Abstract
Purpose
To explore the high-risk factors for rectal cancer No.253 lymph node metastasis (LNM) and to construct a risk nomogram for the individualized prediction of No.253 LNM.
Methods
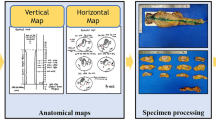
This was a retrospective analysis of 425 patients with rectal cancer who underwent laparoscopic-assisted radical surgery. Independent risk factors for rectal cancer No.253 LNM was identified using multivariate logistic regression analysis, and a risk prediction nomogram was constructed based on the independent risk factors. In addition, the performance of the model was evaluated by discrimination, calibration, and clinical benefit.
Results
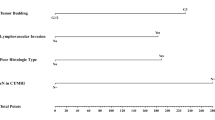
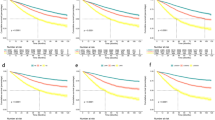
Multivariate logistic regression analysis showed that No.253 lymphadenectasis on CT (OR 10.697, P < 0.001), preoperative T4-stage (OR 4.431, P = 0.001), undifferentiation (OR 3.753, P = 0.004), and preoperative Ca199 level > 27 U/ml (OR 2.628, P = 0.037) were independent risk factors for No.253 LNM. A nomogram was constructed based on the above four factors. The calibration curve of the nomogram was closer to the ideal diagonal, indicating that the nomogram had a better fitting ability. The area under the ROC curve (AUC) was 0.865, which indicated that the nomogram had high discriminative ability. In addition, decision curve analysis (DCA) showed that the model could show better clinical benefit when the threshold probability was between 1% and 50%.
Conclusion
Preoperative No.253 lymphadenectasis on CT, preoperative T4-stage, undifferentiation, and elevated preoperative Ca199 level were found to be independent risk factors for the No.253 LNM. A predictive model based on these risk factors can help surgeons make rational clinical decisions.







Similar content being viewed by others
Data availability
The data sets used or analyzed in this study are available from the corresponding author on reasonable request.
References
Sung H, Ferlay J, Siegel RL et al (2021) Global Cancer statistics 2020: GLOBOCAN estimates of incidence and Mortality Worldwide for 36 cancers in 185 countries. CA Cancer J Clin 71(3):209–249
Mannucci A, Zuppardo RA, Rosati R et al (2019) Colorectal cancer screening from 45 years of age: Thesis, antithesis and synthesis. World J Gastroenterol. ;25(21):2565–2580
Hashiguchi Y, Muro K, Saito Y et al (2020) Japanese Society for Cancer of the Colon and rectum (JSCCR) guidelines 2019 for the treatment of colorectal cancer. Int J Clin Oncol 25(1):1–42
Heald RJ, Husband EM, Ryall RDH (2005) The mesorectum in rectal cancer surgery—the clue to pelvic recurrence? Br J Surg 69(10):613–616
Benson AB, Venook AP, Al-Hawary MM et al (2022) Rectal Cancer, Version 2.2022, NCCN Clinical Practice guidelines in Oncology. J Natl Compr Canc Netw 20(10):1139–1167
Chin CC, Yeh CY, Tang R et al (2008) The oncologic benefit of high ligation of the inferior mesenteric artery in the surgical treatment of rectal or sigmoid colon cancer. Int J Colorectal Dis 23(8):783–788
Kim JC, Lee KH, Yu CS et al (2004) The clinicopathological significance of inferior mesenteric lymph node metastasis in colorectal cancer. Eur J Surg Oncol 30(3):271–279
Crocetti D, Cavallaro G, Tarallo MR et al (2019) Preservation of left colic artery with lymph node dissection of IMA root during laparoscopic surgery for rectosigmoid cancer. Results of a retrospective analysis. Clin Ter 170(2):e124–e128
Kanemitsu Y, Hirai T, Komori K et al (2006) Survival benefit of high ligation of the inferior mesenteric artery in sigmoid colon or rectal cancer surgery. Br J Surg 93(5):609–615
Wang Y, Wang Y, Zou L et al (2022) Does the level of inferior mesenteric artery ligation affect short-term and long-term outcomes of patients with sigmoid colon cancer or rectal cancer? A single-center retrospective study. World J Surg Oncol 20(1):274 Published 2022 Sep 1
Fujii S, Ishibe A, Ota M et al (2019) Short-term and long-term results of a randomized study comparing high tie and low tie inferior mesenteric artery ligation in laparoscopic rectal anterior resection: subanalysis of the HTLT (high tie vs. low tie) study. Surg Endosc 33(4):1100–1110
Matsuda K, Hotta T, Takifuji K et al (2015) Randomized clinical trial of defaecatory function after anterior resection for rectal cancer with high versus low ligation of the inferior mesenteric artery. Br J Surg 102(5):501–508
Rutegård M, Hemmingsson O, Matthiessen P et al (2012) High tie in anterior resection for rectal cancer confers no increased risk of anastomotic leakage. Br J Surg 99(1):127–132
Beppu N, Matsubara N, Noda M et al (2015) A’high tie’confers an increased risk of anastomotic leakage for lower rectal cancer surgery in patients treated with preoperative radiotherapy. Surg Today 45(5):600–605
Rosenberg R, Engel J, Bruns C et al (2010) The prognostic value of lymph node ratio in a population-based collective of colorectal cancer patients. Ann Surg 251(6):1070–1078
Rosenberg R, Friederichs J, Schuster T et al (2008) Prognosis of patients with colorectal cancer is associated with lymph node ratio: a single-center analysis of 3,026 patients over a 25-year time period. Ann Surg 248(6):968–978
Lange MM, Buunen M, van de Velde CJ et al (2008) Level of arterial ligation in rectal cancer surgery: low tie preferred over high tie. A review. Dis Colon Rectum 51(7):1139–1145
Yang Y, Wang G, He J et al (2018) High tie versus low tie of the inferior mesenteric artery in colorectal cancer: a meta-analysis. Int J Surg 52:20–24
Hinoi T, Okajima M, Shimomura M et al (2013) Effect of left colonic artery preservation on anastomotic leakage in laparoscopic anterior resection for middle and low rectal cancer. World J Surg 37(12):2935–2943
Niu JW, Ning W, Wang WY et al (2016) [Clinical effect of preservation of the left colonic artery in laparoscopic anterior resection for rectal cancer]. Zhonghua Yi Xue Za Zhi 96(44):3582–3585
Collins GS, Reitsma JB, Altman DG et al (2015) Transparent reporting of a multivariable prediction model for individual prognosis or diagnosis (TRIPOD): the TRIPOD statement. BMJ 350:g7594 Published 2015 Jan 7
Snell KIE, Levis B, Damen JAA et al (2023) Transparent reporting of multivariable prediction models for individual prognosis or diagnosis: checklist for systematic reviews and meta-analyses (TRIPOD-SRMA). BMJ 381:e073538 Published 2023 May 3
Cai Z, Lin H, Li Z et al (2023) A prediction nomogram for postoperative gastroparesis syndrome in right colon cancer: a retrospective study. Langenbecks Arch Surg 408(1):148 Published 2023 Apr 13
Balachandran VP, Gonen M, Smith JJ et al (2015) Nomograms in oncology: more than meets the eye. Lancet Oncol 16(4):e173–e180
Zhou ZR, Wang WW, Li Y et al (2019) In-depth mining of clinical data: the construction of clinical prediction model with R. Ann Transl Med 7(23):796
Knol J, Keller DS (2020) Total mesorectal excision Technique-Past, Present, and Future. Clin Colon Rectal Surg 33(3):134–143
Wakahara T, Toyokawa A, Ashitani H et al (2015) Comparison of laparoscopic sigmoidectomy with and without preservation of the superior rectal artery: a single-institution retrospective study. Asian J Endosc Surg 8(1):29–33
Wang KX, Cheng ZQ, Liu Z et al (2018) Vascular anatomy of inferior mesenteric artery in laparoscopic radical resection with the preservation of left colic artery for rectal cancer. World J Gastroenterol 24(32):3671–3676
Liakakos T (2011) High ligation of inferior mesenteric artery: a standard procedure for colorectal cancer? Ann Surg Oncol 18(Suppl 3):S240–S243
Hida J, Okuno K (2013) High ligation of the inferior mesenteric artery in rectal cancer surgery. Surg Today 43(1):8–19
Wang LM, Hirano YM, Ishii TM et al (2020) The role of apical lymph node metastasis in right colon cancer. Int J Colorectal Dis 35(10):1887–1894
Derwinger K, Kodeda K, Bexe-Lindskog E et al (2010) Tumour differentiation grade is associated with TNM staging and the risk of node metastasis in colorectal cancer. Acta Oncol 49(1):57–62
Wang L, Hirano Y, Ishii T et al (2020) Left colon as a novel high-risk factor for postoperative recurrence of stage II colon cancer. World J Surg Oncol 18(1):54 Published 2020 Mar 11
Huh JW, Kim YJ, Kim HR (2012) Distribution of lymph node metastases is an independent predictor of survival for sigmoid colon and rectal cancer. Ann Surg 255(1):70–78
Shin JK, Kim HC, Lee WY et al (2019) High preoperative serum CA 19 – 9 levels can predict poor oncologic outcomes in colorectal cancer patients on propensity score analysis. Ann Surg Treat Res 96(3):107–115
Polat E, Duman U, Duman M et al (2014) Diagnostic value of preoperative serum carcinoembryonic antigen and carbohydrate antigen 19 – 9 in colorectal cancer. Curr Oncol 21(1):e1–e7
Dighe S, Purkayastha S, Swift I et al (2010) Diagnostic precision of CT in local staging of colon cancers: a meta-analysis. Clin Radiol 65(9):708–719
Kijima S, Sasaki T, Nagata K et al (2014) Preoperative evaluation of colorectal cancer using CT colonography, MRI, and PET/CT. World J Gastroenterol 20(45):16964–16975
Anderson EM, Betts M, Slater A (2011) The value of true axial imaging for CT staging of colonic cancer. Eur Radiol 21(6):1286–1292
Filippone A, Ambrosini R, Fuschi M et al (2004) Preoperative T and N staging of colorectal cancer: accuracy of contrast-enhanced multi-detector row CT colonography–initial experience. Radiology 231(1):83–90
Duman M, Tas S, Mecit EA et al (2012) Preoperative local staging of colorectal cancer patients with MDCT. Hepatogastroenterology 59(116):1108–1112
Vag T, Slotta-Huspenina J, Rosenberg R et al (2014 Nov-Dec) Computerized analysis of enhancement kinetics for preoperative lymph node staging in rectal cancer using dynamic contrast-enhanced magnetic resonance imaging. Clin Imaging 38(6):845–849
Schrembs P, Martin B, Anthuber M et al (2018) The prognostic significance of lymph node size in node-positive colon cancer. PLoS ONE 13(8):e0201072 Published 2018 Aug 10
Long C, Feng M, Wang S et al (2023) A clinicopathological feature-based Nomogram for Predicting the Likelihood of D3 Lymph Node Metastasis in right-sided Colon cancer patients. Dis Colon Rectum 66(1):75–86
Leufkens AM, van den Bosch MA, van Leeuwen MS et al (2011) Diagnostic accuracy of computed tomography for colon cancer staging: a systematic review. Scand J Gastroenterol 46(7–8):887–894
Liu D, Sun LM, Liang JH et al (2022) Diagnostic accuracy of ≥ 16-slice spiral computed tomography for local staging of colon cancer: a systematic review and meta-analysis. World J Clin Cases 10(19):6483–6495
Nerad E, Lambregts DM, Kersten EL et al (2017) MRI for local staging of Colon cancer: can MRI become the optimal staging modality for patients with Colon cancer? Dis Colon Rectum 60(4):385–392
Acknowledgements
Thank American Journal Experts (AJE) for proofreading the English grammar and spelling of our paper.
Funding
Not applicable
Author information
Authors and Affiliations
Contributions
Conception and design: WXC, ZMC, YCX. Performed the research and acquired the data: WXC, ZMC, JFZ, ZNX, ZXL, ZXG, JPL, ZPG, HYW, YCX. Analyzed the data: WXC, ZMC. Manuscript writing: WXC, ZMC, JFZ, YCX. Final approval of manuscript: All authors.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Weixiang Chen, Zhiming Cai, and Jinfeng Zhou have contributed equally to this work, and should be regarded as first co-authors.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chen, W., Cai, Z., Zhou, J. et al. Construction of a nomogram based on clinicopathologic features to predict the likelihood of No. 253 lymph node metastasis in rectal cancer patients. Langenbecks Arch Surg 409, 161 (2024). https://doi.org/10.1007/s00423-024-03353-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00423-024-03353-5