Epstein-Barr virus, p21, and p53 expression in sinonasal inverted papilloma, nasal polyp, and hypertrophied turbinate in Hong Kong patients. Head Neck 34(4):520–533
Krouse JH (2000) Development of a staging system for inverted papilloma. Laryngoscope 110(6):965–968
Fuessel Haws AL et al (2004) Nested PCR with the PGMY09/11 and GP5(+)/6(+) primer sets improves detection of HPV DNA in cervical samples. J Virol Methods 122(1):87–93
Lewis JS Jr et al (2018) Human papillomavirus testing in head and neck carcinomas: guideline from the College of American Pathologists. Arch Pathol Lab Med 142(5):559–597
Suh JD et al (2013) COX-(2) overexpression in sinonasal inverted papilloma. Int Forum Allergy Rhinol 3(12):997–1000
Byun JY et al (2014) Overexpression of angiomotin in sinonasal inverted papilloma. Int Forum Allergy Rhinol 4(6):512–516
Hasegawa M et al (2012) Human papillomavirus load and physical status in sinonasal inverted papilloma and squamous cell carcinoma. Rhinology 50(1):87–94
Jenko K et al (2011) In inverted papillomas HPV more likely represents incidental colonization than an etiological factor. Virchows Arch 459(5):529–538
Udager AM et al (2018) Human papillomavirus (HPV) and somatic EGFR mutations are essential, mutually exclusive oncogenic mechanisms for inverted sinonasal papillomas and associated sinonasal squamous cell carcinomas. Ann Oncol 29(2):466–471
Doxtader EE, Katzenstein AL (2012) The relationship between p16 expression and high-risk human papillomavirus infection in squamous cell carcinomas from sites other than uterine cervix: a study of 137 cases. Hum Pathol 43(3):327–332
Ang KK, Sturgis EM (2012) Human papillomavirus as a marker of the natural history and response to therapy of head and neck squamous cell carcinoma. Semin Radiat Oncol 22(2):128–142
Acknowledgments
This work was supported by Natural Science Foundation of China (No. 81371077) and Natural Science Foundation of Shanghai (16ZR1405000). The authors would like to thank Jun Wei and Qiang Wang from Shanghai ERA Biotech for their help for the technical issues.
Author information
Authors and Affiliations
Contributions
Huan Wang, Changwen Zhai, and Juan Liu performed the experiments and measurements, Huan Wang and Jingjing Wang processed the experimental data, performed the analysis, drafted the manuscript, and designed the figures. Dehui Wang aided in interpreting the results and worked on the manuscript. Xicai Sun and Li Hu were involved in planning and supervising the work and also the final approval of the manuscript. All authors discussed the results and commented on the manuscript.
Corresponding authors
Ethics declarations
Ethical approval
All procedures followed were in accordance with the ethical standards of the Research and Ethical Committee of EENT Hospital affiliated with Fudan University and with the Helsinki Declaration of 1975 (in its most recently amended version).
Informed consent
Informed consent was obtained from all patients included in the study.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Quality in Pathology
Rights and permissions
About this article
Cite this article
Wang, H., Zhai, C., Liu, J. et al. Low prevalence of human papillomavirus infection in sinonasal inverted papilloma and oncocytic papilloma. Virchows Arch 476, 577–583 (2020). https://doi.org/10.1007/s00428-019-02717-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00428-019-02717-3