Abstract
Purpose
The purpose of this study is to review the latest evidence on operative and perioperative management of patients with groin hernia.
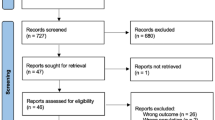
Methods
A literature review of medical databases was undertaken. Recent scientific evidence provided by quality reports was selected and discussed critically.
Results
The Shouldice repair results in low recurrence rates compared to other tissue reconstructions. However, mesh repairs are superior to tissue reconstruction in terms of recurrence. Lichtenstein’s technique remains the gold standard, with low incidence of hernia recurrence and minimal morbidity. Endoscopic techniques have been popularized during the past decades, as alternative approaches to open surgery. Both transabdominal preperitoneal repair (TAPP) and the totally extraperitoneal repair (TEP) are effective in the treatment of groin hernia, although the steep learning curve precludes popularization and may account for increased perioperative morbidity.
Conclusions
Groin hernia surgery remains an evolving field of investigation. Mesh application remains the mainstay of durable results. Individual patient factors and hernia characteristics need to be taken into account when considering the most appropriate surgical practice.
Similar content being viewed by others
References
Burcharth J, Pedersen M, Bisgaard T, Pedersen C, Rosenberg J (2013) Nationwide prevalence of groin hernia repair. PLoS One 8:e54367
Sachs M, Damm M, Encke A (1997) Historical evolution of inguinal hernia repair. World J Surg 21:218–223
Von Czerny V (1890) Studien zur Redikalbehandlung der Hernien in der Klinik des Hofraths Prof. Dr. Billroth, 1877–1889. Arch Klein Chir 40:493
Lucas-Championniére J (1892) Chirurgie Operatoire: Cure Radicale des Hernies; Aves une Étude Statistique de Deux Cents Soixante-quinze Operations et Cinquante Figures Intercalées Dans le Texte. Rueff, Paris
Bassini E (1889) Nuevo Metodo per la Cura Radicale Dell’ernia Inguinale. Padua, Prosperini
Shouldice EE (1953) The treatment of hernia. Ont Med Rev 1:1–14
Lichtenstein IL, Schulman AG, Amid PK, Montllor MM (1989) The tension-free hernioplasty. Am J Surg 157:188–193
Stoppa RE, Warlaumont CR (1989) The preperitoneal approach and prosthetic repair of groin hernia. In: Nyhus LM, Condon RE (eds) Hernia, 3rd edn. Lippincott, Philadelphia, pp 199–225
Gilbert AI (1992) Sutureless repair of inguinal hernia. Am J Surg 163:331–333
Robbins AW, Rutkow IM (1993) The mesh-plug hernioplasty. Surg Clin N Am 73:501–512
Ger R (1982) The management of certain abdominal hernia by intra-abdominal closure of the neck of the sac. Preliminary communication. Ann R Coll Surg Engl 64:342–344
Ger R (1990) Management of indirect hernias by laparoscopic closure of the neck of the sac. Am J Surg 159:370–373
Ger R, Mishrick A, Hurwitz J, Ramero C, Oddsen R (1993) Management of groin hernias by laparoscopy. World J Surg 17:46–50
Arregui ME, Davis CJ, Yucel O, Nagan RF (1992) Laparoscopic mesh repair of inguinal hernia using a preperitoneal approach: a preliminary report. Surg Laparosc Endosc 2:53–58
Dulucq JL (1991) Traitment des hernies de l’aine par mise en place d’un patch prothétique sous-péritonéal en rétropéritonéoscopie. Cah Chir 79:15–16
Bittner R, Sauerland S, Schmedt CG (2005) Comparison of endoscopic techniques vs Shouldice and other open nonmesh techniques for inguinal hernia repair: a meta-analysis of randomized controlled trials. Surg Endosc 19:605–615
Amato B, Moja L, Panico S, Persico G, Rispoli C, Rocco N, Moschetti I (2012) Shouldice technique versus other open techniques for inguinal hernia repair. Cochrane Database Syst Rev 4, CD001543
Awad SS, Fagan SP (2004) Current approaches to inguinal hernia repair. Am J Surg 188(6A Suppl):9S–16S
Li J, Ji Z, Cheng T (2012) Comparison of open preperitoneal and Lichtenstein repair for inguinal hernia repair: a meta-analysis of randomized controlled trials. Am J Surg 204:769–778
Sanjay P, Watt DG, Ogston SA, Alijani A, Windsor JA (2012) Meta-analysis of Prolene Hernia System mesh versus Lichtenstein mesh in open inguinal hernia repair. Surgeon 10:283–289
Li J, Ji Z, Li Y (2012) Comparison of mesh-plug and Lichtenstein for inguinal hernia repair: a meta-analysis of randomized controlled trials. Hernia 16:541–548
Reddy VM, Sutton CD, Bloxham L, Garcea G, Ubhi SS, Robertson GS (2007) Laparoscopic repair of direct inguinal hernia: a new technique that reduces the development of postoperative seroma. Hernia 1:393–396
Lovisetto F, Zonta S, Rota E, Mazzilli M, Bardone M, Bottero L, Faillace G, Longoni M (2007) Use of human fibrin glue (Tissucol) versus staples for mesh fixation in laparoscopic transabdominal preperitoneal hernioplasty: a prospective, randomized study. Ann Surg 245:222–231
Fortelny RH, Petter-Puchner AH, May C, Jaksch W, Benesch T, Khakpour Z, Redl H, Glaser KS (2011) The impact of atraumatic fibrin sealant vs. staple mesh fixation in TAPP hernia repair on chronic pain and quality of life: results of a randomized controlled study. Surg Endosc 26:249–254
Tolver MA, Rosenberg J, Juul P, Bisgaard T (2013) Randomized clinical trial of fibrin glue versus tacked fixation in laparoscopic groin hernia repair. Surg Endosc 27:2727–2733
Bringman S, Ek A, Haglind E, Heikkinen T, Kald A, Kylberg F, Ramel S, Wallon C, Anderberg B (2001) Is a dissection balloon beneficial in totally extraperitoneal endoscopic hernioplasty (TEP)? A randomized prospective multicenter study. Surg Endosc 15:266–270
Tamme C, Garde N, Klingler A, Hampe C, Wunder R, Köckerling F (2005) Totally extraperitoneal inguinal hernioplasty with titanium-coated lightweight polypropylene mesh: early results. Surg Endosc 19:1125–1129
Liem MS, van der Graaf Y, van Steensel CJ, Boelhouwer RU, Clevers GJ, Meijer WS, Stassen LP, Vente JP, Weidema WF, Schrijvers AJ, van Vroonhoven TJ (1997) Comparison of conventional anterior surgery and laparoscopic surgery for inguinal-hernia repair. N Engl J Med 336:1541–1547
Bittner R, Arregui ME, Bisgaard T, Dudai M, Ferzli GS, Fitzgibbons RJ, Fortelny RH, Klinge U, Kockerling F, Kuhry E, Kukleta J, Lomanto D, Misra MC, Montgomery A, Morales-Conde S, Reinpold W, Rosenberg J, Sauerland S, Schug-Pass C, Singh K, Timoney M, Weyhe D, Chowbey P (2011) Guidelines for laparoscopic (TAPP) and endoscopic (TEP) treatment of inguinal hernia [International Endohernia Society (IEHS)]. Surg Endosc 25:2773–2843
Dulucq JL, Wintringer P, Mahajna A (2006) Totally extraperitoneal (TEP) hernia repair after radical prostatectomy or previous lower abdominal surgery: is it safe? A prospective study. Surg Endosc 20:473–476
Wauschkuhn CA, Schwarz J, Bittner R (2009) Laparoscopic transperitoneal inguinal hernia repair (TAPP) after radical prostatectomy: is it safe? Results of prospectively collected data of more than 200 cases. Surg Endosc 23:973–977
O’Reilly EA, Burke JP, O’Connell PR (2012) A meta-analysis of surgical morbidity and recurrence after laparoscopic and open repair of primary unilateral inguinal hernia. Ann Surg 255:846–853
Koning GG, Wetterslev J, van Laarhoven CJ, Keus F (2013) The totally extraperitoneal method versus Lichtenstein’s technique for inguinal hernia repair: a systematic review with meta-analyses and trial sequential analyses of randomized clinical trials. PLoS One 8:e52599
Yang J, da Tong N, Yao J, Chen W (2013) Laparoscopic or Lichtenstein repair for recurrent inguinal hernia: a meta-analysis of randomized controlled trials. ANZ J Surg 83:312–318
Sgourakis G, Dedemadi G, Gockel I, Schmidtmann I, Lanitis S, Zaphiriadou P, Papatheodorou A, Karaliotas C (2013) Laparoscopic totally extraperitoneal versus open preperitoneal mesh repair for inguinal hernia recurrence: a decision analysis based on net health benefits. Surg Endosc 27:2526–2541
Lau H (2004) Endoscopic totally extraperitoneal inguinal hernioplasty for recurrence after open repair. ANZ J Surg 74:877–880
Bracale U, Melillo P, Pignata G, Di Salvo E, Rovani M, Merola G, Pecchia L (2012) Which is the best laparoscopic approach for inguinal hernia repair: TEP or TAPP? A systematic review of the literature with a network meta-analysis. Surg Endosc 26:3355–3366
Antoniou SA, Antoniou GA, Bartsch DK, Fendrich V, Koch OO, Pointner R, Granderath FA (2013) Transabdominal preperitoneal versus totally extraperitoneal repair of inguinal hernia: a meta-analysis of randomized studies. Am J Surg 206:245–252
Kehlet H, Aasvang E (2005) Groin hernia repair: anesthesia. World J Surg 29:1058–1061
Mazaki T, Mado K, Masuda H, Shiono M (2013) Antibiotic prophylaxis for the prevention of surgical site infection after tension-free hernia repair: a Bayesian and frequentist meta-analysis. J Am Coll Surg 217:788–801.e1-4.
Gravante G, Filingeri V, Venditti D (2008) A meta-analytic approach to ilioinguinal nerve excision or preservation during open inguinal hernia repair. Ann Surg 247:1078, discussion 1078–80
Johner A, Faulds J, Wiseman SM (2011) Planned ilioinguinal nerve excision for prevention of chronic pain after inguinal hernia repair: a meta-analysis. Surgery 150:534–541
Hsu W, Chen CS, Lee HC, Liang HH, Kuo LJ, Wei PL, Tam KW (2012) Preservation versus division of ilioinguinal nerve on open mesh repair of inguinal hernia: a meta-analysis of randomized controlled trials. World J Surg 36:2311–2319
Tekatli H, Schouten N, van Dalen T, Burgmans I, Smakman N (2012) Mechanism, assessment, and incidence of male infertility after inguinal hernia surgery: a review of the preclinical and clinical literature. Am J Surg 204:503–509
Sajid MS, Kalra L, Parampalli U, Sains PS, Baig MK (2013) A systematic review and meta-analysis evaluating the effectiveness of lightweight mesh against heavyweight mesh in influencing the incidence of chronic groin pain following laparoscopic inguinal hernia repair. Am J Surg 205:726–736
Conflicts of interest
None.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Antoniou, S.A., Pointner, R. & Granderath, F.A. Current treatment concepts for groin hernia. Langenbecks Arch Surg 399, 553–558 (2014). https://doi.org/10.1007/s00423-014-1212-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-014-1212-8