Abstract
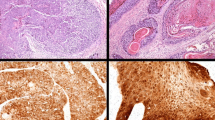
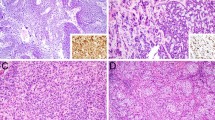
The sinonasal tract is considered a second hotspot for human papillomavirus (HPV)-related tumors in the head and neck, with HPV being identified in up to 62% of squamous cell carcinomas (SCCs) and 38% of papillomas. There is limited data from geographical regions with low prevalence of high-risk (HR)-HPV on the association of HR-HPV in sinonasal neoplasms and on utility of p16 as a surrogate marker. p16 immunohistochemistry, HR-HPV mRNA ISH and quantitative real-time PCR (qPCR) were performed on a retrospective cohort of sinonasal papillomas and SCCs. KRAS mutation analysis was done in oncocytic papillomas. p16 positivity was present in 22/142 cases (15.5%) including eight inverted papillomas, one oncocytic papilloma (OP), and 13 SCC. Among these, mRNA ISH showed HR-HPV in the OP and two SCC, while another SCC was found to harbour HPV18 by qPCR. Two HPV-associated SCCs had foci of OP. mRNA ISH was negative in all p16 negative cases. p16 immunohistochemistry showed 68% concordance with mRNA ISH, and had sensitivity and negative predictive value of 100%; specificity was 67%, and positive predictive value was 14.3%. Association with HR-HPV in sinonasal papillomas and SCC is rare, and may be seen in cases demonstrating oncocytic morphology. p16 immunohistochemistry has low specificity and positive predictive value in low-prevalence populations; thus, reflex direct HR-HPV testing should be performed in p16 immunopositive cases. This two-step approach is viable in resource-limited settings, as the proportion of p16 positive cases is small.



Similar content being viewed by others
References
Lawson W, Schlecht NF, Brandwein-Gensler M (2008) The role of the human papillomavirus in the pathogenesis of Schneiderian inverted papillomas: an analytic overview of the evidence. Head Neck Pathol 2:49–59
Lewis JS Jr, Westra WH, Thompson LD et al (2014) The sinonasal tract: another potential "hot spot" for carcinomas with transcriptionally-active human papillomavirus. Head Neck Pathol 8:241–249
Elgart K, Faden DL (2020) Sinonasal Squamous Cell Carcinoma: Etiology, Pathogenesis, and the Role of Human Papilloma Virus. Curr Otorhinolaryngol Rep 8:111–119
Allen CT, Lewis JS Jr, El-Mofty SK, Haughey BH, Nussenbaum B (2010) Human papillomavirus and oropharynx cancer: biology, detection and clinical implications. Laryngoscope 120:1756–1772
Adelstein DJ, Ridge JA, Gillison ML et al (2008) Head and neck squamous cell cancer and the human papilloma- virus: summary of a National Cancer Institute State of the Science Meeting, November 9-10, 2008, Washington D.C. Head Neck 31:1393–1422
El-Mofty SK, Lu DW (2005) Prevalence of high-risk human papillomavirus DNA in nonkeratinizing (cylindrical cell) carcinoma of the sinonasal tract: a distinct clinicopathologic and molecular disease entity. Am J Surg Pathol 29:1367–1372
Bishop JA, Guo TW, Smith DF et al (2013) Human papillomavirus-related carcinomas of the sinonasal tract. Am J Surg Pathol 37:185–192
Larque AB, Hakim S, Ordi J et al (2014) High-risk human papillomavirus is transcriptionally active in a subset of sinonasal squamous cell carcinomas. Mod Pathol 27:343–351
Rooper LM, Bishop JA, Westra WH (2017) Transcriptionally Active High-Risk Human Papillomavirus is Not a Common Etiologic Agent in the Malignant Transformation of Inverted Schneiderian Papillomas. Head Neck Pathol 11:346–353
Chowdhury N, Alvi S, Kimura K et al (2017) Outcomes of HPV-related nasal squamous cell carcinoma. Laryngoscope 127:1600–1603
Jiromaru R, Yamamoto H, Yasumatsu R et al (2020) HPV-related Sinonasal Carcinoma: Clinicopathologic Features, Diagnostic Utility of p16 and Rb Immunohistochemistry, and EGFR Copy Number Alteration. Am J Surg Pathol 44:305–315
Syrjänen KJ (2003) HPV infections in benign and malignant sinonasal lesions. J Clin Pathol 56:174–181. https://doi.org/10.1136/jcp.56.3.174
Syrjanen S, Happonen RP, Virolainen E et al (1987) Detection of human papillomavirus (HPV) structural antigens and DNA types in inverted papillomas and squamous cell carcinomas of the nasal cavities and paranasal sinuses. Acta Otolaryngol 104:334–341
Lewis JS Jr, Beadle B, Bishop JA et al (2018) Human papillomavirus testing in head and neck carcinomas: guideline from the College of American Pathologists. Arch Pathol Lab Med 142:559–597
Bahl A, Kumar P, Dar L et al (2014) Prevalence and trends of human papillomavirus in oropharyngeal cancer in a predominantly north Indian population. Head Neck 36:505–510
Lewis JS Jr (2016) Sinonasal Squamous Cell Carcinoma: A Review with Emphasis on Emerging Histologic Subtypes and the Role of Human Papillomavirus. Head Neck Pathol 10:60–67
Antony VM, Kakkar A, Sikka K et al (2020) p16 Immunoexpression in sinonasal and nasopharyngeal adenoid cystic carcinomas: a potential pitfall in ruling out HPV-related multiphenotypic sinonasal carcinoma. Histopathol 77:989–993
Kim KY, Lewis JS Jr, Chen Z (2018) Current status of clinical testing for human papillomavirus in oropharyngeal squamous cell carcinoma. J Pathol Clin Res 4:213–226
Avasthi A, Kaur R, Prakash O, Banerjee A, Kumar L, Kulhara P (2008) Sexual behavior of married young women: a preliminary study from north India. Indian J Community Med 33:163–167. https://doi.org/10.4103/0970-0218.39677
Alos L, Moyano S, Nadal A et al (2009) Human papillomaviruses are identified in a subgroup of sinonasal squamous cell carcinomas with favorable outcome. Cancer 115:2701–2709. https://doi.org/10.1002/cncr.24309
Kilic S, Kilic SS, Kim ES et al (2017) Significance of human papillomavirus positivity in sinonasal squamous cell carcinoma. Int Forum Allergy Rhinol 7:980–989. https://doi.org/10.1002/alr.21996
Oliver JR, Lieberman SM, Tam MM et al (2020) Human papillomavirus and survival of patients with sinonasal squamous cell carcinoma. Cancer 126:1413–1423. https://doi.org/10.1002/cncr.32679
Markovic ES, Marqueen KE, Sindhu KK et al (2020) The prognostic significance of human papilloma virus in sinonasal squamous cell carcinoma. Laryngoscope Investig Otolaryngol 5:1070–1078
Thavaraj S (2016) Human papillomavirus-associated neoplasms of the sinonasal tract and nasopharynx. Semin Diagn Pathol 33:104–111
Lewis JS Jr (2020) Human Papillomavirus Testing in Head and Neck Squamous Cell Carcinoma in 2020: Where Are We Now and Where Are We Going? Head Neck Pathol 14:321–329
Kapadia SB, Barnes L, Pelzman K, Mirani N, Heffner DK, Bedetti C (1993) Carcinoma ex oncocytic Schneiderian (cylindrical cell) papilloma. Am J Otolaryngol 14:332–338
Kaufman MR, Brandwein MS, Lawson W (2002) Sinonasal papillomas: clinicopathologic review of 40 patients with inverted and oncocytic schneiderian papillomas. Laryngoscope 112:1372–1377
Stoddard DG Jr, Keeney MG, Gao G, Smith DI, García JJ, O'Brien EK (2015) Transcriptional activity of HPV in inverted papilloma demonstrated by in situ hybridization for E6/E7 mRNA. Otolaryngol Head Neck Surg 152:752–758
Syrjänen K, Syrjänen S (2013) Detection of human papillomavirus in sinonasal carcinoma: Systematic review and meta-analysis. Hum Pathol 44:983–991
Laco J, Sieglová K, Vošmiková H et al (2015) The presence of high-risk human papillomavirus (HPV) E6/E7 mRNA transcripts in a subset of sinonasal carcinomas is evidence of involvement of HPV in its etiopathogenesis. Virchows Arch 467:405–415
Udager AM, McHugh JB, Goudsmit CM et al (2018) Human papillomavirus (HPV) and somatic EGFR mutations are essential, mutually exclusive oncogenic mechanisms for inverted sinonasal papillomas and associated sinonasal squamous cell carcinomas. Ann Oncol 29:466–471
Sahnane N, Ottini G, Turri-Zanoni M et al (2019) Comprehensive analysis of HPV infection, EGFR exon 20 mutations and LINE1 hypomethylation as risk factors for malignant transformation of sinonasal-inverted papilloma to squamous cell carcinoma. Int J Cancer 144:1313–1320
Brown NA, Plouffe KR, Yilmaz O, Weindorf SC, Betz BL, Carey TE et al (2021) TP53 mutations and CDKN2A mutations/deletions are highly recurrent molecular alterations in the malignant progression of sinonasal papillomas. Mod Pathol 34:1133–1142
Gheit T, Vaccarella S, Schmitt M et al (2009) Prevalence of human papillomavirus types in cervical and oral cancers in central India. Vaccine 27:636–639. https://doi.org/10.1016/j.vaccine.2008.11.041
Shah A, Malik A, Garg A, Mair M, Nair S, Chaturvedi P (2017) Oral sex and human papilloma virus-related head and neck squamous cell cancer: a review of the literature. Postgrad Med J 93:704–709
Hongo T, Yamamoto H, Tanabe M et al (2022) High-risk HPV-related Squamous Cell Carcinoma in the Conjunctiva and Lacrimal sac: Clinicopathologic Characteristics and Diagnostic Utility of p16 and Rb Immunohistochemistry. Am J Surg Pathol 46:977–987
Vor der Holte AP, Fangk I, Glombitza S, Wilkens L, Welkoborsky HJ (2020) Identification of Rare and Common HPV Genotypes in Sinonasal Papillomas. Head Neck Pathol 14:936–943
Vor der Holte AP, Fangk I, Glombitza S, Wilkens L, Welkoborsky HJ (2020) Prognostic factors and risk factors for development and recurrence of sinonasal papillomas: potential role of different HPV subtypes. Eur Arch Otorhinolaryngol 277:767–775
Udager AM, McHugh JB, Betz BL et al (2016) Activating KRAS mutations are characteristic of oncocytic sinonasal papilloma and associated sinonasal squamous cell carcinoma. J Pathol 239:394–398
Wang H, Zhai C, Liu J et al (2020) Low prevalence of human papillomavirus infection in sinonasal inverted papilloma and oncocytic papilloma. Virchows Arch 476:577–583
Hyams VJ (1971) Papillomas of the nasal cavity and paranasal sinuses. A clinicopathological study of 315 cases. Ann Otol Rhinol Laryngol 80:192–206
Barnes L, Bedetti C (1984) Oncocytic Schneiderian papilloma: a reappraisal of cylindrical cell papilloma of the sinonasal tract. Hum Pathol 15:344–351
Ward BE, Fechner RE, Mills SE (1990) Carcinoma arising in oncocytic Schneiderian papilloma. Am J Surg Pathol 14:364–369
Yang YJ, Abraham JL (1997) Undifferentiated carcinoma arising in oncocytic Schneiderian (cylindrical cell) papilloma. J Oral Maxillofac Surg 55:289–294
Maitra A, Baskin LB, Lee EL (2001) Malignancies arising in oncocytic schneiderian papillomas: a report of 2 cases and review of the literature. Arch Pathol Lab Med 125:1365–1367
Karligkiotis A, Bignami M, Terranova P et al (2014) Oncocytic Schneiderian papillomas: Clinical behavior and outcomes of the endoscopic endonasal approach in 33 cases. Head Neck 36:624–630
Zhang L, Hu C, Zheng X et al (2018) Oncocytic Schneiderian papilloma-associated adenocarcinoma and KRAS mutation: A case report. Med 97:e11025
Nudell J, Chiosea S, Thompson LD (2014) Carcinoma ex-Schneiderian papilloma (malignant transformation): a clinicopathologic and immunophenotypic study of 20 cases combined with a comprehensive review of the literature. Head Neck Pathol 8:269–286
Bishop JA, Lewis JS Jr, Rocco JW, Faquin WC (2015) HPV-related squamous cell carcinoma of the head and neck: An update on testing in routine pathology practice. Semin Diagn Pathol 32:344–351
Doxtader EE, Katzenstein AL (2012) The relationship between p16 expression and high-risk human papillomavirus infection in squamous cell carcinomas from sites other than uterine cervix: a study of 137 cases. Hum Pathol 43:327–332
Shinn JR, Davis SJ, Lang-Kuhs KA et al (2021) Oropharyngeal Squamous Cell Carcinoma With Discordant p16 and HPV mRNA Results: Incidence and Characterization in a Large, Contemporary United States Cohort. Am J Surg Pathol 45:951–961
Nauta IH, Rietbergen MM, van Bokhoven AAJD et al (2018) Evaluation of the eighth TNM classification on p16-positive oropharyngeal squamous cell carcinomas in the Netherlands and the importance of additional HPV DNA testing. Ann Oncol 29:1273–1279
Funding
This study received funds from Collaborative intramural grant (AC-005), Research Section, All India Institute of Medical Sciences, New Delhi.
Author information
Authors and Affiliations
Contributions
AK: Data acquisition, analysis and interpretation of results, drafting the manuscript; SS, KS, PT, SVS: Data acquisition and analysis; DJ: Conception and design, data acquisition and analysis, final interpretation of results, overall supervision, and critical revision of the manuscript. All authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval
Ethics approval was obtained from the Institute Ethics committee for conducting this study (IEC-608/03.11.2017)
Conflict of Interest
The authors do not have any financial or non-financial interests to declare
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kakkar, A., Satapathy, S., Sikka, K. et al. Evaluation of high-risk human papillomavirus in sinonasal papillomas and squamous cell carcinomas. Virchows Arch 483, 381–392 (2023). https://doi.org/10.1007/s00428-023-03601-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00428-023-03601-x