Abstract
Acidosis is a chemical signature of the tumour microenvironment that challenges intracellular pH homeostasis. The orchestrated activity of acid-base transporters of the solute-linked carrier (SLC) family is critical for removing the end-products of fermentative metabolism (lactate/H+) and maintaining a favourably alkaline cytoplasm. Given the critical role of pH homeostasis in enabling cellular activities, mutations in relevant SLC genes may impact the oncogenic process, emerging as negatively or positively selected, or as driver or passenger mutations. To address this, we performed a pan-cancer analysis of The Cancer Genome Atlas simple nucleotide variation data for acid/base-transporting SLCs (ABT-SLCs). Somatic mutation patterns of monocarboxylate transporters (MCTs) were consistent with their proposed essentiality in facilitating lactate/H+ efflux. Among all cancers, tumours of uterine corpus endometrial cancer carried more ABT-SLC somatic mutations than expected from median tumour mutation burden. Among these, somatic mutations in SLC4A3 had features consistent with meaningful consequences on cellular fitness. Definitive evidence for ABT-SLCs as ‘cancer essential’ or ‘driver genes’ will have to consider microenvironmental context in genomic sequencing because bulk approaches are insensitive to pH heterogeneity within tumours. Moreover, genomic analyses must be validated with phenotypic outcomes (i.e. SLC-carried flux) to appreciate the opportunities for targeting acid-base transport in cancers.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Solute-linked carriers (SLCs) are a superfamily of genes integral to physiological cellular function and wider homeostasis across organ systems. SLCs comprise 66 gene families that code for transporters of ions and solutes across biological membranes [39, 59]. This classification was introduced after a decade of intensive cloning, starting in the 1980s, that assigned genes to measurable fluxes across membranes [38, 45, 70]. There are at least 400 SLC members classed under broad groupings, such as transporters of bicarbonate (or carbonate [52]), monosaccharides, amino acids, and metal cations [39, 59]. SLC function is essential in the context of membrane transport because most ions and many polar solutes cannot freely diffuse across the phospholipid bilayer so require facilitation by proteins. Moreover, some SLCs can support active transport, which is often necessary for cellular homeostasis, substrate sequestration, waste excretion, and trans-epithelial transport. Illustrative of their biological importance, over 100 SLCs have been associated with human genetic disorders [72], and homozygous loss of certain SLCs produces embryonic lethality [84].
The acid/base-transporting SLCs (ABT-SLCs) play a crucial homeostatic role in facilitating the extrusion of acidic products of metabolism (notably lactate/H+) and maintaining a favourable intracellular pH (pHi) by balancing the import and export of H+-equivalents. Thus, ABT-SLCs can be grouped into ‘acid-loaders’ or ‘acid-extruders’, although the net direction of transport will depend on ionic gradients and regulatory cues [60]. In well-perfused normal tissues, extracellular pH (pHe) is tightly clamped at 7.4 by continuous capillary perfusion [11]. In contrast, tumour vasculature is chaotically organised and leaky, resulting in poor acid clearance [71]. pHe measurements in humans by specialised magnetic resonance imaging (MRI) modalities, like Chemical Exchange Saturation Transfer, put the median intra-tumoural pHe of various cancers, including breast cancer, hepatic carcinoma, prostate cancer, and glioma, at 6.8 [11]. Reported values reach as low as 6.3, and it is likely that the spatial resolution of MRI excludes the detection of microscopic pockets of more extreme acidity [11].
ABT-SLCs impinge upon homeostatic processes in cancer cells in three ways. Firstly, protons are a metabolic by-product, in the form of either lactate/H+ produced by fermentation or respiration-generated CO2 (which hydrates to HCO3- and H+) [76]. Whereas CO2 can cross the lipid bilayer of membranes freely, lactate/H+ is poorly permeant without facilitation by SLC16-type proteins. Higher glycolytic rates are typically matched by higher SLC16-dependent membrane permeability to lactate/H+ [74]. This aids in preventing cytoplasmic acidification, which would otherwise exert negative feedback on glycolytic enzymes such as glyceraldehyde 3-phosphate dehydrogenase and phosphofructokinase 1 [61, 81, 83]. Secondly, it is imperative that cancer cells maintain a favourable pHi [60] as biological processes (with the exception of those compartmentalised to organelles of specific pH, like lysosomes or mitochondria) operate optimally around the mildly alkaline pH of 7.2 [60]. Outside the conducive pHi range, cancer cells are unable to engage in aggressive behaviours such as invasion and metastasis [11, 60]. Thirdly, secondary-active ABT-SLCs require considerable energetic input [27], especially considering the demand to maintain a relatively alkaline pHi in an acidic microenvironment (i.e. considerable uphill transport against an electrochemical gradient) [14, 60, 73, 92]. Moreover, many cancers develop from epithelia that transport large and complementary acid-base fluxes across apical and basolateral membranes as part of wider systems-level processes, such as acid secretion by the stomach or bicarbonate secretion by the exocrine pancreas. Such secondary active transport can carry a considerable energetic cost, despite no immediate survival benefit to the epithelial cell. Under finite resources, cancer cells must balance energetic flows to ABT-SLCs against other priorities, such as hyperproliferation [9].
The fundamental link between ABT-SLCs and cancer metabolism begs the question: do changes in acid-base transport influence tumourigenesis in patients? This question is especially pertinent because inhibitors of ABT-SLCs have been mooted as therapeutic targets in cancer [19, 37, 66] and some reached early-phase clinical trials [37]. Direct appraisal of in vivo ABT-SLC flux in human cancers is currently unfeasible. Nonetheless, genomic analysis of human tumours could inform about how ABT-SLCs impact cancer cell fitness in vivo and their ultimate role in intra-tumoural evolution, which arises from the vast genetic and epigenetic heterogeneity among cancer cells [10, 65]. Where somatic mutations in a specific gene augment or impair cancer cell fitness, positive or negative selection, respectively, ensue [56]. A cancer’s landscape of somatic point mutations, insertions, and deletions can be harnessed to interrogate selection events that have occurred over the course of tumourigenesis [6, 7, 28, 50, 56, 90]. Indeed, somatic mutation-based approaches have successfully identified many genes that can drive cancer [6, 7, 28, 50, 56] and processes that are essential for cancer cell survival in human tumours [7, 90]. However, the landscape of somatic mutations in ABT-SLCs across the common types of human cancers is in need of being documented systematically, with the major caveat that it is not intuitive to predict their functional outcomes in terms of transport, i.e. actual phenotype that determines fitness.
Here, we perform a pan-cancer analysis of somatic mutations in ABT-SLCs using human tumour datasets from The Cancer Genome Atlas (TCGA) [16]. In a comparative approach, whereby the mutation status of acid-base transporters is contextualised with that of other cancer-relevant SLC classes [39, 59], we evaluate the role of acid-base transport in intra-tumoural evolution. Specifically, we discuss (i) whether there is evidence that mutations in ABT-SLCs drive cancer; (ii) the essentiality of ABT-SLCs to cancer; and (iii) the degree of redundancy within the pHi regulatory mechanisms of cancer cells.
Pan-cancer analysis of somatic mutations in ABT-SLCs
We subdivided ABT-SLCs into 4 groups based on the type of flux carried: monocarboxylate transporters (MCTs), sodium-hydrogen exchangers (NHEs), sodium-bicarbonate cotransporters (NBCs), and anion exchangers (AEs) [74]. We took a conservative approach and curated ABT-SLCs on the basis of a proven role in acid-base transport across the surface membrane, rather than sequence similarity to known ABT-SLCs [39, 59]. The classification of individual genes, their substrates, and transport type are summarised in Table 1. Under physiological scenarios, NHEs and most NBCs (with the notable exception of SLC4A5 [8]) are predicted to be acid-extruders, AEs are predicted to be acid-loaders, and in fermentive cancer cells, MCTs are predicted to be acid-extruders (Fig. 1a) [12, 74]. Importantly, the direction of transport is a function of numerous microenvironmental conditions, which may differ in tumours, namely: oxygen levels, pH, ATP levels, and lactate [9, 11]. The expression of these SLCs is recognised to be regulated by oncogenic pathways [21], nutrient-sensing mechanisms [60], and gene methylation [33]. Yet, there is little information about their somatic mutations in cancer. Somatic mutations in SLC16A1 [18], SLC16A7 [24, 64], SLC9A2 [91], SLC9A3 [42], SLC9A8 [48], SLC9A9 [31, 85], SLC4A2 [22, 88], SLC4A4 [53], SLC4A7 [34], and SLC4A8 [47] have been reported in human cancers (Table 1). However, their abundance across large pan-cancer cohorts has not been analysed. To address this gap, we downloaded open-access simple nucleotide variation data from all available TCGA projects on the GDC data portal [16] via TCGAbiolinks (R) [23]. The full list of TCGA cohorts included in analyses is denoted in Supplementary Table 1. Maftools (R) was then used to analyse and present the downloaded somatic mutation data [57].
Pan-cancer analysis of simple nucleotide variation in ABT-SLCs. a Schematic of predicted ABT-SLC direction (excluding SLC4A5) at the plasma membrane of fermentive cancer cells under physiological conditions. Created with BioRender.com. b Open-access simple nucleotide variation data for all TCGA projects available for download from the GDC portal via TCGAbiolinks. Oncoplot of somatic mutations in ABT-SLCs. Percentages displayed are the number of samples carrying at least one somatic mutation in the given ABT-SLC normalised to the total number of samples analysed (n=10,549 samples). c Somatic mutation cumulative incidence for SLCs (ranked), highlighting groups of SLCs: all glucose-transporting SLCs, amino acid-transporting SLCs, nucleotide/nucleoside-transporting SLCs, AEs, NHEs, NBCs, and MCTs. The cumulative incidence plot illustrates the distribution of SLCs by grouping across the full range of SLCs, ranked by descending incidence of mutations
Strikingly, 17.58% (1,854/10,549) of tumour samples carried at least one somatic mutation in a gene coding for an ABT-SLC, yet individual ABT-SLC genes were somatically mutated in only 0–2% of tumour samples (Fig. 1b). The majority of mutations changed protein coding sequence (i.e. missense). The most commonly mutated ABT-SLC was SLC9C1, previously reported to be a sperm-specific NHE which, unlike the SLC9A family, is voltage-gated [87]. Overall, MCTs tended to be the least abundantly mutated ABT-SLCs (somatic mutations present in 0–1% of tumour samples), whereas NBCs were collectively some of the most commonly mutated (somatic mutations present in 1–2% of tumour samples).
We next sought to contextualise these findings against other SLC transporters (Fig. 1c) [39, 59]. Glucose uptake by SLCs is required to sustain the high glycolytic rate of cancer cells, a vital source of biosynthetic intermediates for cell proliferation [94]. Amino acids, uptake of which is SLC-mediated, are the building blocks of proteins and precursors to numerous metabolites essential for cellular function, including C1 compounds, nucleotides, glutathione, polyamines, hexosamines, and creatinine [15]. Another important SLC group is the nucleotide/nucleoside transporters which deliver bases of nucleic acids. In order to compare ABT-SLCs against glucose-, amino acid-, or nucleotide/nucleoside-transporting SLCs, we first ranked all somatically mutated SLC genes by descending mutation incidence (Fig. 1c, top). The cumulative incidence of somatic mutations along the SLC ranking was then calculated for each transport group (Fig. 1c, bottom).
In terms of the number of somatic alterations, glucose- and amino acid-transporting SLCs featured uniformly across the range of all SLCs, without enrichment among highly or lowly mutated genes (Fig. 1c). Nucleoside/nucleotide-transporting SLCs tended to have a below-average mutation incidence among SLCs. In terms of ABT-SLCs, NBCs and AEs generally had an above-average mutation incidence among SLCs, whereas MCTs had a below-average incidence (Fig. 1c). These observations indicate that the mutation rates among NBCs and AEs are relatively high among SLCs, whereas mutations in MCTs may be selected negatively. Specifically, the NHEs SLC9C1 and SLC9A2, the NBCs SLC4A10 and SLC4A4, and the AE SLC4A3 ranked among the top 20 somatic SLC mutations most abundantly carried by tumour samples. In fact, SLC9C2 mutations affected the highest proportion of tumour samples out of all SLCs, which is notable because, although it is currently an orphan transporter [59], its sequence is closely related to SLC9C1, the voltage-gated NHE [87]. When contextualised against all SLCs, the relatively high mutation incidence of certain ABT-SLCs warrants further investigation as to whether their mutations have undergone positive selection.
Can mutations in acid-base transporter genes drive cancer?
Cancer driver genes are defined as genes whose mutations increase net cell growth under the specific microenvironmental conditions present in vivo and are estimated to comprise 1–3.9% of somatic mutations [56]. Importantly, cancer driver genes are the basis of targeted anti-cancer therapies. Extrapolating from in vitro findings, it could be speculated that gain-of-function mutations in acid-extruders support cell division by improving pHi homeostasis under intra-tumoural acidosis [4]. Moreover, the germline single nucleotide polymorphism (SNP) in the NBC SLC4A7, rs4973768, is associated with increased lifetime breast cancer risk, putatively due to SLC4A7 overexpression [20, 95]. The germline SNP in the MCT SLC16A7, rs995343, has also been associated with adverse outcomes in colorectal and non-small cell lung cancers (Table 1) [32, 35]. Conversely, loss-of-function mutations in the Na+-coupled secondary active transporters, NBCs and NHEs, could divert ATP towards cell division programmes, particularly in cancers developing from tissues with substantial trans-epithelial solute movement [27]. Thus, there is good reasoning behind testing the notion of ABT-SLCs as cancer driver genes.
It is well-recognised that only few cancer driver genes are mutated in a high percentage of certain cancers [50]. Pertinent examples include BRAF in ~50% of melanomas and PIK3CA in ~25–30% of breast and colorectal cancers [5, 44, 46]. However, most cancer driver genes are mutated at intermediate rates, 2–20% of tumours [50], a threshold that is met by numerous ABT-SLCs pan-cancer (Fig. 1b). Cancer driver genes are typically identified by genomic methods in which two characteristics are assessed [28]: (i) whether their mutation frequency is in excess over background mutation rate and (ii) whether their mutations cluster at genomic loci corresponding to residues that are critical for protein function. These characteristics arise from positive selection as a consequence of the mutation’s survival benefit, relative to non-mutant cancer cells.
Unsurprisingly, we find that the cancer types most likely to carry somatic mutations in ABT-SLCs are known to have the highest background mutation rates (Fig. 2a, abbreviations defined in Supplementary Table 1). These include skin cutaneous melanoma (SKCM) and lung adenocarcinoma (LUAD) or squamous cell carcinoma (LUSC). To identify specific cancers where ABT-SLCs are more likely to be under positive selection, we stratified the proportion of tumour samples carrying at least one ABT-SLC somatic mutation by TCGA cohort, then plotted against the cohort’s median tumour mutation burden with linear model fitting (Fig. 2a). For most cancer types, there was a positive linear relationship between median tumour mutation burden and the proportion of samples carrying mutations in ABT-SLCs. Indeed, it is estimated that 97–98% of somatic mutations in cancer are simply passengers (i.e. not sufficiently advantageous to be positively selected, nor sufficiently deleterious to be negatively selected) [56]. However, some cancer types had an enrichment in ABT-SLC mutations which was not directly proportional to their median tumour mutation burden. These included uterine corpus endometrial carcinoma (UCEC), colon adenocarcinoma (COAD), stomach adenocarcinoma (STAD), cervical squamous cell carcinoma (CESC), and rectal adenocarcinoma (READ) (Fig. 2a, highlighted in green).
Characteristics of cancer driver genes in ABT-SLCs in UCEC. a Percentage of samples possessing at least one somatically mutated ABT-SLC plotted against the median number of somatic mutations per sample for each TCGA project. Linear model (red) fitted to data with 95% confidence interval (grey). b–e TCGA-UCEC project analysis. (b, d–e) n=518 samples. b Of all UCEC samples analysed, the percentage of samples carrying somatic mutations in ABT-SLCs, and the mutation type. c Log2(TPM+1) counts of ABT-SLC mRNA in primary tumours ranked by median. n=553 samples. d–e p=0.05 denoted by red dashed line. d MutSigCV analysis performed on the GenePattern server (http://cloud.genepattern.org) using default coverage and covariate files. Results displayed for ABT-SLCs and the 10 most significant (by p-value) genes with fill denoting fdr (q-value). e Proportion of somatic mutations clustering at genomic loci plotted against statistical significance as calculated by the oncodrive function in maftools. ABT-SLCs and top 10 most significant (by p-value) genes labelled
We selected UCEC for further analyses, given that it was furthest away from the linear relationship. Strikingly, in UCEC, the percentage of tumour samples carrying ABT-SLC somatic mutations was substantially greater than the pan-cancer average: 1–9% (Fig. 2b). In line with our pan-cancer findings, somatic MCT mutations were generally the least common ABT-SLC mutations among UCEC tumour samples, whereas AEs, NBCs, and specific NHEs were the most common somatic ABT-SLC mutations in UCEC tumour samples. The functional impact of somatic mutations on cell fitness is likely to be greater for transporters that are responsible for a significant component of ion/solute flux. Accepting concerns about non-stoichiometric coupling between transcript and proteins levels, we used ABT-SLC expression levels in the UCEC cohort as a surrogate of transport activity (Fig. 2c). Open-access transcriptome profiling (STAR–Counts workflow) data for TCGA-UCEC primary tumours were downloaded from the GDC data portal via TCGAbiolinks [23]. To compare absolute expression levels between ABT-SLCs, transcripts per million (TPM) counts were analysed. Importantly, there was relatively high expression of the AEs SLC4A2, SLC26A6, and SLC4A3, and the MCTs SLC16A3 and SLC16A1, which represent some of the most and least commonly somatically mutated ABT-SLCs in UCEC (Fig. 2b).
Whilst the analysis in Fig. 2a accounted for variation in median tumour mutation burden between cancer types, it is also important to consider that background mutation frequencies vary along an individual genome. This information is important when assessing whether a certain gene is mutated in excess over its expected background mutation rate [50]. To this end, we employed the MutSigCV algorithm to identify cancer driver genes in our UCEC simple nucleotide variation data (Fig. 2d) [51]. MutSigCV is considered a robust computational method because it accounts for multiple patient- and genomic position-based factors which can influence background mutation rate, including overall mutation rate and spectrum, DNA replication timing, and chromatin state estimation [51]. MutSigCV analysis was performed on the GenePattern server (http://cloud.genepattern.org) using default coverage and covariate files. None of the ABT-SLCs had a false discovery rate (fdr) below 5%, but SLC4A3 had a significant non-adjusted p-value (p=0.0167) and emerged as an outlier to other ABT-SLCs (Fig. 2d).
We next sought to explore whether any ABT-SLCs expressed in UCEC fulfil the second characteristic of cancer driver genes: clustering around genomic loci corresponding to critical amino acid residues [28]. The oncodrive function (maftools R package) [57] is based on the OncodriveCLUST algorithm, which identifies genes with a significant bias towards mutational hotspots within the protein sequence [77]. We applied oncodrive to our UCEC simple nucleotide variation data. Overall, there was no evidence for significant clustering of mutations into specific functional domains in ABT-SLCs (Fig. 2e) [57]. However, it is notable that SLC4A3, which emerges as a highly mutated ABT-SLC, had the highest percentage of somatic mutations located in positional clusters (50.76%) among all ABT-SLCs (Fig. 2e, purple dashed outline).
In addition to driver gene criteria based on mutation rate and positional clustering, it is pertinent to evaluate the predicted consequences of somatic mutations on protein function when considering positive selection. Indeed, only somatic mutations which alter cellular function may confer a differential survival advantage. To this end, we explored the PolyPhen-2 [1] and SIFT [63] scores included in the TCGA-UCEC simple nucleotide variation data download (Fig. 3a–c). PolyPhen-2 and SIFT predict the effects on protein function of missense mutations, which account for the vast majority of somatic ABT-SLC mutations in UCEC (Fig. 2b). SIFT predicted an excess of deleterious over tolerated mutations in the case of most ABT-SLCs, except for SLC9A7, SLC9C1, and SLC16A3 (Fig. 3a). For most ABT-SLCs, fewer than half of mutations had benign effects on protein function as predicted by PolyPhen-2, except for SLC9A1, SLC4A1, SLC9A7, SLC16A3, SLC9C1, and SLC16A8 (Fig. 3b).
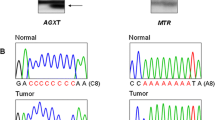
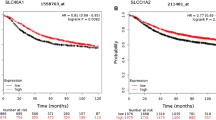
Functional consequences of somatic ABT-SLC mutations. a–e TCGA-UCEC project analysis. a, b n=154 samples. a Log2 of the ratio of somatic missense mutations predicted to be deleterious/tolerated by SIFT score for each ABT-SLC. b Proportion of somatic missense mutations denoted as benign, possibly damaging or probably damaging by PolyPhen-2 score for each ABT-SLC. c Ratios calculated in a plotted against the proportion of somatic missense mutations denoted as benign as calculated in b. Genes with <0.5 benign proportion and >2 deleterious/tolerated ratio labelled ‘high predicted impact’. Genes with >0.5 benign proportion and <1 deleterious/tolerated ratio labelled ‘low predicted impact’. d DESeq2-normalised (design ~1) SLC4A3 mRNA counts for individuals with known SLC4A3 somatic mutation status. Wilcoxon rank sum test. n=451 (non-mutant), 58 (mutant). e Overall survival analysis for TCGA-UCEC samples with both clinical and simple nucleotide variation open-access data available via TCGAbiolinks. n=461 (non-mutant), 49 (mutant in either SLC16A1, SLC16A3, SLC16A7, or SLC16A8). Log-rank test. f Pan-cancer analysis. Mean number of additional mutations/tumour in each ABT-SLC sub-group, in tumours carrying at least one mutation in that sub-group. n=729 (AE), 227 (MCT), 679 (NBC), 869 (NHE) tumour samples. One-way ANOVA
To improve the accuracy of the functional predictions, we combined both SIFT and PolyPhen-2 to highlight ABT-SLCs whose mutations are predicted to have high and low impacts on protein function according to both approaches (Fig. 3c). Notably, SLC9C1 mutations were predicted to have low functional impact, thus likely represent passenger mutations, yet SLC9C1 was the most abundantly mutated ABT-SLC pan-cancer (Fig. 1b) and in UCEC (Fig. 2b). These observations may be explained by the low relative expression of SLC9C1 (Fig. 2c), which suggests that SLC9C1 contribution to ensemble plasma membrane acid-base transport is minimal. Consequently, it is unlikely that SLC9C1 mutations sufficiently alter acid-base transport to provide a survival advantage, from which positive selection for SLC9C1 mutations with high functional impact could ensue. Strikingly, SLC4A3 had the second highest ratio of deleterious/tolerated mutations (SIFT) and the highest proportion of non-benign mutations (PolyPhen-2). Given that we highlighted SLC4A3 as having a high mutation burden, meaningful transcript levels, and a MutSigCV p-value <0.05, it is plausible that the enrichment of functionally damaging SLC4A3 mutations may indicate a degree of positive selection [56].
To further explore the functional impact of SLC4A3 somatic mutations, we analysed SLC4A3 expression in tumour samples included in both our transcriptomic and simple nucleotide variation UCEC data. Lowly expressed genes were filtered out of the unstranded counts prior to DESeq2 normalisation [55]. Tumours carrying somatic SLC4A3 mutations expressed significantly less SLC4A3 mRNA (Fig. 3d). Interestingly, it has recently been shown that lysosomal degradation of its closely related isoform, SLC4A2, is an adaptation mechanism to low pHe in colorectal cancer cells which provides a relatively alkaline cytoplasm [60]. Consequently, we speculate that loss-of-function mutations to SLC4A3 impair its acid-loading function in UCEC. The higher pHi attained this way would improve UCEC cell fitness under selection by intra-tumoural acidosis.
Previous large-scale pan-cancer algorithmic analyses have provided conflicting evidence as to whether ABT-SLCs can be cancer drivers [6, 28, 50, 56]. One of the first applications of algorithm-based detection to whole-genome pan-cancer data identified the AE SLC26A3 and the NBC SLC4A5 as drivers in 2–3% of glioblastoma multiforme and 3–5% of LUAD cases, respectively [50]. However, alternative algorithmic approaches have not confirmed any ABT-SLCs as cancer drivers [6, 28, 56]. These include a pan-software approach, where 26 different computational tools were used to validate candidate genes, and algorithms accounting for the differences in the typical nucleotide sequences flanking driver versus passenger mutations.
Cancer driver mutations are expected to confer an unambiguous advantage to cancer cells. The absence of ABT-SLCs among putative cancer driver genes identified in many analyses [6, 28, 56] may indicate that their mutations do necessarily confer an unequivocal fitness benefit. In carcinomas developing from epithelia, somatic mutations impairing trans-epithelial ABT-SLC-dependent transport may release ATP for hyperproliferation [27], which would benefit the cancer cell. For example, stomach adenocarcinoma (STAD) and pancreatic adenocarcinoma (PAAD) (Fig. 2a, blue dash outline) develop from epithelia that transport large and complementary acid-base fluxes across apical and basolateral membranes as part of wider systems-level processes. However, loss-of-function mutations in ABT-SLCs may cause weaker pHi control and lower steady-state pHi [4], unless compensated for by tandem loss-of-function in acid-loading transport (e.g. AE), a scenario that is unlikely to occur by chance alone. Thus, the overall fitness benefit of loss-of-function mutations in NBC and NHE genes is unclear, as this has to balance the greater availability of ATP against weaker pHi control. The converse would also be true for gain-of-function mutations, and the overall benefit to cancer cells may be conditional.
A second factor underpinning the uncertainty surrounding ABT-SLCs as cancer driver genes relates to spatial considerations in bulk whole-genome/exome sequencing analyses. Whether or not a somatic mutation provides a survival benefit to a cell, relative to neighbouring cells, is dependent upon selection pressures within its microenvironment [11]. pHe is spatially heterogenous within a tumour [69], and acidosis is more common at the invasive edge or central hypoxic core. Gain-of-function mutations in acid-extruders or loss-of-function mutations in acid-loaders, for example, might only provide a survival benefit in specific tumour regions. When cancer cells from acidic and non-acidic tumour regions are pooled for sequencing, acidosis-specific cancer driver genes could be obscured.
Are genes coding for acid-base transporters essential to cancer?
Whereas cancer driver genes provide a relative survival benefit when mutated, essential genes are required in their wildtype form for the absolute survival of cancer cells [89]. Within a cancer, loss-of-function somatic mutations in essential genes can be negatively selected against. Whilst the direction of evolution in cancer is dominated by positive selection (1–3.9% of somatic mutations), it is estimated that 0.02–0.5% of somatic mutations do undergo negative selection [56]. Over the last decade, the development of CRISPR knockout screens has enabled the detection of genes essential for fitness in cancer cells in vitro [61, 89].
Notably, many therapeutics targeting essential genes are associated with limiting toxicities and have often failed Phase 2/3 clinical trials [17]. These include inhibitors of cell cycle controllers, epigenetic regulators, protein homeostasis, and DNA-damage responses. These failures are because many essential genes are common to both cancer cells and healthy tissues. A potential solution is to target pathways that are essential to cell survival only under microenvironmental conditions that are cancer-specific. Intra-tumoural acidosis is one such cancer-specific selection pressure [11]. Given that ABT-SLCs are required to maintain an alkaline pHi in cancer cells under low pHe [4], it is plausible that certain ABT-SLCs could be cancer-specific essential genes and therefore important therapeutic candidates. For example, SLC9A1 genetic ablation may not inhibit cell line growth under control conditions [4], yet significantly impairs cancer cell survival at low pHe [61].
Whilst ABT-SLCs can be essential in vitro, it is critical to determine whether these findings translate to cancer patients. One such approach is to assess negative selection of somatic mutations in ABT-SLCs. Indeed, if somatic mutations in a particular gene were negatively selected, it would implicate that its loss compromises cell fitness, thus identifying essential genes in a patient’s cancer [7]. Intriguingly, somatic mutations in multiple SLC genes are thought to be negatively selected in cancer. In an analysis of 7546 individual tumour exomes from the TCGA database, negatively selected genes were found to be enriched for the transport of glucose, bile salts, organic acids, metal ions, and amine compounds [90]. Out of the negatively selected genes related to molecular transport, the most significant involved glucose transport and metabolism, including genes encoding the glycolysis enzyme glucokinase (GCK), the glucose importers GLUT1 (SLC2A1) and GLUT8 (SLC2A8), and MCT4 (SLC16A3). In a similar pan-cancer analysis, Bányai et al. identified SLC2A1, SLC16A3, and the glycolysis gene G6PD to be negatively selected in human cancers [7]. Clearly, the patterns of negative selection in human tumours paint a pro-glycolytic picture in which transport of the end-products, lactate/H+, by MCTs is essential for cancer cell fitness.
Our analyses are consistent with the notion that plasma membrane transport of substrates and products of fermentation is essential in human tumours. Pan-cancer, a relatively small proportion of tumours carried somatic mutations in MCTs (Fig. 1b-c). Moreover, in UCEC, a tumour cohort with sufficiently frequent MCT mutations to power such analyses, somatic MCT mutations were associated with significantly better overall survival (Fig. 3e). This finding implies that loss of wildtype MCTs could be detrimental to UCEC progression, a feature expected of an essential gene in cancer.
A mechanistic explanation for the proposed essentiality of MCTs in cancer is that their loss-of-function suppresses glycolytic rate [79] and compromises the supply of ATP and key biosynthetic intermediates for proliferation [94]. An alternative explanation may relate to the excessive build-up of intracellular lactate/H+ that could be deleterious to cell growth. Indeed, knock-down of SLC16A3 expression in breast cancer cells reduces the capacity of pHi to recover from an acid load [4]. Pharmacological inhibition or genetic silencing of SLC16A1 and/or SLC16A3 reduces proliferation, and the build-up of intracellular lactate is associated with enhanced production of reactive oxygen species [13, 25, 80]. This disrupted redox balance has been proposed to hamper oxidative phosphorylation, a metabolic pathway which is thought to be essential for cancer cell survival at low pHe [61]. A third explanation relates to intracellular accumulation of non-lactate monocarboxylates, such as pyruvate, when MCT activity is impaired. Indeed, MCT1 inhibition in glycolytic breast cancer cells co-expressing MCT1 and MCT4 acutely reduced pyruvate export, without a reduction in lactate export [41]. When these cells were xenografted into mice, MCT1 inhibition blocked the growth of mammary fat pad tumours.
Despite strong in vitro and clinical evidence for MCT essentiality, it remains unclear whether MCT inhibitors will be effective in the clinic. Firstly, acute reductions in MCT permeability by pharmacological inhibitors can be somewhat overcome over longer time periods by an increased [lactate] driving force, a phenomenon known as autoregulation [12]. Secondly, there are questions regarding the specificity of MCT essentiality to cancer. Indeed, MCT1 is expressed in almost all cell types and can act bi-directionally depending on the substrate gradient. In cancer, where fermentive rate is elevated, the gradient typically favours H+/lactate export [74]. However, the gradient can be reversed in many healthy tissues, facilitating lactate import. In the brain, lactate is one of the most crucial energy substrates after glucose [2]. Accordingly, MCT1 expression is highly localised around axons and oligodendrocytes [2]. Moreover, neurological sequelae have been described in patients with germline inactivating SLC16A1 mutations [2]. This might raise concerns regarding the safety profile of the systemic administration of MCT1 inhibitors to cancer patients. Indeed, the oral MCT1 inhibitor, AZD3965, has reached a Phase 1 clinical trial, where adverse effects including retinopathy, fatigue, and systemic acidosis were observed [37].
To what degree is there redundancy in the acid-base transport system of cancers?
A major biological phenomenon acting against gene essentiality is functional redundancy in systems, including pHi control. This considers whether the impairment to one acid-base transporter can be compensated for by another cell- or population-level mechanism. Functional redundancy among pHi regulatory systems would confer cancer cells with greater resistance to the therapeutic manipulation of acid-base balance. Moreover, it is well-recognised that functional redundancy is more likely if a gene has multiple paralogs with high sequence similarities [26], which is the case for many ABT-SLCs [3]. However, numerous in vitro studies have indicated that functional redundancy among ABT-SLCs may not always manifest. SiRNA-mediated knock-down of the acid-loading AE SLC4A2 can raise steady-state pHi in colorectal cancer cells [60]. Even though there are far more types of acid-extruders than acid-loaders, piecewise knock-down of acid-extruders (SLC9A1, SLC4A7, or SLC16A3) can be sufficient to impair pHi control in cancer cells [4].
To explore whether these in vitro observations might translate to patients, we analysed the number of somatic mutations that tumours accrue in each sub-group of ABT-SLCs using the pan-cancer simple nucleotide variation data previously downloaded (Fig. 3f). For tumour samples carrying a single mutation to either an MCT, NHE, NBC, or AE transporter, we calculated the average number of additional somatic mutations within the affected transporter sub-group per tumour sample. Strikingly, when tumours carried a somatic mutation in an ABT-SLC, there were less than 0.5 additional somatic mutations/tumour sample affecting that same transporter sub-group. Whilst 17.58% of tumour samples carry at least one ABT-SLC mutation (Fig. 1b), few tumours are able to carry multiple somatic mutations affecting the same sub-group of ABT-SLC (i.e. MCT, NHE, NBC, or AE). Assuming that at least some somatic mutations affect protein function, this finding implies that there is a degree of functional redundancy within each sub-group of ABT-SLC that can compensate for a single somatic mutation, but less so for multiple mutated transporters. Relative to other ABT-SLCs, tumours carried significantly fewer additional MCT mutations (Fig. 3f), possibly related to the postulated essentiality of MCTs.
Whilst many NHEs, NBCs, and AEs do not exhibit functional redundancy in vitro [4], it is somewhat surprising that MCTs are the only ABT-SLCs that have been proposed as essential genes in human cancers thus far [7, 90]. A possible explanation for the disparity between observations in vitro and in patients is the nature of cell monocultures. The expression profile of a cancer cell line monoculture is almost infinitely narrower than the transcriptomic landscape of the genetically heterogenous cancer cell population within a tumour, where there is a much higher likelihood of paralog co-expression. This phenomenon is illustrated by studies of MCT inhibition in the lymphoblast-like cell line Raji, which express MCT1, but not MCT4 [25]. MCT1 inhibition by AZD3965 impairs Raji cell growth. However, in viral-driven lymphoma cell lines where MCT1 and MCT4 are co-expressed, neither AZD3965 nor the MCT4 inhibitor VB124 alone affect cell growth [13]. Only dual inhibition of both MCT isoforms is sufficient to impact proliferation. Clearly, functional redundancy is not always present in vitro due to cancer cell line-specific isoform expression that is unrepresentative of in vivo expression.
Compensation for a deficit in a cell’s pH-regulatory apparatus occurs not only at the level of an individual cell, but also at a population level. In population-level compensation, the ‘unit’ under consideration is a syncytial network of cancer cells coupled by gap junctions [75]. Gap junctions mediate the exchange and sharing of small metabolites between cancer cells [29, 30, 62, 75]. Whilst protons permeate gap junctions slowly due to their heavy cytoplasmic buffering, the ABT-SLC substrates lactate and bicarbonate are more rapidly dissipated, e.g. between pancreatic ductal adenocarcinoma cell lines via connexin43-based gap junctions [30]. In a heterogenous cancer cell population, defective pH regulation in one subclone might therefore be compensated for by a fully operational pH-regulatory apparatus in diffusively coupled neighbouring cells. For example, co-culture of SLC9A1-/- and SLC9A1 wildtype colorectal cancer cells rescues the defective pHi recovery of the SLC9A1-/- cells following an acid load, likely due to metabolite dissipation via connexin26-based gap junctions [62]. Such diffusive coupling via gap junctions may permit population-level functional redundancy in ABT-SLCs in patients that cannot be observed in genetically homogenous cell line monocultures.
Future directions
Physiologists will be familiar with Claude Bernard’s assertion that ‘the stability of the milieu intérieur is a condition for a free and independent life’ because it introduced the concept of homeostasis [40]. A homeostatic challenge at the cellular level is the control of solute and ion concentrations, which is why physiologists concur that SLCs are critical. Low pHe is a major homeostatic challenge facing cancer cells and exerts a substantial selection pressure in the context of intra-tumoural genetic and epigenetic heterogeneity [11]. Consequently, we sought to evaluate the role of ABT-SLCs in intra-tumoural evolution.
In many cancer types, we find that the proportion of tumours carrying somatic ABT-SLC mutations is proportional to tumour mutation burden. However, in UCEC, somatic ABT-SLC mutations are more prevalent than expected from the median tumour mutation burden (Fig. 2a). Furthermore, the majority of these mutations are predicted to detrimentally impact protein function (Fig. 3a–c). However, the role and mechanisms of pHi regulation specific to the endometrium remain largely unexplored. Such investigations are warranted, not least due to the unique physiology of the endometrium. Physiological hypoxia has been proposed to occur in the endometrium during menses [58, 68]. Hypoxia-inducible factor (HIF) signalling augments lactate/H+ production via upregulation of glycolytic enzymes, and MCT4 is a known HIF-1 target [82]. Whilst the average age of the TCGA-UCEC cohort is 63.9±11.1 years (mean±standard deviation) [86], it could be interesting to explore whether alterations in endometrial ABT-SLC function earlier in life impact tumourigenesis.
In pan-cancer analyses, we find that SLC4A3 ranks as the second most commonly mutated ABT-SLC (Fig. 1b). In UCEC, SLC4A3 can be highly expressed at transcript level relative to other ABT-SLCs (Fig. 2c). SLC4A3 somatic mutation is associated with significantly lower SLC4A3 mRNA levels (Fig. 3d), and most SLC4A3 missense mutations are predicted to be detrimental to SLC4A3 function (Fig. 3a–c). However, widely utilised algorithm-based approaches to detect cancer driver genes do not definitively identify SLC4A3 when considering both p-value and fdr (Fig. 2d, e). Moreover, it is surprising that many ABT-SLCs are not identified by contemporary in silico studies of selection in cancer [6, 28, 56], given that germline ABT-SLC SNPs can increase cancer risk [20, 95] and genetic ablation of ABT-SLCs substantially impairs cancer cell fitness in vitro [4, 60].
This paradox can be explained in terms of the non-stoichiometric relationship between genotype and phenotype and draws caution to our heavy reliance on genomics in oncology. Intra-tumoural evolution, like species-level evolution, selects for phenotype rather than genotype per say [11]. Phenotype is influenced at a myriad of levels: not only by genomics and epigenomics, but also by factors such as post-translational modification, neighbouring cell function, allosteric regulation, and a cell’s chemical microenvironment. There is clearly a need to explore ABT-SLCs beyond cancer cell line monocultures towards informative studies in human cancers. A mutation-based approach is currently one of the few feasible methods to explore SLCs in human tumour evolution, yet it is important to acknowledge its reductionist nature in comparison to the measurement of phenotype, i.e. SLC-generated ionic or solute fluxes.
A clear direction of future work is thus to annotate important physiological parameters into analyses of ABT-SLCs in patients. Microenvironmental factors which are intrinsically linked to ABT-SLC function, such as pHe and hypoxia, could be integrated into analyses that preserve the location of cells within the microenvironment of a human tumour. These include spatially resolved genomic and transcriptomic sequencing, such as slide-DNA-seq [93] or in situ genome sequencing [67]. Surface membrane-expressed markers of hypoxia (such as CA9 [43]) or acid-adaptation (such as LAMP2 [60]) might be leveraged for this purpose. For example, spatial transcriptomics platforms could be combined with immunofluorescence staining of markers [36], or markers could be used for cell sorting followed by single-cell exome sequencing [78]. Given that robust intracellular pH-reporters, such as cSNARF-1, already exist, ABT-SLC flux could be measured directly in patient-derived organoids and xenografts. Physiologically and clinically relevant methods to interrogate ABT-SLCs in cancer will ultimately yield improved therapeutic targets.
Our findings are consistent with previous reports that MCTs are essential in cancer [7, 90]. Pan-cancer, SLC16A3 and SLC16A8 are somatically mutated in less than 1% of tumours (Fig. 1b). When ABT-SLCs are ranked by the abundance of somatic mutations pan-cancer, the cumulative incidence of somatic MCT mutations is even below that of SLC transporters which supply cancer cells with critical macromolecules for cell division, including glucose, amino acids, and nucleotides/nucleosides (Fig. 1c). Analysis of tumour samples carrying multiple somatic mutations within each ABT-SLC sub-group suggests that there is less functional redundancy within MCTs relative to AEs, NBCs, and NHEs (Fig. 3f). Moreover, UCEC progression is significantly hampered in tumours containing somatic MCT mutations (Fig. 3e). Our findings support efforts to develop MCT inhibitors for clinical use [37]; however, future work might focus on improving selectivity.
MCTs, and indeed other ABT-SLCs, are expressed in many non-tumour tissues due to their near-universal housekeeping functions and roles in systems-level physiological processes [74]. Targeting any ABT-SLC therefore risks adverse effects. A potential solution lies in novel therapeutic delivery systems. Given the close relationship between ABT-SLCs and intra-tumoural acidosis, pHe-dependence of therapeutic delivery will be critical to improving selectivity. For example, cargo unloading of emerging delivery mechanisms, such as extracellular vesicles, could be targeted to acid-induced epitopes on the cell surface [49]. pH-(low) insertion peptides (pHLIP) are an exciting technology based on peptide constructs which can fold into a transmembrane helix, allowing insertion and crossing of the cell membrane, only at low pHe [54]. pHLIP constructs may be engineered to deliver cargo into tumour cells in vivo, such as fluorescent markers or even therapeutics. Indeed, a Phase 2a clinical trial employing imaging of fluorescently labelled pHLIP to guide tumour margin detection in breast cancer surgery has recently begun (ClinicalTrials.gov Identifier: NCT05130801).
Ultimately, genomic approaches alone are insufficient to elucidate and clinically harness acid-base transport in cancer. Clearly, physiology-based approaches are necessary in both target validation and delivery mechanisms to enable ABT-SLCs to become effective therapeutic targets in oncology.
Data availability
The datasets analysed during the current study are available from the National Cancer Institute GDC Data Portal, https://portal.gdc.cancer.gov/.
References
Adzhubei IA, Schmidt S, Peshkin L, Ramensky VE, Gerasimova A, Bork P, Kondrashov AS, Sunyaev SR (2010) A method and server for predicting damaging missense mutations. Nat Methods 7:248–249. https://doi.org/10.1038/nmeth0410-248
Al-Khawaga S, AlRayahi J, Khan F, Saraswathi S, Hasnah R, Haris B, Mohammed I, Abdelalim EM, Hussain K (2019) A SLC16A1 mutation in an infant with ketoacidosis and neuroimaging assessment: expanding the clinical spectrum of MCT1 deficiency. Front Pediatr 7:299. https://doi.org/10.3389/fped.2019.00299
Anderegg MA, Gyimesi G, Ho TM, Hediger MA, Fuster DG (2022) The less well-known little brothers: the SLC9B/NHA sodium proton exchanger subfamily-structure, function, regulation and potential drug-target approaches. Front Physiol 13:898508. https://doi.org/10.3389/fphys.2022.898508
Andersen AP, Samsoe-Petersen J, Oernbo EK, Boedtkjer E, Moreira JMA, Kveiborg M, Pedersen SF (2018) The net acid extruders NHE1, NBCn1 and MCT4 promote mammary tumor growth through distinct but overlapping mechanisms. Int J Cancer 142:2529–2542. https://doi.org/10.1002/ijc.31276
Ascierto PA, Kirkwood JM, Grob J, Simeone E, Grimaldi AM, Maio M, Palmieri G, Testori A, Marincola FM, Mozzillo N (2012) The role of BRAF V600 mutation in melanoma. J Transl Med 10. https://doi.org/10.1186/1479-5876-10-85
Bailey MH, Tokheim C, Porta-Pardo E, Sengupta S, Bertrand D, Weerasinghe A, Colaprico A, Wendl MC, Kim J, Reardon B, Ng PK, Jeong KJ, Cao S, Wang Z, Gao J, Gao Q, Wang F, Liu EM, Mularoni L et al (2018) Comprehensive characterization of cancer driver genes and mutations. Cell 173(371-385):e318. https://doi.org/10.1016/j.cell.2018.02.060
Banyai L, Trexler M, Kerekes K, Csuka O, Patthy L (2021) Use of signals of positive and negative selection to distinguish cancer genes and passenger genes. Elife 10. https://doi.org/10.7554/eLife.59629
Barbuskaite D, Pedersen FD, Christensen HL, Johnsen LO, Praetorius J, Damkier HH (2020) NBCe2 (Slc4a5) is expressed in the renal connecting tubules and cortical collecting ducts and mediates base extrusion. Front Physiol 11:560. https://doi.org/10.3389/fphys.2020.00560
Bartman CR, Weilandt DR, Shen Y, Lee WD, Han Y, TeSlaa T, Jankowski CSR, Samarah L, Park NR, da Silva-Diz V, Aleksandrova M, Gultekin Y, Marishta A, Wang L, Yang L, Roichman A, Bhatt V, Lan T, Hu Z et al (2023) Slow TCA flux and ATP production in primary solid tumours but not metastases. Nature 614:349–357. https://doi.org/10.1038/s41586-022-05661-6
Black JRM, McGranahan N (2021) Genetic and non-genetic clonal diversity in cancer evolution. Nat Rev Cancer 21:379–392. https://doi.org/10.1038/s41568-021-00336-2
Blaszczak W, Swietach P (2021) What do cellular responses to acidity tell us about cancer? Cancer Metastasis Rev 40:1159–1176. https://doi.org/10.1007/s10555-021-10005-3
Blaszczak W, Williams H, Swietach P (2022) Autoregulation of H(+)/lactate efflux prevents monocarboxylate transport (MCT) inhibitors from reducing glycolytic lactic acid production. Br J Cancer 127:1365–1377. https://doi.org/10.1038/s41416-022-01910-7
Bonglack EN, Messinger JE, Cable JM, Ch'ng J, Parnell KM, Reinoso-Vizcaino NM, Barry AP, Russell VS, Dave SS, Christofk HR, Luftig MA (2021) Monocarboxylate transporter antagonism reveals metabolic vulnerabilities of viral-driven lymphomas. Proc Natl Acad Sci U S A 118. https://doi.org/10.1073/pnas.2022495118
Boyd PS, Breitling J, Korzowski A, Zaiss M, Franke VL, Mueller-Decker K, Glinka A, Ladd ME, Bachert P, Goerke S (2022) Mapping intracellular pH in tumors using amide and guanidyl CEST-MRI at 9.4 T. Magn Reson Med 87:2436–2452. https://doi.org/10.1002/mrm.29133
Broer S (2020) Amino acid transporters as targets for cancer therapy: why, where, when, and how. Int J Mol Sci 21. https://doi.org/10.3390/ijms21176156
Cancer Genome Atlas Research N, Weinstein JN, Collisson EA, Mills GB, Shaw KR, Ozenberger BA, Ellrott K, Shmulevich I, Sander C, Stuart JM (2013) The Cancer Genome Atlas Pan-Cancer analysis project. Nat Genet 45:1113–1120. https://doi.org/10.1038/ng.2764
Chang L, Ruiz P, Ito T, Sellers WR (2021) Targeting pan-essential genes in cancer: challenges and opportunities. Cancer Cell 39:466–479. https://doi.org/10.1016/j.ccell.2020.12.008
Chen L, Li Y, Deng X (2023) Comprehensive analysis of pan-cancer reveals the potential of SLC16A1 as a prognostic and immunological biomarker. Medicine (Baltimore) 102:e33242. https://doi.org/10.1097/MD.0000000000033242
Chen Q, Liu Y, Zhu XL, Feng F, Yang H, Xu W (2019) Increased NHE1 expression is targeted by specific inhibitor cariporide to sensitize resistant breast cancer cells to doxorubicin in vitro and in vivo. BMC Cancer 19:211. https://doi.org/10.1186/s12885-019-5397-7
Chen W, Zhong R, Ming J, Zou L, Zhu B, Lu X, Ke J, Zhang Y, Liu L, Miao X, Huang T (2012) The SLC4A7 variant rs4973768 is associated with breast cancer risk: evidence from a case-control study and a meta-analysis. Breast Cancer Res Treat 136:847–857. https://doi.org/10.1007/s10549-012-2309-9
Chiang Y, Chou CY, Hsu KF, Huang YF, Shen MR (2008) EGF upregulates Na+/H+ exchanger NHE1 by post-translational regulation that is important for cervical cancer cell invasiveness. J Cell Physiol 214:810–819. https://doi.org/10.1002/jcp.21277
Chow K, Bedo J, Ryan A, Agarwal D, Bolton D, Chan Y, Dundee P, Frydenberg M, Furrer MA, Goad J, Gyomber D, Hanegbi U, Harewood L, King D, Lamb AD, Lawrentschuk N, Liodakis P, Moon D, Murphy DG et al (2021) Ductal variant prostate carcinoma is associated with a significantly shorter metastasis-free survival. Eur J Cancer 148:440–450. https://doi.org/10.1016/j.ejca.2020.12.030
Colaprico A, Silva TC, Olsen C, Garofano L, Cava C, Garolini D, Sabedot TS, Malta TM, Pagnotta SM, Castiglioni I, Ceccarelli M, Bontempi G, Noushmehr H (2016) TCGAbiolinks: an R/Bioconductor package for integrative analysis of TCGA data. Nucleic Acids Res 44:e71. https://doi.org/10.1093/nar/gkv1507
Couetoux du Tertre M, Marques M, Tremblay L, Bouchard N, Diaconescu R, Blais N, Couture C, Pelsser V, Wang H, Higenell V, Izzi L, Gambaro K, Hoffert C, Srivastava A, Spatz A, Rousseau C, McNamara S, Cohen V, Batist G, Agulnik J (2019) Analysis of the genomic landscape in ALK+ NSCLC patients identifies novel aberrations associated with clinical outcomes. Mol Cancer Ther 18:1628–1636. https://doi.org/10.1158/1535-7163.MCT-19-0105
Curtis NJ, Mooney L, Hopcroft L, Michopoulos F, Whalley N, Zhong H, Murray C, Logie A, Revill M, Byth KF, Benjamin AD, Firth MA, Green S, Smith PD, Critchlow SE (2017) Pre-clinical pharmacology of AZD3965, a selective inhibitor of MCT1: DLBCL, NHL and Burkitt’s lymphoma anti-tumor activity. Oncotarget 8:69219–69236. https://doi.org/10.18632/oncotarget
De Kegel B, Ryan CJ (2019) Paralog buffering contributes to the variable essentiality of genes in cancer cell lines. PLoS Genet 15:e1008466. https://doi.org/10.1371/journal.pgen.1008466
Demaurex N, Romanek RR, Orlowski J, Grinstein S (1997) ATP dependence of Na1/H1 exchange. J Gen Physiol 109:117–128. https://doi.org/10.1085/jgp.109.2.117
Dietlein F, Weghorn D, Taylor-Weiner A, Richters A, Reardon B, Liu D, Lander ES, Van Allen EM, Sunyaev SR (2020) Identification of cancer driver genes based on nucleotide context. Nat Genet 52:208–218. https://doi.org/10.1038/s41588-019-0572-y
Dovmark TH, Hulikova A, Niederer SA, Vaughan-Jones RD, Swietach P (2018) Normoxic cells remotely regulate the acid-base balance of cells at the hypoxic core of connexin-coupled tumor growths. FASEB J 32:83–96. https://doi.org/10.1096/fj.201700480R
Dovmark TH, Saccomano M, Hulikova A, Alves F, Swietach P (2017) Connexin-43 channels are a pathway for discharging lactate from glycolytic pancreatic ductal adenocarcinoma cells. Oncogene 36:4538–4550. https://doi.org/10.1038/onc.2017.71
Esposito MR, Binatti A, Pantile M, Coppe A, Mazzocco K, Longo L, Capasso M, Lasorsa VA, Luksch R, Bortoluzzi S, Tonini GP (2018) Somatic mutations in specific and connected subpathways are associated with short neuroblastoma patients' survival and indicate proteins targetable at onset of disease. Int J Cancer 143:2525–2536. https://doi.org/10.1002/ijc.31748
Fei F, Guo X, Chen Y, Liu X, Tu J, Xing J, Chen Z, Ji J, He X (2015) Polymorphisms of monocarboxylate transporter genes are associated with clinical outcomes in patients with colorectal cancer. J Cancer Res Clin Oncol 141:1095–1102. https://doi.org/10.1007/s00432-014-1877-y
Fisel P, Kruck S, Winter S, Bedke J, Hennenlotter J, Nies AT, Scharpf M, Fend F, Stenzl A, Schwab M, Schaeffeler E (2013) DNA methylation of the SLC16A3 promoter regulates expression of the human lactate transporter MCT4 in renal cancer with consequences for clinical outcome. Clin Cancer Res 19:5170–5181. https://doi.org/10.1158/1078-0432.CCR-13-1180
Giesen N, Paramasivam N, Toprak UH, Huebschmann D, Xu J, Uhrig S, Samur M, Bahr S, Frohlich M, Mughal SS, Mai EK, Jauch A, Muller-Tidow C, Brors B, Munshi N, Goldschmidt H, Weinhold N, Schlesner M, Raab MS (2022) Comprehensive genomic analysis of refractory multiple myeloma reveals a complex mutational landscape associated with drug resistance and novel therapeutic vulnerabilities. Haematologica 107:1891–1901. https://doi.org/10.3324/haematol.2021.279360
Guo X, Chen C, Liu B, Wu Y, Chen Y, Zhou X, Huang X, Li X, Yang H, Chen Z, Xing J (2015) Genetic variations in monocarboxylate transporter genes as predictors of clinical outcomes in non-small cell lung cancer. Tumour Biol 36:3931–3939. https://doi.org/10.1007/s13277-014-3036-0
Hahn N, Bens M, Kempfer M, Reissig C, Schmidl L, Geis C (2023) Protecting RNA quality for spatial transcriptomics while improving immunofluorescent staining quality. Front Neurosci 17:1198154. https://doi.org/10.3389/fnins.2023.1198154
Halford S, Veal GJ, Wedge SR, Payne GS, Bacon CM, Sloan P, Dragoni I, Heinzmann K, Potter S, Salisbury BM, Chenard-Poirier M, Greystoke A, Howell EC, Innes WA, Morris K, Plummer C, Rata M, Petrides G, Keun HC et al (2023) A phase i dose-escalation study of AZD3965, an oral monocarboxylate transporter 1 inhibitor, in patients with advanced cancer. Clin Cancer Res 29:1429–1439. https://doi.org/10.1158/1078-0432.CCR-22-2263
Hediger M, Coady M, Ikeda T, Wright EM (1987) Expression cloning and cDNA sequencing of the Na+/glucose co-transporter. Nature 330:379–381. https://doi.org/10.1038/330379a0
Hediger MA, Clemencon B, Burrier RE, Bruford EA (2013) The ABCs of membrane transporters in health and disease (SLC series): introduction. Mol Aspects Med 34:95–107. https://doi.org/10.1016/j.mam.2012.12.009
Hoenig MP, Zeidel ML (2014) Homeostasis, the milieu interieur, and the wisdom of the nephron. Clin J Am Soc Nephrol 9:1272–1281. https://doi.org/10.2215/CJN.08860813
Hong CS, Graham NA, Gu W, Espindola Camacho C, Mah V, Maresh EL, Alavi M, Bagryanova L, Krotee PAL, Gardner BK, Behbahan IS, Horvath S, Chia D, Mellinghoff IK, Hurvitz SA, Dubinett SM, Critchlow SE, Kurdistani SK, Goodglick L et al (2016) MCT1 modulates cancer cell pyruvate export and growth of tumors that co-express MCT1 and MCT4. Cell Rep 14:1590–1601. https://doi.org/10.1016/j.celrep.2016.01.057
Huang J, Chen M, Xu ES, Luo L, Ma Y, Huang W, Floyd W, Klann TS, Kim SY, Gersbach CA, Cardona DM, Kirsch DG (2019) Genome-wide CRISPR screen to identify genes that suppress transformation in the presence of endogenous Kras(G12D). Sci Rep 9:17220. https://doi.org/10.1038/s41598-019-53572-w
Hulikova A, Harris AL, Vaughan-Jones RD, Swietach P (2013) Regulation of intracellular pH in cancer cell lines under normoxia and hypoxia. J Cell Physiol 228:743–752. https://doi.org/10.1002/jcp.24221
Isakoff SJ, Engelman JA, Irie HY, Luo J, Brachmann SM, Pearline RV, Cantley LC, Brugge JS (2005) Breast cancer-associated PIK3CA mutations are oncogenic in mammary epithelial cells. Cancer Res 65:10992–11000. https://doi.org/10.1158/0008-5472.CAN-05-2612
James DE, Brown R, Navarro J, Pilch PF (1988) Insulin-regulatable tissues express a unique insulin-sensitive glucose transport protein. Nature 333:183–185. https://doi.org/10.1038/333183a0
Janku F, Tsimberidou AM, Garrido-Laguna I, Wang X, Luthra R, Hong DS, Naing A, Falchook GS, Moroney JW, Piha-Paul SA, Wheler JJ, Moulder SL, Fu S, Kurzrock R (2011) PIK3CA mutations in patients with advanced cancers treated with PI3K/AKT/mTOR axis inhibitors. Mol Cancer Ther 10:558–565. https://doi.org/10.1158/1535-7163.MCT-10-0994
Kim M, Kwon CH, Jang MH, Kim JM, Kim EH, Jeon YK, Kim SS, Choi KU, Kim IJ, Park M, Kim BH (2021) Whole-exome sequencing in papillary microcarcinoma: potential early biomarkers of lateral lymph node metastasis. Endocrinol Metab (Seoul) 36:1086–1094. https://doi.org/10.3803/EnM.2021.1132
Kondelin J, Gylfe AE, Lundgren S, Tanskanen T, Hamberg J, Aavikko M, Palin K, Ristolainen H, Katainen R, Kaasinen E, Taipale M, Taipale J, Renkonen-Sinisalo L, Jarvinen H, Bohm J, Mecklin JP, Vahteristo P, Tuupanen S, Aaltonen LA, Pitkanen E (2017) Comprehensive evaluation of protein coding mononucleotide microsatellites in microsatellite-unstable colorectal cancer. Cancer Res 77:4078–4088. https://doi.org/10.1158/0008-5472.CAN-17-0682
Kucuk N, Primozic M, Knez Z, Leitgeb M (2021) Exosomes engineering and their roles as therapy delivery tools, therapeutic targets, and biomarkers. Int J Mol Sci 22. https://doi.org/10.3390/ijms22179543
Lawrence MS, Stojanov P, Mermel CH, Robinson JT, Garraway LA, Golub TR, Meyerson M, Gabriel SB, Lander ES, Getz G (2014) Discovery and saturation analysis of cancer genes across 21 tumour types. Nature 505:495–501. https://doi.org/10.1038/nature12912
Lawrence MS, Stojanov P, Polak P, Kryukov GV, Cibulskis K, Sivachenko A, Carter SL, Stewart C, Mermel CH, Roberts SA, Kiezun A, Hammerman PS, McKenna A, Drier Y, Zou L, Ramos AH, Pugh TJ, Stransky N, Helman E et al (2013) Mutational heterogeneity in cancer and the search for new cancer-associated genes. Nature 499:214–218. https://doi.org/10.1038/nature12213
Lee SK, Occhipinti R, Moss FJ, Parker MD, Grichtchenko II, Boron WF (2023) Distinguishing among HCO 3- , CO 3= , and H + as substrates of proteins that appear to be "bicarbonate" transporters. J Am Soc Nephrol 34:40–54. https://doi.org/10.1681/ASN.2022030289
Liang C, Niu L, Xiao Z, Zheng C, Shen Y, Shi Y, Han X (2020) Whole-genome sequencing of prostate cancer reveals novel mutation-driven processes and molecular subgroups. Life Sci 254:117218. https://doi.org/10.1016/j.lfs.2019.117218
Liu YC, Wang ZX, Pan JY, Wang LQ, Dai XY, Wu KF, Ye XW, Xu XL (2023) Recent advances in imaging agents anchored with pH (Low) insertion peptides for cancer theranostics. Molecules 28. https://doi.org/10.3390/molecules28052175
Love MI, Huber W, Anders S (2014) Moderated estimation of fold change and dispersion for RNA-seq data with DESeq2. Genome Biol 15:550. https://doi.org/10.1186/s13059-014-0550-8
Martincorena I, Raine KM, Gerstung M, Dawson KJ, Haase K, Van Loo P, Davies H, Stratton MR, Campbell PJ (2017) Universal patterns of selection in cancer and somatic tissues. Cell 171(1029-1041):e1021. https://doi.org/10.1016/j.cell.2017.09.042
Mayakonda A, Lin DC, Assenov Y, Plass C, Koeffler HP (2018) Maftools: efficient and comprehensive analysis of somatic variants in cancer. Genome Res 28:1747–1756. https://doi.org/10.1101/gr.239244.118
Maybin JA, Murray AA, Saunders PTK, Hirani N, Carmeliet P, Critchley HOD (2018) Hypoxia and hypoxia inducible factor-1alpha are required for normal endometrial repair during menstruation. Nat Commun 9:295. https://doi.org/10.1038/s41467-017-02375-6
Meixner E, Goldmann U, Sedlyarov V, Scorzoni S, Rebsamen M, Girardi E, Superti-Furga G (2020) A substrate-based ontology for human solute carriers. Mol Syst Biol 16:e9652. https://doi.org/10.15252/msb.20209652
Michl J, Monterisi S, White B, Blaszczak W, Hulikova A, Abdullayeva G, Bridges E, Yin Z, Bodmer WF, Swietach P (2023) Acid-adapted cancer cells alkalinize their cytoplasm by degrading the acid-loading membrane transporter anion exchanger 2, SLC4A2. Cell Rep 42:112601. https://doi.org/10.1016/j.celrep.2023.112601
Michl J, Wang Y, Monterisi S, Blaszczak W, Beveridge R, Bridges EM, Koth J, Bodmer WF, Swietach P (2022) CRISPR-Cas9 screen identifies oxidative phosphorylation as essential for cancer cell survival at low extracellular pH. Cell Rep 38:110493. https://doi.org/10.1016/j.celrep.2022.110493
Monterisi S, Michl J, Hulikova A, Koth J, Bridges EM, Hill AE, Abdullayeva G, Bodmer WF, Swietach P (2022) Solute exchange through gap junctions lessens the adverse effects of inactivating mutations in metabolite-handling genes. Elife 11. https://doi.org/10.7554/eLife.78425
Ng PC, Henikoff S (2003) SIFT: Predicting amino acid changes that affect protein function. Nucleic Acids Res 31:3812–3814. https://doi.org/10.1093/nar/gkg509
Nie JH, Yang T, Li H, Ye HS, Zhong GQ, Li TT, Zhang C, Huang WH, Xiao J, Li Z, He JL, Du BL, Zhang Y, Liu J (2021) Identification of GPC3 mutation and upregulation in a multidrug resistant osteosarcoma and its spheroids as therapeutic target. J Bone Oncol 30:100391. https://doi.org/10.1016/j.jbo.2021.100391
Nowell PC (1976) The clonal evolution of tumor cell populations. Science 194:23–28. https://doi.org/10.1126/science.959840
Payen VL, Mina E, Van Hee VF, Porporato PE, Sonveaux P (2020) Monocarboxylate transporters in cancer. Mol Metab 33:48–66. https://doi.org/10.1016/j.molmet.2019.07.006
Payne AC, Chiang ZD, Reginato PL, Mangiameli SM, Murray EM, Yao CC, Markoulaki S, Earl AS, Labade AS, Jaenisch R, Church GM, Boyden ES, Buenrostro JD, Chen F (2021) In situ genome sequencing resolves DNA sequence and structure in intact biological samples. Science 371. https://doi.org/10.1126/science.aay3446
Reavey JJ, Walker C, Nicol M, Murray AA, Critchley HOD, Kershaw LE, Maybin JA (2021) Markers of human endometrial hypoxia can be detected in vivo and ex vivo during physiological menstruation. Hum Reprod 36:941–950. https://doi.org/10.1093/humrep/deaa379
Rohani N, Hao L, Alexis MS, Joughin BA, Krismer K, Moufarrej MN, Soltis AR, Lauffenburger DA, Yaffe MB, Burge CB, Bhatia SN, Gertler FB (2019) Acidification of tumor at stromal boundaries drives transcriptome alterations associated with aggressive phenotypes. Cancer Res 79:1952–1966. https://doi.org/10.1158/0008-5472.CAN-18-1604
Sardet C, Franchi A, Pouyssegur J (1989) Molecular cloning, primary structure, and expression of the human growth factor-activatable Na+/H+ antiporter. Cell 56:271–280. https://doi.org/10.1016/0092-8674(89)90901-x
Schaaf MB, Garg AD, Agostinis P (2018) Defining the role of the tumor vasculature in antitumor immunity and immunotherapy. Cell Death Dis 9:115. https://doi.org/10.1038/s41419-017-0061-0
Schaller L, Lauschke VM (2019) The genetic landscape of the human solute carrier (SLC) transporter superfamily. Hum Genet 138:1359–1377. https://doi.org/10.1007/s00439-019-02081-x
Stubbs M, Veech RL, Griffiths JR (1995) Tumor metabolism: the lessons of magnetic resonance spectroscopy. Adv Enzyme Regul 35:101–115. https://doi.org/10.1016/0065-2571(94)00016-V
Swietach P (2019) What is pH regulation, and why do cancer cells need it? Cancer Metastasis Rev 38:5–15. https://doi.org/10.1007/s10555-018-09778-x
Swietach P, Monterisi S (2019) A barter economy in tumors: exchanging metabolites through gap junctions. Cancers (Basel) 11. https://doi.org/10.3390/cancers11010117
Swietach P, Vaughan-Jones RD, Harris AL, Hulikova A (2014) The chemistry, physiology and pathology of pH in cancer. Philos Trans R Soc Lond B Biol Sci 369:20130099. https://doi.org/10.1098/rstb.2013.0099
Tamborero D, Gonzalez-Perez A, Lopez-Bigas N (2013) OncodriveCLUST: exploiting the positional clustering of somatic mutations to identify cancer genes. Bioinformatics 29:2238–2244. https://doi.org/10.1093/bioinformatics/btt395
Tang J, Tu K, Lu K, Zhang J, Luo K, Jin H, Wang L, Yang L, Xiao W, Zhang Q, Liu X, Ge XY, Li G, Zhou Z, Xie D (2021) Single-cell exome sequencing reveals multiple subclones in metastatic colorectal carcinoma. Genome Med 13:148. https://doi.org/10.1186/s13073-021-00962-3
Tanner LB, Goglia AG, Wei MH, Sehgal T, Parsons LR, Park JO, White E, Toettcher JE, Rabinowitz JD (2018) Four key steps control glycolytic flux in mammalian cells. Cell Syst 7(49-62):e48. https://doi.org/10.1016/j.cels.2018.06.003
Todenhofer T, Seiler R, Stewart C, Moskalev I, Gao J, Ladhar S, Kamjabi A, Al Nakouzi N, Hayashi T, Choi S, Wang Y, Frees S, Daugaard M, Oo HZ, Fisel P, Schwab M, Schaeffeler E, Douglas J, Hennenlotter J et al (2018) Selective inhibition of the lactate transporter MCT4 reduces growth of invasive bladder cancer. Mol Cancer Ther 17:2746–2755. https://doi.org/10.1158/1535-7163.MCT-18-0107
Ui M (1966) A role of phosphofructokinase in pH-dependent regulation of glycolysis. Biochimica et Biophysica Acta 124:310–322. https://doi.org/10.1016/0304-4165(66)90194-2
Ullah MS, Davies AJ, Halestrap AP (2006) The plasma membrane lactate transporter MCT4, but not MCT1, is up-regulated by hypoxia through a HIF-1alpha-dependent mechanism. J Biol Chem 281:9030–9037. https://doi.org/10.1074/jbc.M511397200
Van Leemputte F, Vanthienen W, Wijnants S, Van Zeebroeck G, Thevelein JM (2020) Aberrant intracellular pH regulation limiting glyceraldehyde-3-phosphate dehydrogenase activity in the glucose-sensitive yeast tps1Delta mutant. mBio 11. https://doi.org/10.1128/mBio.02199-20
Wang D, Pascual JM, Yang H, Engelstad K, Mao X, Cheng J, Yoo J, Noebels JL, De Vivo DC (2006) A mouse model for Glut-1 haploinsufficiency. Hum Mol Genet 15:1169–1179. https://doi.org/10.1093/hmg/ddl032
Wang F (2023) Identification of tumor antigens and immune subtypes of acute myeloid leukemia for mRNA vaccine development. Clin Transl Oncol 25:2204–2223. https://doi.org/10.1007/s12094-023-03108-6
Wang X, Steensma JT, Bailey MH, Feng Q, Padda H, Johnson KJ (2018) Characteristics of The Cancer Genome Atlas cases relative to U.S. general population cancer cases. Br J Cancer 119:885–892. https://doi.org/10.1038/s41416-018-0140-8
Windler F, Bonigk W, Korschen HG, Grahn E, Strunker T, Seifert R, Kaupp UB (2018) The solute carrier SLC9C1 is a Na(+)/H(+)-exchanger gated by an S4-type voltage-sensor and cyclic-nucleotide binding. Nat Commun 9:2809. https://doi.org/10.1038/s41467-018-05253-x
Yang MQ, Li D, Yang W, Zhang Y, Liu J, Tong W (2017) A gene module-based eQTL analysis prioritizing disease genes and pathways in kidney cancer. Comput Struct Biotechnol J 15:463–470. https://doi.org/10.1016/j.csbj.2017.09.003
Yilmaz A, Peretz M, Aharony A, Sagi I, Benvenisty N (2018) Defining essential genes for human pluripotent stem cells by CRISPR-Cas9 screening in haploid cells. Nat Cell Biol 20:610–619. https://doi.org/10.1038/s41556-018-0088-1
Zapata L, Pich O, Serrano L, Kondrashov FA, Ossowski S, Schaefer MH (2018) Negative selection in tumor genome evolution acts on essential cellular functions and the immunopeptidome. Genome Biol 19:67. https://doi.org/10.1186/s13059-018-1434-0
Zhang D, Xia J (2020) Somatic synonymous mutations in regulatory elements contribute to the genetic aetiology of melanoma. BMC Med Genomics 13:43. https://doi.org/10.1186/s12920-020-0685-2
Zhang X, Lin Y, Gillies RJ (2010) Tumor pH and its measurement. J Nucl Med 51:1167–1170. https://doi.org/10.2967/jnumed.109.068981
Zhao T, Chiang ZD, Morriss JW, LaFave LM, Murray EM, Del Priore I, Meli K, Lareau CA, Nadaf NM, Li J, Earl AS, Macosko EZ, Jacks T, Buenrostro JD, Chen F (2022) Spatial genomics enables multi-modal study of clonal heterogeneity in tissues. Nature 601:85–91. https://doi.org/10.1038/s41586-021-04217-4
Zheng J (2012) Energy metabolism of cancer: glycolysis versus oxidative phosphorylation (Review). Oncol Lett 4:1151–1157. https://doi.org/10.3892/ol.2012.928
Zhou Y, Ma X, Sun J (2023) Update on the relationship between the SLC4A7 variant rs4973768 and breast cancer risk: a systematic review and meta-analysis. J Int Med Res 51:3000605231166517. https://doi.org/10.1177/03000605231166517
Acknowledgements
The results published here are in whole or part based upon data generated by the TCGA Research Network: https://www.cancer.gov/tcga.
Funding
Funded by Cancer Research UK (grant reference PHDSTU-Hist\100200) and the European Research Council (Consolidator Grant SURVIVE #723997).
Author information
Authors and Affiliations
Contributions
All authors contributed to the review conception and design. Literature search and data analysis were performed by Bobby White. The first draft of the manuscript was written in full by Bobby White. All authors commented on previous versions of the manuscript, performed revisions, and read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the special issue on Physiology of systemic and cellular pH regulation in Pflügers Archiv—European Journal of Physiology
Supplementary information
ESM 1
(PDF 40 kb)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
White, B., Swietach, P. What can we learn about acid-base transporters in cancer from studying somatic mutations in their genes?. Pflugers Arch - Eur J Physiol 476, 673–688 (2024). https://doi.org/10.1007/s00424-023-02876-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00424-023-02876-y