Abstract
Background
Laparoscopic cholecystectomy (LC) is the standard of care for acute calculous cholecystitis; however, in patients at high risk for surgery, particularly in the elderly, insertion of a percutaneous catheter drainage (PCD) at gallbladder is recommended. Current evidence suggests that PCD may have less favorable outcomes than LC, but also that LC-associated complications increase in direct relation to patient age. There is no recommendation supported by robust evidence to decide between one or the other procedure in super elderly patients.
Methods
A retrospective observational cohort study was designed to analyze the surgical outcomes of super elderly patients with cholecystitis who underwent LC versus PCD for treatment. The surgical outcomes of a subgroup of high-risk patients were also analyzed.
Results
A total of 96 patients who met the inclusion criteria between 2014 and 2021 were included. The median age of patients were 92 years (IQR: 4.00) with a female predominance (58.33%). The overall morbidity rate in the series was 36.45% and mortality rate was 7.29%. There was no statistically significant difference when compared to the associated morbidity and mortality among patients who underwent LC versus those who underwent PCD, neither in the analysis of the complete series or in the subgroup of high-risk patients.
Conclusions
The morbidity and mortality associated with the two most frequently recommended therapeutic options for operating super elderly patients with acute cholecystitis are high. We found no evidence of superiority in outcomes for either of the two procedures in this age group.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The prevalence of gallstones is estimated to be 10-15% in the general population, its most frequent clinical manifestation being acute cholecystitis. Laparoscopic cholecystectomy (LC) is the current standard of care for acute calculous cholecystitis [1]. However, major complications of LC and postoperative morbidity and mortality rates increase with age, and it is estimated that perioperative mortality risk in those over 80 years of age can be increased tenfold [2]. Additionally, due to their low functional reserve nonagenarian patients are often not considered candidates for general anesthesia, which is necessary for the performance of LC [3]. Therefore, it is essential to explore therapeutic alternatives such as the insertion of a percutaneous catheter drainage (PCD) in the gallbladder for this particular population [1].
There are few studies that assess results of LC in super elderly patients; an age group who, due to recent research, is in a state of constant exponential growth [4, 5]. Moreover, some studies have evaluated PCD management in high-risk patients, finding a higher rate of complications. A systematic review of present literature shows that 30-day mortality after the procedure can be as high as 15.4% [6, 7]. Therefore, it is relevant to compare the results of both management options (LC vs PCD) in patients such as the super elderly, a special population with a high perioperative risk due to their fragility and multiple comorbidities [3]. Such a study has not been described in actual literature up to this date.
The aim of this study is to compare surgical outcomes, complications, and mortality rates in super elderly (> 90 years of age) patients who underwent LC versus PCD for acute calculous cholecystitis.
Patients and methods
Study design
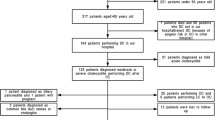
A retrospective observational cohort study was designed. Between January 2014 and December 2021, 13.192 cholecystectomies were performed in our institution [8]. Among them, 65 laparoscopic cholecystectomies were carried out in patients over 90 years of age with the presence of cholecystitis. During the same period, 286 PCDs were performed, out of which 31 were performed in patients over 90 years of age coursing with cholecystitis. Variables were collected in an anonymous database. This study was reviewed and approved by the ethics committee (number DVO005 2066-CV1595). We followed STROBE guidelines in order to report this study [9].
Patients
Patients over 90 years of age with a diagnosis of cholecystitis were included. Patients scheduled for open cholecystectomy with a diagnosis of gallbladder cancer or cholecystectomy associated to another surgical procedure (gastrectomy or pancreaticoduodenectomy, among others), patients without postoperative follow-up (postoperative follow-up appointment), and patients whose records did not have variables of interest were excluded.
In all cases LC indication was a cholecystitis diagnosis confirmed by at least one imaging study, these were classified by severity and were treated accordingly following Tokyo guidelines [10, 11]. The American Society for Gastrointestinal Endoscopy protocol guideline was followed to establish risk of choledocholithiasis; LCs or PCDs was performed without additional studies in low-risk cases; LC or PCD was performed after discarding choledocholithiasis with magnetic resonance cholangiography in intermediate-risk cases and after endoscopic retrograde cholangiopancreatography (ERCP) in high-risk cases [12]. The decision to perform LC or PCD was taken depending on surgeon criteria, taking into account pre-anesthetic assessment and the risk/benefit ratio for the procedure.
All patients had an outpatient control appointment (20 +/- 5 days after hospital discharge) where clinical evolution and surgical wounds were evaluated. In cases with PCD, correct catheter functioning was checked.
We analyzed the following data: patient demographic characteristics, body mass index, ASA Physical Status Classification, presence of comorbidities, preoperative laboratory tests, bile duct diameter in preoperative imaging, classification of cholecystitis severity, need for preoperative ERCP, time from admission to completion of surgical procedure, intraoperative findings (Nassar Score), conversion rate, type of cholecystectomy (total or subtotal), drain usage, PCD removal/dysfunction, complications associated with the procedure and hospitalization, recurrence of biliary disease, hospital stay, reintervention requirement, and mortality.
Surgical procedure
Laparoscopic cholecystectomy was performed with the standard 4-port technique in the American position. Dissection of the hepatocystic triangle was performed when critical safety window was reached, dissecting above the R4U line in all cases. After reaching the critical view of safety, ligation of the cystic duct and artery and dissection of the gallbladder was performed. In cases where critical view of safety was not achieved, alternative strategies such as fundus first, subtotal cholecystectomy or conversion to open procedure were used according to surgeon preference. Drain placement in surgical site was also performed according to surgeon discretion.
Percutaneous drainage by catheter was performed under ultrasound guidance with a multi frequency convex transducer. The gallbladder was punctured with a Chiba 22 G needle; a micro guide was advanced and a triaxial system was placed over it. Consequently, the micro guide was removed, the support guide was advanced, and the 10 Fr drainage catheter was pushed forward and into the gallbladder. In all cases, the catheter was fixed with a Revolution™ fixation device and plugged into a collection bag for proper drainage.
Statistical analysis
A description was made with demographic, clinical, paraclinical and surgical variables and outcomes. Categorical variables were described as proportions and continuous variables as medians with their respective interquartile range (IQR). A bivariate analysis was performed with the Chi-squared test for categorical variables and with the Mann-Whitney test for continuous variables among patients who underwent laparoscopic cholecystectomy and those who underwent cholecystostomy. In addition, this same analysis was performed separately on a subgroup of patients defined as high risk (ASA ≥3) in order to compare outcomes. A multivariate analysis was performed to identify the independent factors for major complications (Clavien-Dindo ≥3), the variables were included with p < 0.1 in the bivariate analysis and those considered as clinically relevant. This entire analysis was performed in SPSS® 27, considering p<0.05 as statistically significant.
Results
This study included 96 patients. LC was performed in 65 (67.7%) cases. The selection process is shown in the following flowchart (Fig. 1).
Median patient age was 92 years (IQR: 4.00) and were predominantly female (58.33%). Table 1 shows demographic, clinical and paraclinical characteristics according to the procedure performed.
Intraoperative findings were measured using the Nassar score (where a higher score is directly proportional to a more difficult laparoscopic cholecystectomy). We found a higher rate of difficult cholecystectomies (grades 3, 4 and 5) than easy cholecystectomies (grades 1 and 2) [13, 14].
The rate of complications in the complete series was 36.45% and mortality was 7.29%. There were no statistically significant differences when comparing morbidity and mortality among patients who underwent LC versus those who underwent PCD (Table 2).
Five patients who underwent LC died secondary to bile duct injury, postoperative bleeding, acute myocardial infarction, pulmonary embolism and septic shock due to cholecystitis. The two patients who died in the PCD group were from septic shock due to cholecystitis.
The sex, IMC, ASA Physical Status Classification, chronic obstructive pulmonary disease, cardiovascular disease, anticoagulant agents, antiplatelet agents, bile duct diameter and laparoscopic cholecystectomy were identified as potential risk factors for the development of major complications therefore, were included in the multivariate analysis. we did not find statistically significant differences in the outcomes with any of the variables (Table 3).
Analysis of high-risk patients’ subgroup
Comparison of demographic, clinical and surgical variables in the subgroup of high-risk patients (defined as ASA ≥3) showed the same differences within the general group, except for gender (Table 4).
There were also no statistically significant differences between outcomes for both treatment groups in this subgroup, with a complication rate of 43.18%, a major complication rate of 22.73%, and a mortality rate of 4.55% for patients who underwent LC (Table 5).
Discussion
Our study did not show statistically significant differences when comparing outcomes in LC and PCD for the management of cholecystitis in a series of 96 super elderly patients. Neither were there any statistically significant differences when analyzing a subgroup of high-risk patients within the series. We consider the results of this paper as a contribution to the available literature regarding treatment alternatives for patients over 90 years of age, regarding insufficient evidence in this group of patients when choosing adequate treatment between both procedures (LC or PCD).
LC is considered the standard of care for benign biliary disease due to its efficacy and low complication rate, however we should regard special considerations for this procedure in elderly patients because of the high complication and mortality rate in this age group [2]. Furthermore, the rate of difficult cholecystectomies in this age group according to Nassar’s Score were higher than what is usually reported [8, 14].
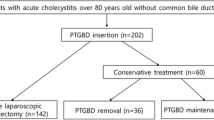
For high-risk patients, PCD has been proposed as an alternative procedure since it can be performed at the patient’s bedside and under local anesthesia, with the aim of reducing risks of general anesthesia and those inherent to the surgical procedure [15, 16]. However, studies have shown a higher rate of complications in PCD for the management of acute cholecystitis compared to LC [17], even in elderly and high-risk patients, therefore, some guidelines recommend LC as the standard of care [2]. The current evidence-based indication for PCD is in patients not eligible for surgical procedure in order to resolve septic status [1].
When evaluating the subgroup of high-risk patients (ASA≥3) we found surgical outcomes similar to those observed in the general group, with no statistically significant differences between the two procedures. It should be noted that, when assessing the high-risk subgroup, only 3 patients (11.11%) of those who underwent PCD were excluded from the analysis; on the other hand, 21 patients (30.30%) of those who underwent LC were; this suggests that PCD is used in patients who are considered unable to tolerate surgery, which is logical and consistent with actual evidence.
We also highlight our finding of a statistically significant difference in patients with a greater presence of cardiovascular and pulmonary comorbidities who underwent PCD. We believe that this difference showcases both surgeon and anesthesiologist preference for PCD in these patients during clinical practice, taking into consideration the physiological repercussions of pneumoperitoneum during laparoscopic procedures.
Regarding the limitations of this paper, we consider the retrospective nature of the cohort, small sample size and limited follow-up. The deficient information on the medium- and long-term follow-up of patients in the group who underwent PCD is particularly relevant, since the monitoring of complications such as catheter dysfunction/removal or symptom recurrence that may deserve additional interventions in the medium and long term is essential for a complete and accurate description of results in this group.
The super elderly group constitutes a special population, which is constantly increasing (1,5)(1,5)(1,5)(1,3), and deserves specialized studies due to their characteristics [18, 19]. Benign biliary pathology is not the only exception and complications associated to cholelithiasis and age should be taken into account [20]. To this date, LC continues to be the standard of care for benign biliary pathology [20]; however, prospective studies with longer follow-up controls are needed in this group of patients, considering LC may not be so well tolerated, and to evaluate factors such as quality of life [21] with the aim of defining the best treatment alternative.
Conclusions
In this study, we found no significant differences between major complications and mortality in super elderly patients with acute cholecystitis treated by LC or PCD. Although LC is still the standard of care in benign biliary pathology, morbidity and mortality rates associated with this procedure increase exponentially with age, therefore, it is necessary to evaluate each case individually to select the best treatment alternative available in order to avoid complications and improve quality of life in super elderly patients.
Data Availability
Data are available on request through institutional review board of Hospital Universitario Mayor - Méderi. You can contact to request the data to jose.daza@mederi.com.co.
References
Pisano M, Allievi N, Gurusamy K, Borzellino G, Cimbanassi S, Boerna D et al (2020) 2020 World Society of Emergency Surgery updated guidelines for the diagnosis and treatment of acute calculus cholecystitis. World J Emerg Surg 15(1):1–27
Kamarajah SK, Karri S, Bundred JR, Evans RPT, Lin A, Kew T et al (2020) Perioperative outcomes after laparoscopic cholecystectomy in elderly patients: a systematic review and meta-analysis. Surg Endosc 34(11):4727–4740. https://doi.org/10.1007/s00464-020-07805-z
Wahlen BM, De GA (2021) Anesthetic Concerns in Advanced Age Undergoing Emergency Surgery. In: Latifi R, Catena F, Coccolini F (eds) Emergency General Surgery in Geriatrics [Internet]. First. Springer, pp 97–127 Available from: https://link.springer.com/10.1007/978-3-030-62215-2
DANE. Serie nacional de población por área, sexo y edad para el periodo 2018 – 2070 [Internet]. 2020. Available from: https://www.dane.gov.co/index.php/estadisticas-por-tema/demografia-y-poblacion/proyecciones-de-poblacion. Accessed 25 Jan 2022
Dubecz A, Langer M, Stadlhuber RJ, Schweigert M, Solymosi N, Feith M et al (2012) Cholecystectomy in the Very Elderly-Is 90 the New 70? J Gastrointest Surg 16(2):282–285
Winbladh A, Gullstrand P, Svanvik J, Sandström P (2009) Systematic review of cholecystostomy as a treatment option in acute cholecystitis. Hpb. 11(3):183–193
Loozen CS, Van Santvoort HC, Van Duijvendijk P, Besselink MG, Gouma DJ, Nieuwenhuijzen GA et al (2018) Laparoscopic cholecystectomy versus percutaneous catheter drainage for acute cholecystitis in high risk patients (CHOCOLATE): Multicentre randomised clinical trial. BMJ. 363
Ramírez-Giraldo C, Alvarado-Valenzuela K, Restrepo-Isaza A, Navarro-Alean J (2022) Predicting the difficult laparoscopic cholecystectomy based on a preoperative scale. Updates Surg 74(3):969–977. https://doi.org/10.1007/s13304-021-01216-y
von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP (2008) The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol 61(4):344–349
Yokoe M, Hata J, Takada T, Strasberg SM, Asbun HJ, Wakabayashi G et al (2018) Tokyo Guidelines 2018: diagnostic criteria and severity grading of acute cholecystitis (with videos). J Hepatobiliary Pancreat Sci 25(1):41–54
Okamoto K, Suzuki K, Takada T, Strasberg SM, Asbun HJ, Endo I et al (2018) Tokyo Guidelines 2018: flowchart for the management of acute cholecystitis. J Hepatobiliary Pancreat Sci 25(1):55–72
Buxbaum JL, Abbas Fehmi SM, Sultan S, Fishman DS, Qumseya BJ, Cortessis VK et al (2019) ASGE guideline on the role of endoscopy in the evaluation and management of choledocholithiasis. Gastrointest Endosc 89(6):1075–1105.e15. https://doi.org/10.1016/j.gie.2018.10.001
Griffiths EA, Hodson J, Vohra RS, Marriott P, Katbeh T, Zino S et al (2019) Utilisation of an operative difficulty grading scale for laparoscopic cholecystectomy. Surg Endosc 33(1):1–12. https://doi.org/10.1007/s00464-018-6281-2
Nassar AHM, Hodson J, Ng HJ, Vohra RS, Katbeh T, Zino S et al (2019) Predicting the difficult laparoscopic cholecystectomy: development and validation of a pre-operative risk score using an objective operative difficulty grading system. Surg Endosc 34:4549–4561
Garcés-Albir M, Martín-Gorgojo V, Perdomo R, Molina-Rodríguez JL, Muñoz-Forner E, Dorcaratto D et al (2020) Acute cholecystitis in elderly and high-risk surgical patients: is percutaneous cholecystostomy preferable to emergency cholecystectomy? J Gastrointest Surg 24(11):2579–2586
Schlottmann F, Gaber C, Strassle PD, Patti MG, Charles AG (2018) Comparative Analysis of Cholecystectomy vs. Cholecystostomy for the Management of Acute Cholecystitis in Elderly Patients. Gastroenterology. 154(6):S-1311
Markopoulos G, Mulita F, Kehagias D, Tsochatzis S, Lampropoulos C, Kehagias I (2021) Outcomes of percutaneous cholecystostomy in elderly patients: A systematic review and meta-analysis. Prz Gastroenterol 16(3):188–195
Ogawa Y, Ikeda K, Watanabe C, Kamei Y, Goto W, Shiraishi C et al (2019) Super-elderly patient-specific perioperative complications in breast cancer surgery. Surg Today 49(10):843–849. https://doi.org/10.1007/s00595-019-01812-x
Hashida H, Ryosuke M, Kentaro I, Kanbe H, Sumi T, Kawarabayashi T et al (2021) Laparoscopic Surgery for Colorectal Cancer in Super-Elderly Patients: A Single-Center Analysis. Surg Laparosc Endosc Percutan Tech 31(3):337–341
Sugrue M, Huan H, Skelly B, Watson A (2021) Emergency Cholecystectomy in the Elderly. In: Latifi R, Catena F, Coccolini F (eds) Emergency General Surgery in Geriatrics [Internet]. First. Springer, pp 407–418 Available from: https://link.springer.com/10.1007/978-3-030-62215-2
Miura Y, Nishio K, Kitamura Y, Goto T, Yano M, Matsui S (2022) Surgical risk assessment for super-elderly patients. Geriatr Gerontol Int 22(4):271–277
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
Camilo Ramírez-Giraldo: Study design, acquisition of data, analysis and interpretation of data, drafting of manuscript, critical revision of manuscript. Andrés Isaza-Restrepo: Analysis and interpretation of data, drafting of manuscript, critical revision of manuscript. Enid Ximena Rico-Rivera: Study conception and design, acquisition of data, critical revision of manuscript.Juan Carlos Vallejo-Soto: Study conception and design, acquisition of data, critical revision of manuscript. Isabella Van-Londoño: Drafting of manuscript, critical revision of manuscript.
Corresponding author
Ethics declarations
Conflicts of interest
All authors declare no conflicts of interest.
Ethical standards
Ethical compliance with the Helsinki Declaration, current legislation on research Res. 008430-1993 and Res. 2378-2008 (Colombia) and the International Committee of Medical Journal Editors (ICMJE) were ensured under our Ethics and Research Institutional Committee (IRB) approval. Informed consent was filled out as required for the execution of this study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ramírez-Giraldo, C., Isaza-Restrepo, A., Rico-Rivera, E.X. et al. Laparoscopic cholecystectomy versus percutaneous catheter drainage for acute calculous cholecystitis in patients over 90 years of age. Langenbecks Arch Surg 408, 194 (2023). https://doi.org/10.1007/s00423-023-02903-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00423-023-02903-7