Abstract
Purpose
Laser speckle flowgraphy (LSFG) is a noninvasive method for quantitative evaluation of blood flow using the mean blur rate (MBR) as the blood flow index. We investigated whether LSFG can intraoperatively detect the demarcation line after vessel dissection and reduce the incidence of anastomotic leakage (AL).
Methods
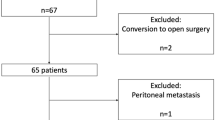
This study included 36 patients who underwent left-sided colorectal surgery. First, we compared the demarcation line (determined by LSFG) with the transection line (TL) at which the marginal vessels were divided. We then measured the MBR on both sides of the TL to determine where the MBR changed significantly. We investigated the presence or absence of significant differences between the MBR on the proximal side and that on the distal side of the TL. Finally, we retrospectively compared the patient characteristics and AL rates in the LSFG group (n = 36) and control group (n = 87).
Results
In total, 58.3% (21/36) of the demarcation lines determined by LSFG matched the TL. The median distance between the demarcation line determined by LSFG and the TL was 0.0 mm (0.0–12.1 mm). The MBR sharply decreased at the TL in 80.6% (29/36) of cases. The median MBR was significantly lower on the distal than proximal side. The AL rate was not significantly lower in the LSFG group than in the control group.
Conclusion
LSFG accurately detected the demarcation line during surgery. However, LSFG did not reduce the incidence of AL.






Similar content being viewed by others
References
Shogan BD, Carlisle EM, Alverdy JC, Umanskiy K (2013) Do we really know why colorectal anastomoses leak? J Gastrointest Surg 17:1698–1707. https://doi.org/10.1007/s11605-013-2227-0
Attard JA, Raval MJ, Martin GR, Kolb J, Afrouzian M, Buie WD, Sigalet DL (2005) The effects of systemic hypoxia on colon anastomotic healing: an animal model. Dis Colon Rectum 48:1460–1470. https://doi.org/10.1007/s10350-005-0047-3
James DR, Ris F, Yeung TM, Kraus R, Buchs NC, Mortensen NJ, Hompes RJ (2015) Fluorescence angiography in laparoscopic low rectal and anorectal anastomoses with pinpoint perfusion imaging--a critical appraisal with specific focus on leak risk reduction. Color Dis 17(Suppl 3):16–21. https://doi.org/10.1111/codi.13033
Boyle NH, Manifold D, Jordan MH, Mason RC (2000) Intraoperative assessment of colonic perfusion using scanning laser Doppler flowmetry during colonic resection. J Am Coll Surg 191:504–510. https://doi.org/10.1016/s1072-7515(00)00709-2
Hirano Y, Omura K, Tatsuzawa Y, Shimizu J, Kawaura Y, Watanabe G (2006) Tissue oxygen saturation during colorectal surgery measured by near-infrared spectroscopy: pilot study to predict anastomotic complications. World J Surg 30:457–461. https://doi.org/10.1007/s00268-005-0271-y
Ambrosetti P, Robert J, Mathey P, Rohner A (1994) Left-sided colon and colorectal anastomoses: Doppler ultrasound as an aid to assess bowel vascularization. A prospective evaluation of 200 consecutive elective cases. Int J Color Dis 9:211–214. https://doi.org/10.1007/bf00292253
Karliczek A, Benaron DA, Baas PC, Zeebregts CJ, Wiggers T, Van Dam GM (2010) Intraoperative assessment of microperfusion with visible light spectroscopy for prediction of anastomotic leakage in colorectal anastomoses. Color Dis 12:1018–1025. https://doi.org/10.1111/j.1463-1318.2009.01944.x
Darwich I, Rustanto D, Friedberg R, Willeke F (2019) Spectrophotometric assessment of bowel perfusion during low anterior resection: a prospective study. Updates Surg 71(4):677–686. https://doi.org/10.1007/s13304-019-00682-9
Jafari MD, Wexner SD, Martz JE, McLemore EC, Margolin DA, Sherwinter DA, Lee SW, Senagore AJ, Phelan MJ, Stamos MJ (2015) Perfusion assessment in laparoscopic left-sided/anterior resection (PILLAR II): a multi-institutional study. J Am Coll Surg 220:82–92. https://doi.org/10.1016/j.jamcollsurg.2014.09.015
Kudszus S, Roesel C, Schachtrupp A, Höer JJ (2010) Intraoperative laser fluorescence angiography in colorectal surgery: a noninvasive analysis to reduce the rate of anastomotic leakage. Langenbeck’s Arch Surg 395:1025–1030. https://doi.org/10.1007/s00423-010-0699-x
De Nardi P, Elmore U, Maggi G, Maggiore R, Boni L, Cassinotti E, Fumagalli U, Gardani M, De Pascale S, Parise P, Vignali A, Rosati R (2020) Intraoperative angiography with indocyanine green to assess anastomosis perfusion in patients undergoing laparoscopic colorectal resection: results of a multicenter randomized controlled trial. Surg Endosc 34(1):53–60. https://doi.org/10.1007/s00464-019-06730-0
Hayami S, Matsuda K, Iwamoto H, Ueno M, Kawai M, Hirono S, Okada K, Miyazawa M, Tamura K, Mitani Y, Kitahata Y, Mizumoto Y, Yamaue H (2019) Visualization and quantification of anastomotic perfusion in colorectal surgery using near-infrared fluorescence. Tech Coloproctol 23:973–980. https://doi.org/10.1007/s10151-019-02089-5
Bjerregaard J, Pandia MP, Jaffe RA (2013) Occurrence of severe hypotension after indocyanine green injection during the intraoperative period. A A Case Rep 1:26–30. https://doi.org/10.1097/ACC.0b013e3182933c12
Fujii H, Nohira K, Yamamoto Y, Ikawa H, Ohura T (1987) Evaluation of blood flow by laser speckle image sensing. Part 1. Appl Opt 26:5321–5325. https://doi.org/10.1364/AO.26.005321
Sugiyama T (2014) Basic technology and clinical applications of the updated model of laser speckle flowgraphy to ocular diseases. Photonics 1:220–234. https://doi.org/10.3390/photonics1030220
Kikuchi S, Miyake K, Tada Y, Uchida D, Koya A, Saito Y, Ohura T, Azuma N (2019) Laser speckle flowgraphy can also be used to show dynamic changes in the blood flow of the skin of the foot after surgical revascularization. Vascular 27:242–251. https://doi.org/10.1177/1708538118810664
Rønn JH, Nerup N, Strandby RB, Svendsen MBS, Ambrus R, Svendsen LB, Achiam MP (2019) Laser speckle contrast imaging and quantitative fluorescence angiography for perfusion assessment. Langenbeck’s Arch Surg 404:505–515. https://doi.org/10.1007/s00423-019-01789-8
Nagashima Y, Ohsugi Y, Niki Y, Maeda K, Okamoto T (2015) Assessment of laser speckle flowgraphy: development of novel cutaneous blood flow measurement technique. Proc. SPIE 9792, Biophotonics Japan 2015, 979218 (9 December 2015). https://doi.org/10.1117/12.2203712
Japanese Society for Cancer of the Colon and Rectum (2019) Japanese classification of colorectal, appendiceal, and anal carcinoma: the 3d English Edition [Secondary Publication]. J Anus Rectum Colon 30;3(4):175–195. doi: https://doi.org/10.23922/jarc.2019-018. eCollection 2019
Shiokawa H, Funahashi K, Kaneko H, Teramoto T (2018) Long-term assessment of anorectal function after extensive resection of the internal anal sphincter for treatment of low-lying rectal cancer near the anus. J Anus Rectum Colon 25;1(1):29-34. Doi: https://doi.org/10.23922/jarc.2016-002. eCollection
Kawada K, Hasegawa S, Hida K, Hirai K, Okoshi K, Nomura A, Kawamura J, Nagayama S, Sakai Y (2014) Risk factors for anastomotic leakage after laparoscopic low anterior resection with DST anastomosis. Surg Endosc 28:2988–2995. https://doi.org/10.1007/s00464-014-3564-0
Luft N, Wozniak PA, Aschinger GC, Fondi K, Bata AM, Werkmeister RM, Schmidl D, Witkowska KJ, Bolz M, Garhöfer G, Schmetterer L (2016) Ocular blood flow measurements in healthy white subjects using laser speckle flowgraphy. PLoS One 11:e0168190. https://doi.org/10.1371/journal.pone.0168190
Sugiyama T, Araie M, Riva CE, Schmetterer L, Orgul S (2010) Use of laser speckle flowgraphy in ocular blood flow research. Acta Ophthalmol 88:723–729. https://doi.org/10.1111/j.1755-3768.2009.01586.x
Takahashi H, Sugiyama T, Tokushige H, Maeno T, Nakazawa T, Ikeda T, Araie M (2013) Comparison of CCD-equipped laser speckle flowgraphy with hydrogen gas clearance method in the measurement of optic nerve head microcirculation in rabbits. Exp Eye Res 108:10–15. https://doi.org/10.1016/j.exer.2012.12.003
Wang L, Cull GA, Piper C, Burgoyne CF, Fortune B (2012) Anterior and posterior optic nerve head blood flow in nonhuman primate experimental glaucoma model measured by laser speckle imaging technique and microsphere method. Invest Ophthalmol Vis Sci 53:8303–8309. https://doi.org/10.1167/iovs.12-10911
Kojima S, Sakamoto T, Matsui Y, Nambu K, Masamune K (2019) Clinical efficacy of bowel perfusion assessment during laparoscopic colorectal resection using laser speckle contrast imaging: a matched case-control study. Asian J Endosc Surg 13:329–335. https://doi.org/10.1111/ases.12759
Acknowledgments
We thank Angela Morben, DVM, ELS, from Edanz Group (https://en-author-services.edanzgroup.com/), for editing a draft of this manuscript.
Author information
Authors and Affiliations
Contributions
Study conception and design: Tomoaki Kaneko, Kimihiko Funahashi. Acquisition of data: Mitstunori Ushigome, Kimihiko Yoshida, Yasuyuki Miura, Akiharu Kurihara. Analysis and interpretation of data: Satoru Kagami, Takamaru Koda, Yoshitaka Murakami. Drafting of the manuscript: Tomoaki Kaneko. Critical revision of the manuscript: Kimihiko Funahashi.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval
This study was approved by the Ethics Committee of Toho University Omori Hospital (M17229).
Informed consent
All patients provided informed consent to undergo the procedures described in this report.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kaneko, T., Funahashi, K., Ushigome, M. et al. Noninvasive assessment of bowel blood perfusion using intraoperative laser speckle flowgraphy. Langenbecks Arch Surg 405, 817–826 (2020). https://doi.org/10.1007/s00423-020-01933-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-020-01933-9