Abstract
Purpose
Abdominal Veress needle insertion is commonly performed to generate a pneumoperitoneum during laparoscopy. Various safety tests are conducted to confirm accurate needle tip positioning into the abdominal cavity. However, these occasionally yield unclear results and do not help directly visualize the peritoneum puncture. We validated a negative pressure–based technique that helps instantly visualize the moment of the Veress needle entry into the abdominal cavity.
Methods
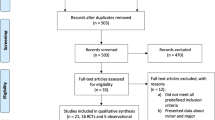
This study included 761 patients who underwent laparoscopic hernioplasty between 2003 and 2021 that entailed pneumoperitoneum creation using a Veress needle. They were divided into conventional technique (CON) and negative pressure visualization technique (NPV) groups. The patients were propensity score–matched (1:1) to minimize selection bias. To determine whether the technique gave a clear result to the surgeon and precisely informed the moment of entry, failed entry and emphysematous complications were compared between the groups.
Results
The propensity score–matching yielded 105 pairs in the matched CON and NPV groups. Failed entry did not occur in the NPV group, whereas it occurred in 8 patients (7.6%) in the CON group (p = 0.004). No patient experienced extraperitoneal emphysema in the matched NPV group, whereas 7 patients (6.7%) in the CON group did (p = 0.007). The groups did not differ in the incidence of omental or mesenteric emphysema.
Conclusion
The NPV eliminated the incidence of failed entry and decreased the incidence of extraperitoneal emphysema, indicating that it could simply and adequately inform the moment of needle entry into the abdominal cavity.




Similar content being viewed by others
Availability of data and materials
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
References
Merlin TL, Hiller JE, Maddern GJ, Jamieson GG, Brown AR, Kolbe A (2003) Systematic review of the safety and effectiveness of methods used to establish pneumoperitoneum in laparoscopic surgery. Br J Surg 90:668–679
Molloy D, Kaloo PD, Cooper M, Nguyen TV (2002) Laparoscopic entry: a literature review and analysis of techniques and complications of primary port entry. Aust N Z J Obstet Gynaecol 42:246–254
Jansen FW, Kolkman W, Bakkum EA, de Kroon CD, Trimbos-Kemper TC, Trimbos JB (2004) Complications of laparoscopy: an inquiry about closed- versus open-entry technique. Am J Obstet Gynecol 190:634–638
Catarci M, Carlini M, Gentileschi P, Santoro E (2001) Major and minor injuries during the creation of pneumoperitoneum. A multicenter study on 12,919 cases. Surg Endosc 15:566–569
Teoh B, Sen R, Abbott J (2005) An evaluation of four tests used to ascertain Veres needle placement at closed laparoscopy. J Minim Invasive Gynecol 12:153–158
Azevedo OC, Azevedo JL, Sorbello AA, Miguel GP, Wilson Junior JL, Godoy AC (2006) Evaluation of tests performed to confirm the position of the Veress needle for creation of pneumoperitoneum in selected patients: a prospective clinical trial. Acta Cirurgica Brasileira 21:385–391
Thepsuwana J, Huang KG, Wilamarta M, Adlan A, Manvelyan V, Lee C (2013) Principles of safe abdominal entry in laparoscopic gynecologic surgery. J Minim Invasive Gynecol 2:105
Krishnakumar S, Tambe P (2009) Entry complications in laparoscopic surgery. Journal of Gynecological Endoscopy and Surgery 1:4–11
Burke C, Nathan E, Karthigasu K, Garry R, Hart R (2009) Laparoscopic entry—the experience of a range of gynaecological surgeons. Gynecol Surg 6:125–133
Pratap A, Oleynikov D, Kothari V (2018) Real time ultrasound guided insertion of Veress needle in obese patients. Ann R Coll Surg Engl 100:158–159
Silay MS, Tepeler A, Sancaktutar AA, Kilincaslan H, Altay B, Erdem MR, Hatipoglu NK, Akcay M, Akman T, Armagan A (2013) The all-seeing needle instead of the Veress needle in pediatric urologic laparoscopy. J Endourol 27:1376–1380
Schaufler A, Sühn T, Esmaeili N, Boese A, Wex C, Croner R, Friebe M, Illanes A (2019) Automatic differentiation between Veress needle events in laparoscopic access using proximally attached audio signal characterization. Current Directions in Biomedical Engineering 5:369–371
Postema RR, Cefai D, van Straten B, Miedema R, Hardjo LL, Dankelman J, Nickel F, Horeman-Franse T (2021) A novel Veress needle mechanism that reduces overshooting after puncturing the abdominal wall. Surg Endosc 35:5857–5866
Coccolini F, Ansaloni L, Manfredi R, Campanati L, Poiasina E, Bertoli P, Capponi MG, Sartelli M, Di Saverio S, Cucchi M, Lazzareschi D, Pisano M, Catena F (2013) Peritoneal adhesion index (PAI): proposal of a score for the “ignored iceberg” of medicine and surgery. World Journal of Emergency Surgery: WJES 8:6
Wada H, Kimura T, Kawabe A, Sato M, Miyaki Y, Tochikubo J, Inamori K, Shiiya N (2012) Laparoscopic transabdominal preperitoneal inguinal hernia repair using needlescopic instruments: a 15-year, single-center experience in 317 patients. Surg Endosc 26:1898–1902
Mukaka MM (2012) Statistics corner: a guide to appropriate use of correlation coefficient in medical research. Malawi Medical Journal: The Journal of Medical Association of Malawi 24:69–71
Austin PC (2011) Optimal caliper widths for propensity-score matching when estimating differences in means and differences in proportions in observational studies. Pharm Stat 10:150–161
Austin PC (2009) Balance diagnostics for comparing the distribution of baseline covariates between treatment groups in propensity-score matched samples. Stat Med 28:3083–3107
Sekhon JS (2011) Multivariate and propensity score matching software with automated balance optimization: the matching package for R. J Stat Softw 42:1–52
Kanda Y (2013) Investigation of the freely available easy-to-use software “EZR” for medical statistics. Bone Marrow Transplant 48:452–458
Ahmad G, Baker J, Finnerty J, Phillips K, Watson A (2019) Laparoscopic entry techniques. The Cochrane Database of Systematic Reviews 1:CD006583
Angioli R, Terranova C, De Cicco NC, Cafa EV, Damiani P, Portuesi R, Muzii L, Plotti F, Zullo MA, Panici PB (2013) A comparison of three different entry techniques in gynecological laparoscopic surgery: a randomized prospective trial. Eur J Obstet Gynecol Reprod Biol 171:339–342
Agresta F, De Simone P, Ciardo LF, Bedin N (2004) Direct trocar insertion vs Veress needle in nonobese patients undergoing laparoscopic procedures: a randomized prospective single-center study. Surg Endosc 18:1778–1781
Jansen FW, Kapiteyn K, Trimbos-Kemper T, Hermans J, Trimbos JB (1997) Complications of laparoscopy: a prospective multicentre observational study. Br J Obstet Gynaecol 104:595–600
Vilos GA, Vilos AG (2003) Safe laparoscopic entry guided by Veress needle CO2 insufflation pressure. J Am Assoc Gynecol Laparosc 10:415–420
Vilos GA, Ternamian A, Dempster J, Laberge PY (2007) Laparoscopic entry: a review of techniques, technologies, and complications. Journal of Obstetrics and Gynaecology Canada: JOGC = Journal d’Obstetrique et Gynecologie du Canada: JOGC 29:433–447
Briel JW, Plaisier PW, Meijer WS, Lange JF (2000) Is it necessary to lift the abdominal wall when preparing a pneumoperitoneum? A randomized study. Surg Endosc 14:862–864
Roy GM, Bazzurini L, Solima E, Luciano AA (2001) Safe technique for laparoscopic entry into the abdominal cavity. J Am Assoc Gynecol Laparosc 8:519–528
Sakamoto A, Kikuchi I, Shimanuki H, Tejima K, Saito J, Sakai K, Kumakiri J, Kitade M, Takeda S (2017) Initial closed trocar entry for laparoscopic surgery: technique, umbilical cosmesis, and patient satisfaction. Gynecology and Minimally Invasive Therapy 6:167–172
Sanchez NC, Tenofsky PL, Dort JM, Shen LY, Helmer SD, Smith RS (2001) What is normal intra-abdominal pressure? Am Surg 67:243–248
Shamiyeh A, Glaser K, Kratochwill H, Hormandinger K, Fellner F, Wayand WU, Zehetner J (2009) Lifting of the umbilicus for the installation of pneumoperitoneum with the Veress needle increases the distance to the retroperitoneal and intraperitoneal structures. Surg Endosc 23:313–317
Cakir T, Tuney D, Esmaeilzadem S, Aktan AO (2006) Safe Veress needle insertion. J Hepatobiliary Pancreat Surg 13:225–227
Neudecker J, Sauerland S, Neugebauer E, Bergamaschi R, Bonjer HJ, Cuschieri A, Fuchs KH, Jacobi C, Jansen FW, Koivusalo AM, Lacy A, McMahon MJ, Millat B, Schwenk W (2002) The European Association for Endoscopic Surgery clinical practice guideline on the pneumoperitoneum for laparoscopic surgery. Surg Endosc 16:1121–1143
Author information
Authors and Affiliations
Contributions
Takanobu Onoda developed the method, reviewed the videos, collected and analyzed the data, and drafted the manuscript. Masanori Sato designed the study, reviewed the videos, collected the data, and revised the manuscript with conceptual and editorial input. Kakeru Torii reviewed the videos and collected the data. Koji Inamori collected the data, and Eisaku Okada assisted with and reviewed the statistical analyses. Masashi Nozawa, Norihiko Shiiya, and Hidetoshi Wada revised the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Hamamatsu University School of Medicine Independent Ethics Committee (Permission number: 20–294). The requirement for patient consent was waived by the committee. Patient permission was requested on the institute’s website, and opt-out consent was obtained from the patients.
Consent for publication
The authors affirm that the participant provided informed consent for publication of the images in Fig. 2 and the supplemental movie.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary file2 (MP4 16153 kb)
Rights and permissions
About this article
Cite this article
Onoda, T., Sato, M., Torii, K. et al. A negative pressure–based visualization technique for abdominal Veress needle insertion. Langenbecks Arch Surg 407, 2105–2113 (2022). https://doi.org/10.1007/s00423-022-02504-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-022-02504-w