Abstract
Chronic pain is a global problem affecting up to 20% of the world’s population and has a significant economic, social and personal cost to society. Sensory neurons of the dorsal root ganglia (DRG) detect noxious stimuli and transmit this sensory information to regions of the central nervous system (CNS) where activity is perceived as pain. DRG neurons express multiple voltage-gated sodium channels that underlie their excitability. Research over the last 20 years has provided valuable insights into the critical roles that two channels, NaV1.7 and NaV1.9, play in pain signalling in man. Gain of function mutations in NaV1.7 cause painful conditions while loss of function mutations cause complete insensitivity to pain. Only gain of function mutations have been reported for NaV1.9. However, while most NaV1.9 mutations lead to painful conditions, a few are reported to cause insensitivity to pain. The critical roles these channels play in pain along with their low expression in the CNS and heart muscle suggest they are valid targets for novel analgesic drugs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pain is an important warning system to guard against tissue damage and disease. Pathological pain, however, has no warning value and has huge economic, social and personal costs to society. Chronic pain is a global problem affecting up to 20% of the world’s population [9, 50]. Sensory neurons of the dorsal root ganglia (DRG) detect painful stimuli and transmit sensory information to regions of the central nervous system (CNS) that perceive pain. DRG neurons are a heterogeneous population of neurons with distinct functional and histochemical properties [53, 77]. The DRG contains neurons responding to a variety of non-noxious stimuli (such as proprioceptors and low-threshold mechanoreceptors) as well as those responding to noxious stimuli (nociceptors).
Inflammation and nerve injury sensitise DRG neurons and result in decreased pain thresholds and/or intense pain. This can be in part due to increased voltage-gated sodium channel (VGSC) activity resulting in increased excitability of DRG neurons [8, 104]. VGSCs consist of pore-forming α-subunits and auxiliary β-subunits. There are ten cloned α-subunits and 4 β-subunits. The β-subunits modulate the localisation, expression and functional properties of α-subunits [12]. Each α-subunit is composed of four homologous membrane-spanning domains (DI-DIV). Each domain consists of six transmembrane segments (S1-S6) [12]. Different α-subunits have distinct electrophysiological and pharmacological properties [12, 104], and DRG neurons express multiple α-subunits that are essential to their ability to fire action potentials [104].
This review aims to clarify the roles of two VGSC channels expressed selectively, though not exclusively, in primary sensory neurons in pain pathways, and in the light of evidence from genetic mouse models and mutations in man. We discuss the usefulness of these channels as potential drug targets, and suggest that while our present understanding of function has grown more complex, targeting these channels either alone or in combination may still provide a strategy for analgesic development, potentially even for chronic use.
VGSC as targets for analgesic drugs
There are two reasons why VGSCs are attractive targets for analgesic drugs. Firstly, VGSCs are required for the firing of action potentials in DRG neurons; therefore, blocking their activity will reduce pain signalling in painful conditions even if they were not the primary or only contributor to increased firing. For example, sensitisation of primary transducing channels, like the transient receptor potential (TRP) channels, is often involved in many forms of pathological pain [11, 90, 105]. This sensitisation will lead to greater generator potentials in sensory nerve terminals. However, since VGSCs are required to initiate an action potential in nerve terminals and to allow conduction into the CNS, an effective VGSC blocker can still cancel out the effect of the sensitised TRP channels in nerve terminals.
Secondly, a few of the VGSC α-subunits expressed in DRG are either exclusive to or enriched in DRG neurons that signal pain, with little expression in other DRG neurons, the CNS, skeletal and heart muscles. Blockers for these subunits would therefore be expected to produce analgesia without detrimental side effects. DRG neurons express many of the cloned α-subunits [104]; however, three subunits (Nav1.7, Nav1.8 and Nav1.9) meet the above criteria. Not surprisingly, many pharmaceutical companies are developing and testing subunit specific Nav1.7, NaV1.8 and NaV1.9 blockers as analgesics [38, 128].
The three α-subunits differ in their biophysical properties that determine their role in neuronal excitability [104]. The NaV1.9 channel activates over a negative range of membrane potentials close to the resting potential and generates a persistent current. Evidence suggests that it is powerfully regulated by G protein pathways, in a unique way. Therefore, when it is activated, it contributes to setting the resting membrane potentials of neurons expressing it [23]. Nav1.7 generates a transient Na+ current, but has a relatively slower rate of inactivation near the resting potential (slow closed-state inactivation) allowing the channel to generate persistent currents and making it a so-called threshold channel [22, 25]. Nav1.8 has a relatively depolarised activation voltage (~ − 20 mV) compared with Nav1.7 and Nav1.9 [2, 104]; thus, Nav1.8 activation comes after and perhaps subsequent to the activation of Nav1.9 and Nav1.7 channels. Nonetheless, Nav1.8’s depolarised inactivation and more rapid recovery from inactivation allow it to contribute to repetitive firing, for example [104]. This review will focus on NaV1.9 and Nav1.7 subunits since their biophysical properties allow them both to influence pain thresholds through setting the membrane potential and action potential threshold in DRG neurons.
Role of Nav1.7 in pain
Nav1.7 was cloned from PC12 cells in 1997 [118]. At that time, NaV1.8 and NaV1.3 channels were already under the spotlight and their role in pain was actively being investigated. NaV1.8 was cloned in 1996 and its strong expression in medium and small sensory neurons (the sizes of most nociceptors) made it the best and most obvious target for analgesic drug development [2]. The NaV1.8 knockout mouse was reported 3 years later and although it showed a pain deficit, its phenotype was compromised by a compensatory upregulation of Nav1.7 [3] with clear functional consequences [3, 89]. However, knockdown of NaV1.8 by antisense oligonucleotides in adult rats inhibited neuropathic pain [75, 129]. The difference could be due to the timing of the deletion (embryonic versus adult) or the animal model used (mouse versus rat). In contrast to Nav1.8, the expression pattern of Nav1.3 does not suggest it would be a useful drug target. Nav1.3 is expressed throughout the nervous system and its expression is highest during embryonic development and decreases postnatally [121]. However, Nav1.3 is the only channel that is re-expressed in DRG following nerve injury and diabetes [122]. This made it a potentially viable target for analgesics. However, mice lacking Nav1.3 do not show any deficits in pain phenotype [92].
Nav1.7 became the focus of the pain field in 2004 with the publication of two papers [91, 125]. The first paper identified a mutation in SCN9A (the gene coding for Nav1.7) as the cause for a rare inherited pain condition known as primary erythromelalgia (PEM). PEM symptoms start at early age with episodes of pain in the extremities (usually in the feet) that are triggered by exposure to heat or walking [125]. The second paper reported the complete absence of inflammatory pain in a conditional mouse lacking Nav1.7 in most nociceptors [91]. The conditional ablation in nociceptors was achieved using a Cre driver mouse line where Cre is expressed by the Nav1.8 promotor [113]. The complete loss of all inflammatory pain and mechanical pressure after ablation of Nav1.7 in nociceptors [91] excited the pain field and stimulated drug discovery programmes at several pharmaceutical companies [38, 128]. A conditional mouse was generated because global deletion of Nav1.7 in mouse proved to be lethal [91]. Global knockout pups were born alive but failed to feed and died within 24 h. Hand feeding and special husbandry arrangements allow Nav1.7 global KOs to survive to adulthood [49]. Inducing Nav1.7 ablation in adult mice causes pain deficits without detrimental effects [107].
Remarkably, the symptoms of PEM patients complemented the phenotype of the conditional Nav1.7 null mice. While pain can be triggered by mechanical pressure on the feet (walking and exercise), conditional null mutants showed a complete loss of pain to mechanical pressure. While PEM patients showed signs of inflammatory pain (heat, redness and occasionally swelling of the feet), conditional null showed a complete loss of inflammatory pain. This helped support the hypothesis that blocking Nav1.7 in humans would significantly reduce pain signalling. However, the mouse study raised significant questions. Firstly, is the role of Nav1.7 in pain signalling in humans as critical as it is in mice, or in other words, would the loss or block of Nav1.7 in humans lead to the all or none loss of pain seen in mice? Furthermore, if this is the case, then would the loss or block of Nav1.7 in humans result in lethality (as it did in mice)? These questions were critical for the validity of Nav1.7 as a drug target. These questions were answered in 2006 when it was reported that a loss of function mutation in SCN9A causes complete insensitivity to pain (CIP) [19]. In CIP patients, perception of non-noxious touch and warmth is not affected, whereas perception of noxious heat, pressure and injury pain is completely lost. CIP patients confirmed that Nav1.7 plays as a critical role in pain signalling in humans as it does in mice. Importantly, loss of Nav1.7 did not lead to lethality nor any significant disability (CIP patients are anosmic due to the expression of Nav1.7 in the olfactory epithelia [135]). A second heritable painful condition was mapped to a gain of function mutation in SCN9A in the same year (2006). Paroxysmal extreme pain disorder (PEPD, initially known as familial rectal pain), was found to be caused by a gain of function mutation in the Nav1.7 channel [45]. The four papers between 2004 and 2006 provided very strong evidence that Nav1.7 is a critical player in pain signalling, catapulting it to the top of the list of analgesic drug targets. Since then, human geneticists have identified scores of mutations causing PEM, PEPD, CIP and small fibre neuropathy (SFN).
Primary Erythromelalgia
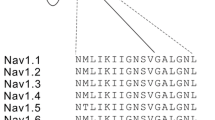
Primary erythromelalgia is an autosomal dominant condition caused by a mutation in the SCN9A gene. The condition was first mapped to SCN9A in 2004 by Yang et al. [125]. The proband suffered from bilateral episodes of burning pain in their hands and feet that started during their childhood and continued throughout their life. During the attacks, the feet and hands became warm and red. The pain episodes were triggered by exercise or exposure to heat. The proband had the nonsense mutation L858H which is located in the second domain, Fig. 1. Characterisation of the channel’s biophysical properties showed that the mutation shifted the activation voltage about 12 mV in the hyperpolarising direction resulting in a reduced threshold for channel opening and thus increased excitability [24]. Since the first report, several mutations have been reported that cause PEM, listed in Table 1 in chronological order. Symptoms appear early in life although late onset cases have been reported [16, 21]. All PEM mutations cause similar changes to the biophysical properties of Nav1.7, involving a shift of the activation voltage to hyperpolarised potentials [30], and where the magnitude of the shift seems to affect the severity of the symptoms [55]. Furthermore, PEM mutations tend to cluster in domains I and II of the channel protein, Fig. 1.
Topological representation of SCN9A mutations that cause PEM. A VGSC α-subunit consists of four homologous domains (DI-DIV). Each domain consists of six transmembrane segments. Three intracellular loops (L1-L2) connect the four domains. Note that most mutations are localised to domains I and II. Structures are not drawn to scale
Treatment for PEM patients includes avoidance of the conditions that trigger pain (i.e. heat and physical pressure on the feet). Patients typically resort to foot lifting, cooling feet by fans or immersing them in water or iced water to reduce or relief pain. Although immersion in cold water is effective for mild cases, it can result in ulceration and maceration of foot skin leading to infection [19, 116]. Recently, it has been reported that behavioural therapy reduced dependence on water immersion in PEM patients [67]. There is no consensus on pharmacotherapy. Among effective drugs are non-selective sodium blockers (lignocaine, mexiletine and carbamazepine) [82, 116] which have been shown to inhibit NaV1.7 [120, 133].
Paroxysmal extreme pain disorder
Paroxysmal extreme pain disorder (PEPD, formerly known as familial rectal pain syndrome), is caused by gain of function mutations in SCN9A that alter the biophysical properties of the Nav1.7 channel [45]. There are several similarities between PEPD and PEM. Both are autosomal dominant conditions with symptoms starting early in childhood (PEPD is observed in infants [17]). PEPD is characterised by episodes of severe burning pain in the rectal, ocular and mandibular areas accompanied by flushing of the skin. Pain in PEPD patients is triggered by otherwise innocuous mechanical stimulation (defecating, chewing and yawning) and warmth of the affected areas. However, functional characterisation of mutant Nav1.7 channels showed that they have normal activation voltages (unlike PEM mutations). In contrast, PEPD mutations cause a depolarising shift in inactivation voltages with incomplete channel inactivation, leading to a persistent current and increased excitability [7, 45, 119]. Table 2 lists reported SCN9A mutations that are found in PEPD patients. PEPD mutations tend to cluster in domains III and IV of the channel protein, Fig. 2. Despite the severity of the pain, PEPD patients responded well to the anti-epileptic drug carbamazepine [117].
Heritable small fibre neuropathy
Small fibre neuropathy (SFN) is caused by damage to thinly myelinated and unmyelinated nerve fibres. SFN is often characterised by late onset, bilateral burning pain to the hands and feet. SFN is also associated with disturbances to autonomic functions like sweating, dryness in the eyes or mouth and disturbance to bowel and bladder functions [117]. Autonomic symptoms are not reported in both PEM and PEPD. Diagnosis is usually confirmed by a decrease in intra-epidermal fibre density (IDFD) in skin biopsies. Several conditions can cause SFN, and these include diabetes and autoimmune disease [52, 112]. About 50% of SFN cases are idiopathic, with no obvious aetiology [112]. The dominant pattern of inheritance of SFN in some cases of idiopathic SFN suggested mutations in a single gene [52, 112]. Mutations in the three peripheral VGSCs, Nav1.7 [10], Nav1.8 [44] and Nav1.9 [63] channels, have been found in heritable SFN cases.
Characterisation of Nav1.7 channels in SFN patients, listed in Table 3, showed that they would cause hyperexcitability [43, 62]; however, it is not clear how this leads to a small fibre neuropathy and why it is of late onset. Nav1.7 channel mutations linked to SFN are not localised to a particular region within the channel but many are clustered in the first intracellular loop between domains I and II, Fig. 3. Recently a clinical trial has found lacosamide to be efficacious in reducing pain and well-being of SFN patients with SCN9A mutations [27]; however, the effect was linked to subset of SCN9A mutations [74].
Role of Nav1.7 in epilepsies
Although the expression of Nav1.7 in the human brain is poorly characterised, there is emerging evidence that Nav1.7 plays some role in modulating excitability in the brain. It is known that CIP patients suffer from the loss of the sense of smell due to expression of Nav1.7 in the olfactory epithelia [135] and a patient with the PEM mutation N1245S displayed high olfactory sensitivity [54]. However, CIP patients are not reported to suffer from brain-related symptoms. Nonetheless, several papers have recently reported mutations in SCN9A in patients with various types of epilepsies, Table 4. These mutations are mostly localised to the DI-DII part of the channel, Fig. 4. The above suggests that while a loss of Nav1.7 function has no detrimental effect on the brain, altered or increased Nav1.7 function does. Therefore, further research is needed to provide insights onto the type of cells that express Nav1.7 (types of neurons? any in glia?) in the brain. Furthermore, knock-in models will help to explore how the mutations cause epilepsy rather than act as modifiers to changes in other genes (e.g. SCN1A, SCN2A and SCN3A). Finally, it is intriguing that a few mutations (e.g. Q10R) cause PEM in some patients, and epilepsy in others. This may suggest that variations in the functional expression of other genes or epigenetic changes influence the biological consequences of mutations in Nav1.7.
Complete insensitivity to pain
Complete insensitivity to pain is characterised by loss of all pain sensations throughout patient’s life. SCN9A loss of function mutations cause an autosomal recessive CIP [19, 34]. Several mutations have been identified, and most are non-sense mutations causing truncated proteins, Table 5. Most of the mutations are located within domains I and II, Fig. 5. There is recent evidence that the CIP phenotype involves changes to endogenous opioids [87, 97]; however, this was not observed in a rat null model [14].
Role of Nav1.9 in pain
Nav1.9 (gene name SCN11A) is a tetrodotoxin-resistant (TTX-r), so-called persistent Na+ current, with clear evidence for functional expression in nociceptive primary sensory neurons in the dorsal root ganglia (DRG) and trigeminal (e.g. [6, 23]), and the AH cells of the myenteric plexus in the gut [18, 102]. The human clone (first named as SCN12A, 73% identical with rat SCN11A) [68] had initial reported expression in the placenta, spleen, small intestine, spinal cord and brain (potentially neurons and glia). In primary sensory neurons, it has been associated with nerve endings in the tooth pulp and cornea using immunohistochemical methods, and evidence suggests it is found distributed along IB4+ axons in the sciatic nerve (e.g. [28, 47, 95]); furthermore, the channel have been located to gut afferents [60, 61] and also to the bladder [101] using electrophysiological methods in gene knockout mice.
The functional properties of the channel currents were first identified in Nav1.8 knockout mouse sensory neurons, because under these circumstances, the channel generates the only tetrodotoxin-resistant (TTX-r) Na+ current [23, 84]. The channel produces a Na+ current in sensory neuron cell bodies that has ultra-slow activation and inactivation kinetics. It gives rise to a persistent, non-inactivating current operating over the negative portion of its activation membrane potential range, allowing it to act as a ‘threshold channel’, and to contribute to setting the membrane potential. Its unusual kinetic properties and negative activation range produce ‘plateau potentials’ that amplify applied or transduced sub-threshold depolarisations and massively prolong them in duration (Fig. 6). It is worth noting that Nav1.9 has activation kinetics that are too slow to directly contribute to impulse firing.
a Upregulation of Nav1.9 in an Nav1.8 knockout neuron, following the introduction of 500 μM GTP-γ-S into the cell interior for 12 min. b Upregulation of Nav1.9 using intracellular GTP-γ-S gives rise to changes in the firing properties of Nav1.8 knockout neuron, with reductions in current and voltage threshold, recorded from a holding potential of − 90 mV. The upregulated current gives rise to plateau potentials (arrow). Reproduced from [6], with permission
Intracellular dialysis of the non-hydrolysable GTP analogue, GTP-γ-S, upregulated the Nav1.9 current with no changes in current kinetics, recorded in voltage-clamp. It was also found that at a membrane potential of near − 60 mV, functional upregulation of the current can cause sensory neurons to fire rhythmically and spontaneously, at low frequency (Fig. 6) [6]. The current could be upregulated following the activation of ATP receptors, deduced to be P2Y, operating through a probable Gq/11 pathway and PKC [5, 6], and such a pathway has later been confirmed to be a contributor to modifying the firing properties of gut afferents.
There are several mouse knockouts of SCN11A reported in the literature and these have been associated with an elimination of the GTP-γ-S-upregulated current in primary sensory neurons [94] and a complementary reduction in forms of inflammatory pain following exposure to PGE2 [4] and including the formalin and CFA tests [99]—consistent with a role of Nav1.9 in inflammatory pain in both the skin and gut. A likely role for Nav1.9 in the control of normal gut motility, attributable to altered plexus function, seems consistent with the effects of mutation in human carriers and gain of function is associated with constipation (e.g. [69]). With these facts in mind, it may be possible to understand the defects in pain signalling found in humans with rare, heritable mutations in SCN11A.
Painful and painless Nav1.9 channelopathies
About 20 mutations have been reported for SCN11A, Table 6. All follow a dominant inheritance pattern. Most mutations have been confirmed to lead to a gain of function. No loss of function mutations have been reported to date which could be because such mutations cause mild or no effect on pain signalling in humans (given the phenotype of knockout mice, it is very unlikely that human loss of function mutation causes lethality). It is also possible that the loss or reduction of inflammatory pain may mean such individuals are unlikely to have a reason to visit the doctor!
The persistent nature of Nav1.9 currents and the negative activation voltage dependence make the channel functionally unique. It is proposed to act as a threshold channel in peripheral nociceptors, so gain of function mutations associated with facilitated activation would be expected to give rise to painful neuropathy, because the threshold for action potential generation is reduced. Indeed, SCN11A mutations result in two painful conditions, familial episodic pain [65, 80, 93, 130] and painful small fibre neuropathy [48, 57, 63]. In familial episodic pain, painful episodes centre on regions on the arms and legs; in addition, there are age-related decreases of pain, suggesting real age-related changes in gene expression. Painful episodes (lasting 10 s of minutes) are associated with rainy days, cold temperature and commonly also fatigue; some are associated with gut motility symptoms. Further, drugs acting as NSAIDs or anti-pyretics, such as ibuprofen, appear to be able to ameliorate these symptoms. Patients with SCN11A-related small fibre neuropathy experience pain, tingling and numbness in their arms and legs. Patients may experience diarrhoea which is consistent with expression of Nav1.9 in the gut [130].
Surprisingly, a few SCN11A gain of function mutations cause a complete insensitivity to pain [70, 79, 98]. Several possible explanations for how enhanced channel function leads to reduced neuronal excitability have been suggested [31], although arguments concerning modifications of channel-gating kinetics as the primary cause seem incomplete and are based on voltage-clamp recordings whose interpretation may not be straightforward. It is thought that increased activation/inactivation-gating overlap (or window current) depolarise the Nav1.9 expressing neurons. This prolonged depolarisation causes rapidly gating Na+ channels (e.g. Nav1.7 and Nav1.8) to enter the inactivated state [64]. Since these channels underpin action potential generation and propagation, the depolarizing block of Nav1.7 and Nav1.8 in nerve endings leads to an overall decrease in excitability. It was noted that the mutations that lead to CIP are those that produced the largest shift in the activation threshold of the channel, whereas those that lead to familial episodic pain and painful small fibre neuropathy cause smaller shifts, Table 6 [31]. Also of note, SCN11A CIP mutations are all localised to transmembrane segment 6, Fig. 7. However, several issues are difficult to reconcile with the above explanation for the painless phenotype. Firstly, Nav1.9 is expressed in the IB4+ subset of neurons and not in all DRG neurons (at least in rodents). Therefore, a depolarising block in this subset of neurons alone is not expected to cause a complete loss of pain. Second, NaV1.8 which is expressed in most nociceptors (i.e. in same neurons as Nav1.9) is a channel known to operate at more depolarised membrane potentials and can maintain excitability, even in the face of a depolarised membrane potential [56, 103, 111, 134].
Concluding remarks
In the past 20 years, mouse models and human genetics have confirmed that Nav1.7 and Nav1.9 play critical roles in pain signalling. The link between genotype and phenotype for mutations in both channels is poorly understood. Symptoms manifest in the extremities (mainly in the feet/legs) in most human conditions. In Nav1.7 channel mutations, there is a link between mutations that cause enhancement of activation to PEM and mutations that cause incomplete inactivation to PEPD. The physiological or microanatomical basis for these associations in terms of nerve ending function is only partly understood. In NaV1.9 channel mutations, a clear understanding of why most gain of function mutations cause painful conditions while those affecting segment 6 cause insensitivity to pain is also lacking, although insensitivity to pain is hypothesised to be caused by reduced excitability due to a depolarising block [121, 122].
Nonetheless, available evidence confirms a critical role for both channels in pain earning them a position in the list of potential drug targets. Ablation of Nav1.8 and Nav1.9 in mice does not lead to lethality or any observable detrimental effects. Ablation of Nav1.7 in human [19] and in adult mice [107] does not lead to lethality. Reassuringly, there are no reported respiratory or behavioural abnormalities as a result of the absence of any one of these three channels in mouse and human. Yet important challenges for VGSC blockers in chronic pain remain, developing subunit-specific blockers being the first. This is important considering that VGSC blockers would need to be administered regularly to treat chronic pain and perhaps at higher doses for breakthrough pain, when pain is severe. Therefore, VGSC blockers would need to be safe for long-term administration. The development of specific and effective small molecule inhibitors of Nav1.7 is still elusive, despite efforts by several pharmaceutical companies [38, 71, 128]. The second challenge is the extent of Nav1.7 inhibition required for analgesia in vivo. Given that CIP carriers have normal pain phenotype, an Nav1.7 blocker may need to reduce channel activity to a level well below 50% to produce analgesia.
The contribution of the endogenous opioid system to the phenotype of the SCN9A CIP raises the question of whether the CIP phenotype is a direct consequence of the loss of Nav1.7 [87, 97]. Several papers have provided complementary evidence that the loss of Nav1.7 reduces the excitability of DRG neurons per se. Deletion of Nav1.7 causes an increase in action potential threshold in small-diameter DRG neurons [107]. Deletion of Nav1.7 causes a major decrease in DRG neuron responsiveness to the VGSC opener veratridine [89]. Mechanically evoked spiking of C-fibres in the skin-nerve preparation was reduced in Nav1.7 KO mice [49]. No changes in the expression of other VGSC channels were reported in the Nav1.7 KO mouse to contribute to the observed reduced excitability of DRG [107]. Furthermore, pain deficits in a rat model of NaV1.7 deletion were not reversed by the opioid receptor antagonist naloxone [14]. Therefore, although an increase in spinal cord opioid synthesis would reduce signal transmission at the first synapse in CIP patients, the loss of NaV1.7 has a profound effect on the excitability of DRG neurons (i.e. expected to affect the initiation of the pain signal in the periphery).
The lack of reported Nav1.9 loss of function mutations may indicate that its loss does not lead to a major phenotype in humans, or at least does not make people go to the doctor, raising doubts as to whether a blocker would lead to a major analgesic effect. Finally, considering that nociceptors express at least two of the peripheral VGSC subunits (Nav1.7, Nav1.8 and Nav1.9), an effective analgesic strategy may ultimately result from a combination of blockers against these subunits to have additive and synergistic effects on nociceptors. The effectiveness of various drug combinations to reduce neuronal excitability can only be measured in DRG neurons because they express the target VGSCs at biologically relevant levels. Equally important, for the evaluation of any drug combination, is the potential effects on non-nociceptors as well as nociceptors. We recently described a relevant assay [88] and provided proof-of-concept data that showed a combination of Nav1.7 and Nav1.8 blockers produced a reduction in the excitability of DRG neurons close to that measured in Nav1.7 KO [89]. Changing the constituents and doses in VGSC blocker combinations may enable clinicians to manage chronic pain safely over the long term.
References
Ahn HS, Dib-Hajj SD, Cox JJ, Tyrrell L, Elmslie FV, Clarke AA, Drenth JP, Woods CG, Waxman SG (2010) A new Nav1.7 sodium channel mutation I234T in a child with severe pain. Eur J Pain 14:944–950. https://doi.org/10.1016/j.ejpain.2010.03.007
Akopian AN, Sivilotti L, Wood JN (1996) A tetrodotoxin-resistant voltage-gated sodium channel expressed by sensory neurons. Nature 379:257–262. https://doi.org/10.1038/379257a0
Akopian AN, Souslova V, England S, Okuse K, Ogata N, Ure J, Smith A, Kerr BJ, McMahon SB, Boyce S, Hill R, Stanfa LC, Dickenson AH, Wood JN (1999) The tetrodotoxin-resistant sodium channel SNS has a specialized function in pain pathways. Nat Neurosci 2:541–548. https://doi.org/10.1038/9195
Amaya F, Wang H, Costigan M, Allchorne AJ, Hatcher JP, Egerton J, Stean T, Morisset V, Grose D, Gunthorpe MJ, Chessell IP, Tate S, Green PJ, Woolf CJ (2006) The voltage-gated sodium channel Na(v)1.9 is an effector of peripheral inflammatory pain hypersensitivity. J Neurosci 26:12852–12860. https://doi.org/10.1523/JNEUROSCI.4015-06.2006
Baker MD (2005) Protein kinase C mediates up-regulation of tetrodotoxin-resistant, persistent Na+ current in rat and mouse sensory neurones. J Physiol 567:851–867. https://doi.org/10.1113/jphysiol.2005.089771
Baker MD, Chandra SY, Ding Y, Waxman SG, Wood JN (2003) GTP-induced tetrodotoxin-resistant Na+ current regulates excitability in mouse and rat small diameter sensory neurones. J Physiol 548:373–382. https://doi.org/10.1113/jphysiol.2003.039131
Bennett DL, Woods CG (2014) Painful and painless channelopathies. Lancet Neurol 13:587–599. https://doi.org/10.1016/S1474-4422(14)70024-9
Beyak MJ, Vanner S (2005) Inflammation-induced hyperexcitability of nociceptive gastrointestinal DRG neurones: the role of voltage-gated ion channels. Neurogastroenterol Motil 17:175–186. https://doi.org/10.1111/j.1365-2982.2004.00596.x
Breivik H, Collett B, Ventafridda V, Cohen R, Gallacher D (2006) Survey of chronic pain in Europe: prevalence, impact on daily life, and treatment. Eur J Pain 10:287–333. https://doi.org/10.1016/j.ejpain.2005.06.009
Brouwer BA, Merkies IS, Gerrits MM, Waxman SG, Hoeijmakers JG, Faber CG (2014) Painful neuropathies: the emerging role of sodium channelopathies. J Peripher Nerv Syst 19:53–65. https://doi.org/10.1111/jns5.12071
Caterina MJ, Pang Z (2016) TRP channels in skin biology and pathophysiology. Pharmaceuticals (Basel) 9. https://doi.org/10.3390/ph9040077
Catterall WA (2017) Forty years of sodium channels: structure, function, pharmacology, and epilepsy. Neurochem Res 42:2495–2504. https://doi.org/10.1007/s11064-017-2314-9
Cen Z, Lou Y, Guo Y, Wang J, Feng J (2017) Q10R mutation in SCN9A gene is associated with generalized epilepsy with febrile seizures plus. Seizure 50:186–188. https://doi.org/10.1016/j.seizure.2017.06.023
Chen L, Effraim P, Carrara J, Zhao P, Dib-Hajj FB, Dib-Hajj SD, Waxman SG (2020) Pharmacological characterization of a rat Nav1.7 loss-of-function model with insensitivity to pain. Pain. https://doi.org/10.1097/j.pain.0000000000001807
Cheng X, Dib-Hajj SD, Tyrrell L, Te Morsche RH, Drenth JP, Waxman SG (2011) Deletion mutation of sodium channel Na(V)1.7 in inherited erythromelalgia: enhanced slow inactivation modulates dorsal root ganglion neuron hyperexcitability. Brain 134:1972–1986. https://doi.org/10.1093/brain/awr143
Choi JS, Cheng X, Foster E, Leffler A, Tyrrell L, Te Morsche RH, Eastman EM, Jansen HJ, Huehne K, Nau C, Dib-Hajj SD, Drenth JP, Waxman SG (2010) Alternative splicing may contribute to time-dependent manifestation of inherited erythromelalgia. Brain 133:1823–1835. https://doi.org/10.1093/brain/awq114
Choi JS, Boralevi F, Brissaud O, Sanchez-Martin J, Te Morsche RH, Dib-Hajj SD, Drenth JP, Waxman SG (2011) Paroxysmal extreme pain disorder: a molecular lesion of peripheral neurons. Nat Rev Neurol 7:51–55. https://doi.org/10.1038/nrneurol.2010.162
Coste B, Osorio N, Padilla F, Crest M, Delmas P (2004) Gating and modulation of presumptive NaV1.9 channels in enteric and spinal sensory neurons. Mol Cell Neurosci 26:123–134. https://doi.org/10.1016/j.mcn.2004.01.015
Cox JJ, Reimann F, Nicholas AK, Thornton G, Roberts E, Springell K, Karbani G, Jafri H, Mannan J, Raashid Y, Al-Gazali L, Hamamy H, Valente EM, Gorman S, Williams R, McHale DP, Wood JN, Gribble FM, Woods CG (2006) An SCN9A channelopathy causes congenital inability to experience pain. Nature 444:894–898. https://doi.org/10.1038/nature05413
Cox JJ, Sheynin J, Shorer Z, Reimann F, Nicholas AK, Zubovic L, Baralle M, Wraige E, Manor E, Levy J, Woods CG, Parvari R (2010) Congenital insensitivity to pain: novel SCN9A missense and in-frame deletion mutations. Hum Mutat 31:E1670–E1686. https://doi.org/10.1002/humu.21325
Cregg R, Laguda B, Werdehausen R, Cox JJ, Linley JE, Ramirez JD, Bodi I, Markiewicz M, Howell KJ, Chen YC, Agnew K, Houlden H, Lunn MP, Bennett DL, Wood JN, Kinali M (2013) Novel mutations mapping to the fourth sodium channel domain of Nav1.7 result in variable clinical manifestations of primary erythromelalgia. NeuroMolecular Med 15:265–278. https://doi.org/10.1007/s12017-012-8216-8
Cummins TR, Howe JR, Waxman SG (1998) Slow closed-state inactivation: a novel mechanism underlying ramp currents in cells expressing the hNE/PN1 sodium channel. J Neurosci 18:9607–9619
Cummins TR, Dib-Hajj SD, Black JA, Akopian AN, Wood JN, Waxman SG (1999) A novel persistent tetrodotoxin-resistant sodium current in SNS-null and wild-type small primary sensory neurons. J Neurosci 19:RC43
Cummins TR, Dib-Hajj SD, Waxman SG (2004) Electrophysiological properties of mutant Nav1.7 sodium channels in a painful inherited neuropathy. J Neurosci 24:8232–8236. https://doi.org/10.1523/JNEUROSCI.2695-04.2004
Cummins TR, Sheets PL, Waxman SG (2007) The roles of sodium channels in nociception: implications for mechanisms of pain. Pain 131:243–257. https://doi.org/10.1016/j.pain.2007.07.026
Dabby R, Sadeh M, Gilad R, Lampl Y, Cohen S, Inbar S, Leshinsky-Silver E (2011) Chronic non-paroxysmal neuropathic pain-novel phenotype of mutation in the sodium channel SCN9A gene. J Neurol Sci 301:90–92. https://doi.org/10.1016/j.jns.2010.10.006
de Greef BTA, Hoeijmakers JGJ, Geerts M, Oakes M, Church TJE, Waxman SG, Dib-Hajj SD, Faber CG, Merkies ISJ (2019) Lacosamide in patients with Nav1.7 mutations-related small fibre neuropathy: a randomized controlled trial. Brain 142:263–275. https://doi.org/10.1093/brain/awy329
Dib-Hajj S, Black JA, Cummins TR, Waxman SG (2002) NaN/Nav1.9: a sodium channel with unique properties. Trends Neurosci 25:253–259. https://doi.org/10.1016/s0166-2236(02)02150-1
Dib-Hajj SD, Rush AM, Cummins TR, Hisama FM, Novella S, Tyrrell L, Marshall L, Waxman SG (2005) Gain-of-function mutation in Nav1.7 in familial erythromelalgia induces bursting of sensory neurons. Brain 128:1847–1854. https://doi.org/10.1093/brain/awh514
Dib-Hajj SD, Cummins TR, Black JA, Waxman SG (2007) From genes to pain: Na v 1.7 and human pain disorders. Trends Neurosci 30:555–563. https://doi.org/10.1016/j.tins.2007.08.004
Dib-Hajj SD, Black JA, Waxman SG (2015) NaV1.9: a sodium channel linked to human pain. Nat Rev Neurosci 16:511–519. https://doi.org/10.1038/nrn3977
Ding J, Zhang JW, Guo YX, Zhang YX, Chen ZH, Zhai QX (2019) Novel mutations in SCN9A occurring with fever-associated seizures or epilepsy. Seizure 71:214–218. https://doi.org/10.1016/j.seizure.2019.06.005
Drenth JP, te Morsche RH, Guillet G, Taieb A, Kirby RL, Jansen JB (2005) SCN9A mutations define primary erythermalgia as a neuropathic disorder of voltage gated sodium channels. J Invest Dermatol 124:1333–1338. https://doi.org/10.1111/j.0022-202X.2005.23737.x
Drissi I, Woods WA, Woods CG (2020) Understanding the genetic basis of congenital insensitivity to pain. Br Med Bull. https://doi.org/10.1093/bmb/ldaa003
Eberhardt M, Nakajima J, Klinger AB, Neacsu C, Huhne K, O’Reilly AO, Kist AM, Lampe AK, Fischer K, Gibson J, Nau C, Winterpacht A, Lampert A (2014) Inherited pain: sodium channel Nav1.7 A1632T mutation causes erythromelalgia due to a shift of fast inactivation. J Biol Chem 289:1971–1980. https://doi.org/10.1074/jbc.M113.502211
Eijkenboom I, Sopacua M, Hoeijmakers JGJ, de Greef BTA, Lindsey P, Almomani R, Marchi M, Vanoevelen J, Smeets HJM, Waxman SG, Lauria G, Merkies ISJ, Faber CG, Gerrits MM (2019) Yield of peripheral sodium channels gene screening in pure small fibre neuropathy. J Neurol Neurosurg Psychiatry 90:342–352. https://doi.org/10.1136/jnnp-2018-319042
Emery EC, Habib AM, Cox JJ, Nicholas AK, Gribble FM, Woods CG, Reimann F (2015) Novel SCN9A mutations underlying extreme pain phenotypes: unexpected electrophysiological and clinical phenotype correlations. J Neurosci 35:7674–7681. https://doi.org/10.1523/JNEUROSCI.3935-14.2015
Emery EC, Luiz AP, Wood JN (2016) Nav1.7 and other voltage-gated sodium channels as drug targets for pain relief. Expert Opin Ther Targets 20:975–983. https://doi.org/10.1517/14728222.2016.1162295
Estacion M, Dib-Hajj SD, Benke PJ, Te Morsche RH, Eastman EM, Macala LJ, Drenth JP, Waxman SG (2008) NaV1.7 gain-of-function mutations as a continuum: A1632E displays physiological changes associated with erythromelalgia and paroxysmal extreme pain disorder mutations and produces symptoms of both disorders. J Neurosci 28:11079–11088. https://doi.org/10.1523/JNEUROSCI.3443-08.2008
Estacion M, Choi JS, Eastman EM, Lin Z, Li Y, Tyrrell L, Yang Y, Dib-Hajj SD, Waxman SG (2010) Can robots patch-clamp as well as humans? Characterization of a novel sodium channel mutation. J Physiol 588:1915–1927. https://doi.org/10.1113/jphysiol.2009.186114
Estacion M, Han C, Choi JS, Hoeijmakers JG, Lauria G, Drenth JP, Gerrits MM, Dib-Hajj SD, Faber CG, Merkies IS, Waxman SG (2011) Intra- and interfamily phenotypic diversity in pain syndromes associated with a gain-of-function variant of NaV1.7. Mol Pain 7:92. https://doi.org/10.1186/1744-8069-7-92
Estacion M, Yang Y, Dib-Hajj SD, Tyrrell L, Lin Z, Yang Y, Waxman SG (2013) A new Nav1.7 mutation in an erythromelalgia patient. Biochem Biophys Res Commun 432:99–104. https://doi.org/10.1016/j.bbrc.2013.01.079
Faber CG, Hoeijmakers JG, Ahn HS, Cheng X, Han C, Choi JS, Estacion M, Lauria G, Vanhoutte EK, Gerrits MM, Dib-Hajj S, Drenth JP, Waxman SG, Merkies IS (2012) Gain of function Nanu1.7 mutations in idiopathic small fiber neuropathy. Ann Neurol 71:26–39. https://doi.org/10.1002/ana.22485
Faber CG, Lauria G, Merkies IS, Cheng X, Han C, Ahn HS, Persson AK, Hoeijmakers JG, Gerrits MM, Pierro T, Lombardi R, Kapetis D, Dib-Hajj SD, Waxman SG (2012) Gain-of-function Nav1.8 mutations in painful neuropathy. Proc Natl Acad Sci U S A 109:19444–19449. https://doi.org/10.1073/pnas.1216080109
Fertleman CR, Baker MD, Parker KA, Moffatt S, Elmslie FV, Abrahamsen B, Ostman J, Klugbauer N, Wood JN, Gardiner RM, Rees M (2006) SCN9A mutations in paroxysmal extreme pain disorder: allelic variants underlie distinct channel defects and phenotypes. Neuron 52:767–774. https://doi.org/10.1016/j.neuron.2006.10.006
Fischer TZ, Gilmore ES, Estacion M, Eastman E, Taylor S, Melanson M, Dib-Hajj SD, Waxman SG (2009) A novel Nav1.7 mutation producing carbamazepine-responsive erythromelalgia. Ann Neurol 65:733–741. https://doi.org/10.1002/ana.21678
Fjell J, Hjelmstrom P, Hormuzdiar W, Milenkovic M, Aglieco F, Tyrrell L, Dib-Hajj S, Waxman SG, Black JA (2000) Localization of the tetrodotoxin-resistant sodium channel NaN in nociceptors. Neuroreport 11:199–202. https://doi.org/10.1097/00001756-200001170-00039
Ginanneschi F, Rubegni A, Moro F, Volpi N, Santorelli FM, Rossi A (2019) SCN11A variant as possible pain generator in sensory axonal neuropathy. Neurol Sci 40:1295–1297. https://doi.org/10.1007/s10072-019-3703-4
Gingras J, Smith S, Matson DJ, Johnson D, Nye K, Couture L, Feric E, Yin R, Moyer BD, Peterson ML, Rottman JB, Beiler RJ, Malmberg AB, McDonough SI (2014) Global Nav1.7 knockout mice recapitulate the phenotype of human congenital indifference to pain. PLoS One 9:e105895. https://doi.org/10.1371/journal.pone.0105895
Goldberg DS, McGee SJ (2011) Pain as a global public health priority. BMC Public Health 11:770. https://doi.org/10.1186/1471-2458-11-770
Goldberg YP, MacFarlane J, MacDonald ML, Thompson J, Dube MP, Mattice M, Fraser R, Young C, Hossain S, Pape T, Payne B, Radomski C, Donaldson G, Ives E, Cox J, Younghusband HB, Green R, Duff A, Boltshauser E, Grinspan GA, Dimon JH, Sibley BG, Andria G, Toscano E, Kerdraon J, Bowsher D, Pimstone SN, Samuels ME, Sherrington R, Hayden MR (2007) Loss-of-function mutations in the Nav1.7 gene underlie congenital indifference to pain in multiple human populations. Clin Genet 71:311–319. https://doi.org/10.1111/j.1399-0004.2007.00790.x
Gwathmey KG, Pearson KT (2019) Diagnosis and management of sensory polyneuropathy. BMJ 365:l1108. https://doi.org/10.1136/bmj.l1108
Haberberger RV, Barry C, Dominguez N, Matusica D (2019) Human dorsal root ganglia. Front Cell Neurosci 13:271. https://doi.org/10.3389/fncel.2019.00271
Haehner A, Hummel T, Heinritz W, Krueger S, Meinhardt M, Whitcroft KL, Sabatowski R, Gossrau G (2018) Mutation in Nav 1.7 causes high olfactory sensitivity. Eur J Pain 22:1767–1773. https://doi.org/10.1002/ejp.1272
Han C, Dib-Hajj SD, Lin Z, Li Y, Eastman EM, Tyrrell L, Cao X, Yang Y, Waxman SG (2009) Early- and late-onset inherited erythromelalgia: genotype-phenotype correlation. Brain 132:1711–1722. https://doi.org/10.1093/brain/awp078
Han C, Hoeijmakers JG, Liu S, Gerrits MM, te Morsche RH, Lauria G, Dib-Hajj SD, Drenth JP, Faber CG, Merkies IS, Waxman SG (2012) Functional profiles of SCN9A variants in dorsal root ganglion neurons and superior cervical ganglion neurons correlate with autonomic symptoms in small fibre neuropathy. Brain 135:2613–2628. https://doi.org/10.1093/brain/aws187
Han C, Yang Y, de Greef BT, Hoeijmakers JG, Gerrits MM, Verhamme C, Qu J, Lauria G, Merkies IS, Faber CG, Dib-Hajj SD, Waxman SG (2015) The domain II S4-S5 linker in Nav1.9: a missense mutation enhances activation, impairs fast inactivation, and produces human painful neuropathy. NeuroMolecular Med 17:158–169. https://doi.org/10.1007/s12017-015-8347-9
Han C, Yang Y, Te Morsche RH, Drenth JP, Politei JM, Waxman SG, Dib-Hajj SD (2017) Familial gain-of-function Nav1.9 mutation in a painful channelopathy. J Neurol Neurosurg Psychiatry 88:233–240. https://doi.org/10.1136/jnnp-2016-313804
Harty TP, Dib-Hajj SD, Tyrrell L, Blackman R, Hisama FM, Rose JB, Waxman SG (2006) Na(V)1.7 mutant A863P in erythromelalgia: effects of altered activation and steady-state inactivation on excitability of nociceptive dorsal root ganglion neurons. J Neurosci 26:12566–12575. https://doi.org/10.1523/JNEUROSCI.3424-06.2006
Hockley JR, Boundouki G, Cibert-Goton V, McGuire C, Yip PK, Chan C, Tranter M, Wood JN, Nassar MA, Blackshaw LA, Aziz Q, Michael GJ, Baker MD, Winchester WJ, Knowles CH, Bulmer DC (2014) Multiple roles for NaV1.9 in the activation of visceral afferents by noxious inflammatory, mechanical, and human disease-derived stimuli. Pain 155:1962–1975. https://doi.org/10.1016/j.pain.2014.06.015
Hockley JR, Tranter MM, McGuire C, Boundouki G, Cibert-Goton V, Thaha MA, Blackshaw LA, Michael GJ, Baker MD, Knowles CH, Winchester WJ, Bulmer DC (2016) P2Y receptors sensitize mouse and human colonic nociceptors. J Neurosci 36:2364–2376. https://doi.org/10.1523/JNEUROSCI.3369-15.2016
Hoeijmakers JG, Han C, Merkies IS, Macala LJ, Lauria G, Gerrits MM, Dib-Hajj SD, Faber CG, Waxman SG (2012) Small nerve fibres, small hands and small feet: a new syndrome of pain, dysautonomia and acromesomelia in a kindred with a novel NaV1.7 mutation. Brain 135:345–358. https://doi.org/10.1093/brain/awr349
Huang J, Han C, Estacion M, Vasylyev D, Hoeijmakers JG, Gerrits MM, Tyrrell L, Lauria G, Faber CG, Dib-Hajj SD, Merkies IS, Waxman SG, Group PS (2014) Gain-of-function mutations in sodium channel Na(v)1.9 in painful neuropathy. Brain 137:1627–1642. https://doi.org/10.1093/brain/awu079
Huang J, Vanoye CG, Cutts A, Goldberg YP, Dib-Hajj SD, Cohen CJ, Waxman SG, George AL Jr (2017) Sodium channel NaV1.9 mutations associated with insensitivity to pain dampen neuronal excitability. J Clin Invest 127:2805–2814. https://doi.org/10.1172/JCI92373
Huang J, Estacion M, Zhao P, Dib-Hajj FB, Schulman B, Abicht A, Kurth I, Brockmann K, Waxman SG, Dib-Hajj SD (2019) A novel gain-of-function Nav1.9 mutation in a child with episodic pain. Front Neurosci 13:918. https://doi.org/10.3389/fnins.2019.00918
Imai N, Miyake N, Saito Y, Kobayashi E, Ikawa M, Manaka S, Shiina M, Ogata K, Matsumoto N (2015) Short-lasting unilateral neuralgiform headache attacks with ispilateral facial flushing is a new variant of paroxysmal extreme pain disorder. J Headache Pain 16:519. https://doi.org/10.1186/s10194-015-0519-3
Ito M, Yamaguchi S, Omine T, Miyagi T, Arakaki O, Yamamoto YI, Takahashi K (2019) Behavioral therapy ceased cold water immersion dependence in a patient with familial erythromelalgia caused by SCN9A mutation. JAAD Case Rep 5:806–808. https://doi.org/10.1016/j.jdcr.2019.07.007
Jeong SY, Goto J, Hashida H, Suzuki T, Ogata K, Masuda N, Hirai M, Isahara K, Uchiyama Y, Kanazawa I (2000) Identification of a novel human voltage-gated sodium channel alpha subunit gene, SCN12A. Biochem Biophys Res Commun 267:262–270. https://doi.org/10.1006/bbrc.1999.1916
Kabata R, Okuda H, Noguchi A, Kondo D, Fujiwara M, Hata K, Kato Y, Ishikawa K, Tanaka M, Sekine Y, Hishikawa N, Mizukami T, Ito J, Akasaka M, Sakurai K, Yoshida T, Minoura H, Hayashi T, Inoshita K, Matsuyama M, Kinjo N, Cao Y, Inoue S, Kobayashi H, Harada KH, Youssefian S, Takahashi T, Koizumi A (2018) Familial episodic limb pain in kindreds with novel Nav1.9 mutations. PLoS One 13:e0208516. https://doi.org/10.1371/journal.pone.0208516
King MK, Leipold E, Goehringer JM, Kurth I, Challman TD (2017) Pain insensitivity: distal S6-segment mutations in NaV1.9 emerge as critical hotspot. Neurogenetics 18:179–181. https://doi.org/10.1007/s10048-017-0513-9
Kingwell K (2019) Nav1.7 withholds its pain potential. Nat Rev Drug Discov. https://doi.org/10.1038/d41573-019-00065-0
Klein CJ, Wu Y, Kilfoyle DH, Sandroni P, Davis MD, Gavrilova RH, Low PA, Dyck PJ (2013) Infrequent SCN9A mutations in congenital insensitivity to pain and erythromelalgia. J Neurol Neurosurg Psychiatry 84:386–391. https://doi.org/10.1136/jnnp-2012-303719
Kurban M, Wajid M, Shimomura Y, Christiano AM (2010) A nonsense mutation in the SCN9A gene in congenital insensitivity to pain. Dermatology 221:179–183. https://doi.org/10.1159/000314692
Labau JIR, Estacion M, Tanaka BS, de Greef BTA, Hoeijmakers JGJ, Geerts M, Gerrits MM, Smeets HJM, Faber CG, Merkies ISJ, Lauria G, Dib-Hajj SD, Waxman SG (2020) Differential effect of lacosamide on Nav1.7 variants from responsive and non-responsive patients with small fibre neuropathy. Brain 143:771–782. https://doi.org/10.1093/brain/awaa016
Lai J, Gold MS, Kim CS, Bian D, Ossipov MH, Hunter JC, Porreca F (2002) Inhibition of neuropathic pain by decreased expression of the tetrodotoxin-resistant sodium channel, NaV1.8. Pain 95:143–152. https://doi.org/10.1016/s0304-3959(01)00391-8
Lampert A, Dib-Hajj SD, Eastman EM, Tyrrell L, Lin Z, Yang Y, Waxman SG (2009) Erythromelalgia mutation L823R shifts activation and inactivation of threshold sodium channel Nav1.7 to hyperpolarized potentials. Biochem Biophys Res Commun 390:319–324. https://doi.org/10.1016/j.bbrc.2009.09.121
Lawson SN (2002) Phenotype and function of somatic primary afferent nociceptive neurones with C-, adelta- or aalpha/beta-fibres. Exp Physiol 87:239–244. https://doi.org/10.1113/eph8702350
Lee MJ, Yu HS, Hsieh ST, Stephenson DA, Lu CJ, Yang CC (2007) Characterization of a familial case with primary erythromelalgia from Taiwan. J Neurol 254:210–214. https://doi.org/10.1007/s00415-006-0328-3
Leipold E, Liebmann L, Korenke GC, Heinrich T, Giesselmann S, Baets J, Ebbinghaus M, Goral RO, Stodberg T, Hennings JC, Bergmann M, Altmuller J, Thiele H, Wetzel A, Nurnberg P, Timmerman V, De Jonghe P, Blum R, Schaible HG, Weis J, Heinemann SH, Hubner CA, Kurth I (2013) A de novo gain-of-function mutation in SCN11A causes loss of pain perception. Nat Genet 45:1399–1404. https://doi.org/10.1038/ng.2767
Leipold E, Hanson-Kahn A, Frick M, Gong P, Bernstein JA, Voigt M, Katona I, Oliver Goral R, Altmuller J, Nurnberg P, Weis J, Hubner CA, Heinemann SH, Kurth I (2015) Cold-aggravated pain in humans caused by a hyperactive NaV1.9 channel mutant. Nat Commun 6:10049. https://doi.org/10.1038/ncomms10049
Liu Z, Ye X, Qiao P, Luo W, Wu Y, He Y, Gao P (2019) G327E mutation in SCN9A gene causes idiopathic focal epilepsy with Rolandic spikes: a case report of twin sisters. Neurol Sci 40:1457–1460. https://doi.org/10.1007/s10072-019-03752-3
Mann N, King T, Murphy R (2019) Review of primary and secondary erythromelalgia. Clin Exp Dermatol 44:477–482. https://doi.org/10.1111/ced.13891
Marchi M, Provitera V, Nolano M, Romano M, Maccora S, D’Amato I, Salvi E, Gerrits M, Santoro L, Lauria G (2018) A novel SCN9A splicing mutation in a compound heterozygous girl with congenital insensitivity to pain, hyposmia and hypogeusia. J Peripher Nerv Syst 23:202–206. https://doi.org/10.1111/jns.12280
Maruyama H, Yamamoto M, Matsutomi T, Zheng T, Nakata Y, Wood JN, Ogata N (2004) Electrophysiological characterization of the tetrodotoxin-resistant Na+ channel, Na(v)1.9, in mouse dorsal root ganglion neurons. Pflugers Arch 449:76–87. https://doi.org/10.1007/s00424-004-1315-0
Meglic A, Perkovic-Benedik M, Trebusak Podkrajsek K, Bertok S (2014) Painful micturition in a small child: an unusual clinical picture of paroxysmal extreme pain disorder. Pediatr Nephrol 29:1643–1646. https://doi.org/10.1007/s00467-014-2819-2
Michiels JJ, te Morsche RH, Jansen JB, Drenth JP (2005) Autosomal dominant erythermalgia associated with a novel mutation in the voltage-gated sodium channel alpha subunit Nav1.7. Arch Neurol 62:1587–1590. https://doi.org/10.1001/archneur.62.10.1587
Minett MS, Pereira V, Sikandar S, Matsuyama A, Lolignier S, Kanellopoulos AH, Mancini F, Iannetti GD, Bogdanov YD, Santana-Varela S, Millet Q, Baskozos G, MacAllister R, Cox JJ, Zhao J, Wood JN (2015) Endogenous opioids contribute to insensitivity to pain in humans and mice lacking sodium channel Nav1.7. Nat Commun 6:8967. https://doi.org/10.1038/ncomms9967
Mohammed ZA, Doran C, Grundy D, Nassar MA (2017) Veratridine produces distinct calcium response profiles in mouse dorsal root ganglia neurons. Sci Rep 7:45221. https://doi.org/10.1038/srep45221
Mohammed ZA, Kaloyanova K, Nassar MA (2020) An unbiased and efficient assessment of excitability of sensory neurons for analgesic drug discovery. Pain. 161:1100–1108. https://doi.org/10.1097/j.pain.0000000000001802
Moore C, Gupta R, Jordt SE, Chen Y, Liedtke WB (2018) Regulation of pain and itch by TRP channels. Neurosci Bull 34:120–142. https://doi.org/10.1007/s12264-017-0200-8
Nassar MA, Stirling LC, Forlani G, Baker MD, Matthews EA, Dickenson AH, Wood JN (2004) Nociceptor-specific gene deletion reveals a major role for Nav1.7 (PN1) in acute and inflammatory pain. Proc Natl Acad Sci U S A 101:12706–12711. https://doi.org/10.1073/pnas.0404915101
Nassar MA, Baker MD, Levato A, Ingram R, Mallucci G, McMahon SB, Wood JN (2006) Nerve injury induces robust allodynia and ectopic discharges in Nav1.3 null mutant mice. Mol Pain 2:33. https://doi.org/10.1186/1744-8069-2-33
Okuda H, Noguchi A, Kobayashi H, Kondo D, Harada KH, Youssefian S, Shioi H, Kabata R, Domon Y, Kubota K, Kitano Y, Takayama Y, Hitomi T, Ohno K, Saito Y, Asano T, Tominaga M, Takahashi T, Koizumi A (2016) Infantile pain episodes associated with novel Nav1.9 mutations in familial episodic pain syndrome in Japanese families. PLoS One 11:e0154827. https://doi.org/10.1371/journal.pone.0154827
Ostman JA, Nassar MA, Wood JN, Baker MD (2008) GTP up-regulated persistent Na+ current and enhanced nociceptor excitability require NaV1.9. J Physiol 586:1077–1087. https://doi.org/10.1113/jphysiol.2007.147942
Padilla F, Couble ML, Coste B, Maingret F, Clerc N, Crest M, Ritter AM, Magloire H, Delmas P (2007) Expression and localization of the Nav1.9 sodium channel in enteric neurons and in trigeminal sensory endings: implication for intestinal reflex function and orofacial pain. Mol Cell Neurosci 35:138–152. https://doi.org/10.1016/j.mcn.2007.02.008
Peddareddygari LR, Oberoi K, Grewal RP (2014) Congenital insensitivity to pain: a case report and review of the literature. Case Rep Neurol Med 2014:141953–141954. https://doi.org/10.1155/2014/141953
Pereira V, Millet Q, Aramburu J, Lopez-Rodriguez C, Gaveriaux-Ruff C, Wood JN (2018) Analgesia linked to Nav1.7 loss of function requires micro- and delta-opioid receptors. Wellcome Open Res 3:101. https://doi.org/10.12688/wellcomeopenres.14687.1
Phatarakijnirund V, Mumm S, McAlister WH, Novack DV, Wenkert D, Clements KL, Whyte MP (2016) Congenital insensitivity to pain: fracturing without apparent skeletal pathobiology caused by an autosomal dominant, second mutation in SCN11A encoding voltage-gated sodium channel 1.9. Bone 84:289–298. https://doi.org/10.1016/j.bone.2015.11.022
Priest BT, Murphy BA, Lindia JA, Diaz C, Abbadie C, Ritter AM, Liberator P, Iyer LM, Kash SF, Kohler MG, Kaczorowski GJ, MacIntyre DE, Martin WJ (2005) Contribution of the tetrodotoxin-resistant voltage-gated sodium channel NaV1.9 to sensory transmission and nociceptive behavior. Proc Natl Acad Sci U S A 102:9382–9387. https://doi.org/10.1073/pnas.0501549102
Rajasekharan S, Martens L, Domingues L, Cauwels R (2017) SCN9A channelopathy associated autosomal recessive congenital indifference to pain. A case report. Eur J Paediatr Dent 18:66–68. https://doi.org/10.23804/ejpd.2017.18.01.14
Ritter AM, Martin WJ, Thorneloe KS (2009) The voltage-gated sodium channel Nav1.9 is required for inflammation-based urinary bladder dysfunction. Neurosci Lett 452:28–32. https://doi.org/10.1016/j.neulet.2008.12.051
Rugiero F, Mistry M, Sage D, Black JA, Waxman SG, Crest M, Clerc N, Delmas P, Gola M (2003) Selective expression of a persistent tetrodotoxin-resistant Na+ current and NaV1.9 subunit in myenteric sensory neurons. J Neurosci 23:2715–2725
Rush AM, Dib-Hajj SD, Liu S, Cummins TR, Black JA, Waxman SG (2006) A single sodium channel mutation produces hyper- or hypoexcitability in different types of neurons. Proc Natl Acad Sci U S A 103:8245–8250. https://doi.org/10.1073/pnas.0602813103
Rush AM, Cummins TR, Waxman SG (2007) Multiple sodium channels and their roles in electrogenesis within dorsal root ganglion neurons. J Physiol 579:1–14. https://doi.org/10.1113/jphysiol.2006.121483
Sadler KE, Stucky CL (2019) Neuronal transient receptor potential (TRP) channels and noxious sensory detection in sickle cell disease. Neurosci Lett 694:184–191. https://doi.org/10.1016/j.neulet.2018.11.056
Sawal HA, Harripaul R, Mikhailov A, Dad R, Ayub M, Jawad Hassan M, Vincent JB (2016) Biallelic truncating SCN9A mutation identified in four families with congenital insensitivity to pain from Pakistan. Clin Genet 90:563–565. https://doi.org/10.1111/cge.12860
Shields SD, Deng L, Reese RM, Dourado M, Tao J, Foreman O, Chang JH, Hackos DH (2018) Insensitivity to pain upon adult-onset deletion of Nav1.7 or its blockade with selective inhibitors. J Neurosci 38:10180–10201. https://doi.org/10.1523/JNEUROSCI.1049-18.2018
Shorer Z, Wajsbrot E, Liran TH, Levy J, Parvari R (2014) A novel mutation in SCN9A in a child with congenital insensitivity to pain. Pediatr Neurol 50:73–76. https://doi.org/10.1016/j.pediatrneurol.2013.09.007
Singh NA, Pappas C, Dahle EJ, Claes LR, Pruess TH, De Jonghe P, Thompson J, Dixon M, Gurnett C, Peiffer A, White HS, Filloux F, Leppert MF (2009) A role of SCN9A in human epilepsies, as a cause of febrile seizures and as a potential modifier of Dravet syndrome. PLoS Genet 5:e1000649. https://doi.org/10.1371/journal.pgen.1000649
Skeik N, Rooke TW, Davis MD, Davis DM, Kalsi H, Kurth I, Richardson RC (2012) Severe case and literature review of primary erythromelalgia: novel SCN9A gene mutation. Vasc Med 17:44–49. https://doi.org/10.1177/1358863X11422584
Snape A, Pittaway JF, Baker MD (2010) Excitability parameters and sensitivity to anemone toxin ATX-II in rat small diameter primary sensory neurones discriminated by Griffonia simplicifolia isolectin IB4. J Physiol 588:125–137. https://doi.org/10.1113/jphysiol.2009.181107
Sopacua M, Hoeijmakers JGJ, Merkies ISJ, Lauria G, Waxman SG, Faber CG (2019) Small-fiber neuropathy: expanding the clinical pain universe. J Peripher Nerv Syst 24:19–33. https://doi.org/10.1111/jns.12298
Stirling LC, Forlani G, Baker MD, Wood JN, Matthews EA, Dickenson AH, Nassar MA (2005) Nociceptor-specific gene deletion using heterozygous NaV1.8-Cre recombinase mice. Pain 113:27–36. https://doi.org/10.1016/j.pain.2004.08.015
Suter MR, Bhuiyan ZA, Laedermann CJ, Kuntzer T, Schaller M, Stauffacher MW, Roulet E, Abriel H, Decosterd I, Wider C (2015) p.L1612P, a novel voltage-gated sodium channel Nav1.7 mutation inducing a cold sensitive paroxysmal extreme pain disorder. Anesthesiology 122:414–423. https://doi.org/10.1097/ALN.0000000000000476
Tanaka BS, Nguyen PT, Zhou EY, Yang Y, Yarov-Yarovoy V, Dib-Hajj SD, Waxman SG (2017) Gain-of-function mutation of a voltage-gated sodium channel NaV1.7 associated with peripheral pain and impaired limb development. J Biol Chem 292:9262–9272. https://doi.org/10.1074/jbc.M117.778779
Tham SW, Giles M (2018) Current pain management strategies for patients with erythromelalgia: a critical review. J Pain Res 11:1689–1698. https://doi.org/10.2147/JPR.S154462
Themistocleous AC, Ramirez JD, Serra J, Bennett DL (2014) The clinical approach to small fibre neuropathy and painful channelopathy. Pract Neurol 14:368–379. https://doi.org/10.1136/practneurol-2013-000758
Toledo-Aral JJ, Moss BL, He ZJ, Koszowski AG, Whisenand T, Levinson SR, Wolf JJ, Silos-Santiago I, Halegoua S, Mandel G (1997) Identification of PN1, a predominant voltage-dependent sodium channel expressed principally in peripheral neurons. Proc Natl Acad Sci U S A 94:1527–1532. https://doi.org/10.1073/pnas.94.4.1527
Vetter I, Deuis JR, Mueller A, Israel MR, Starobova H, Zhang A, Rash LD, Mobli M (2017) NaV1.7 as a pain target-from gene to pharmacology. Pharmacol Ther 172:73–100. https://doi.org/10.1016/j.pharmthera.2016.11.015
Wang Y, Mi J, Lu K, Lu Y, Wang K (2015) Comparison of gating properties and use-dependent block of Nav1.5 and Nav1.7 channels by anti-arrhythmics mexiletine and lidocaine. PLoS One 10:e0128653. https://doi.org/10.1371/journal.pone.0128653
Waxman SG, Kocsis JD, Black JA (1994) Type III sodium channel mRNA is expressed in embryonic but not adult spinal sensory neurons, and is reexpressed following axotomy. J Neurophysiol 72:466–470. https://doi.org/10.1152/jn.1994.72.1.466
Waxman SG, Dib-Hajj S, Cummins TR, Black JA (1999) Sodium channels and pain. Proc Natl Acad Sci U S A 96:7635–7639. https://doi.org/10.1073/pnas.96.14.7635
Wu MT, Huang PY, Yen CT, Chen CC, Lee MJ (2013) A novel SCN9A mutation responsible for primary erythromelalgia and is resistant to the treatment of sodium channel blockers. PLoS One 8:e55212. https://doi.org/10.1371/journal.pone.0055212
Wu B, Zhang Y, Tang H, Yang M, Long H, Shi G, Tang J, Shi X (2017) A novel SCN9A mutation (F826Y) in primary erythromelalgia alters the excitability of Nav1.7. Curr Mol Med 17:450–457. https://doi.org/10.2174/1566524017666171009105029
Yang Y, Wang Y, Li S, Xu Z, Li H, Ma L, Fan J, Bu D, Liu B, Fan Z, Wu G, Jin J, Ding B, Zhu X, Shen Y (2004) Mutations in SCN9A, encoding a sodium channel alpha subunit, in patients with primary erythermalgia. J Med Genet 41:171–174. https://doi.org/10.1136/jmg.2003.012153
Yang Y, Huang J, Mis MA, Estacion M, Macala L, Shah P, Schulman BR, Horton DB, Dib-Hajj SD, Waxman SG (2016) Nav1.7-A1632G mutation from a family with inherited erythromelalgia: enhanced firing of dorsal root ganglia neurons evoked by thermal stimuli. J Neurosci 36:7511–7522. https://doi.org/10.1523/JNEUROSCI.0462-16.2016
Yang C, Hua Y, Zhang W, Xu J, Xu L, Gao F, Jiang P (2018) Variable epilepsy phenotypes associated with heterozygous mutation in the SCN9A gene: report of two cases. Neurol Sci 39:1113–1115. https://doi.org/10.1007/s10072-018-3300-y
Yekkirala AS, Roberson DP, Bean BP, Woolf CJ (2017) Breaking barriers to novel analgesic drug development. Nat Rev Drug Discov 16:545–564. https://doi.org/10.1038/nrd.2017.87
Yu YQ, Zhao F, Guan SM, Chen J (2011) Antisense-mediated knockdown of Na(V)1.8, but not Na(V)1.9, generates inhibitory effects on complete Freund’s adjuvant-induced inflammatory pain in rat. PLoS One 6:e19865. https://doi.org/10.1371/journal.pone.0019865
Zhang XY, Wen J, Yang W, Wang C, Gao L, Zheng LH, Wang T, Ran K, Li Y, Li X, Xu M, Luo J, Feng S, Ma X, Ma H, Chai Z, Zhou Z, Yao J, Zhang X, Liu JY (2013) Gain-of-function mutations in SCN11A cause familial episodic pain. Am J Hum Genet 93:957–966. https://doi.org/10.1016/j.ajhg.2013.09.016
Zhang Z, Schmelz M, Segerdahl M, Quiding H, Centerholt C, Jureus A, Carr TH, Whiteley J, Salter H, Kvernebo MS, Orstavik K, Helas T, Kleggetveit IP, Lunden LK, Jorum E (2014) Exonic mutations in SCN9A (NaV1.7) are found in a minority of patients with erythromelalgia. Scand J Pain 5:217–225. https://doi.org/10.1016/j.sjpain.2014.09.002
Zhang T, Chen M, Zhu A, Zhang X, Fang T (2020) Novel mutation of SCN9A gene causing generalized epilepsy with febrile seizures plus in a Chinese family. Neurol Sci. https://doi.org/10.1007/s10072-020-04284-x
Zhao F, Li X, Jin L, Zhang F, Inoue M, Yu B, Cao Z (2016) Development of a rapid throughput assay for identification of hNav1.7 antagonist using unique efficacious sodium channel agonist, antillatoxin. Mar Drugs 14. https://doi.org/10.3390/md14020036
Zimmermann K, Leffler A, Babes A, Cendan CM, Carr RW, Kobayashi J, Nau C, Wood JN, Reeh PW (2007) Sensory neuron sodium channel Nav1.8 is essential for pain at low temperatures. Nature 447:855–858. https://doi.org/10.1038/nature05880
Zufall F, Pyrski M, Weiss J, Leinders-Zufall T (2012) Link between pain and olfaction in an inherited sodium channelopathy. Arch Neurol 69:1119–1123. https://doi.org/10.1001/archneurol.2012.21
Acknowledgements
MAN is grateful to Yusef Nassar for the proof reading and suggestions on the manuscript.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the special issue on Channelopathies: from mutation to diseases in Pflügers Archiv—European Journal of Physiology
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Baker, M.D., Nassar, M.A. Painful and painless mutations of SCN9A and SCN11A voltage-gated sodium channels. Pflugers Arch - Eur J Physiol 472, 865–880 (2020). https://doi.org/10.1007/s00424-020-02419-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00424-020-02419-9