Abstract
Background
Chronic groin pain after inguinal hernia repair, a serious problem, is caused by entrapment of the ilioinguinal nerve either by mesh or development of fibrosis. Division of the ilioinguinal nerve during hernioplasty has been found to reduce the incidence of chronic groin pain. However, the traditional approach favors preservation of the ilioinguinal nerve during open hernia repair.
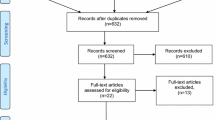
Methods
We conducted a systematic review and meta-analysis of randomized controlled trials that compared the outcomes of preservation versus division of the ilioinguinal nerve during open mesh repair of inguinal hernia. The primary outcome was the incidence of groin pain; secondary outcomes were numbness and sensory loss.
Results
We reviewed six trials with 1,286 patients. We found no difference between the groups for the incidence of groin pain or numbness at 1, 6, and 12 months after open mesh inguinal repair. The incidence of sensory loss or change was significantly higher in the division group than in the preservation group at 6 months [risk ratio (RR) 1.25; 95 % confidence interval (CI) 1.02–1.53] and at 12 months (RR 1.55; 95 % CI 1.01–2.37) postoperatively. No significant differences between the groups were noted at any other points in time.
Conclusions
Preservation of the ilioinguinal nerve during open mesh repair of inguinal hernia is associated with a decreased incidence of sensory loss at 6 and 12 months postoperatively compared with that of the division technique. No significant differences were found between the groups for chronic groin pain or numbness.





Similar content being viewed by others
References
Poobalan AS, Bruce J, Smith WC et al (2003) A review of chronic pain after inguinal herniorrhaphy. Clin J Pain 19:48–54
Bay-Nielsen M, Perkins FM, Kehlet H et al (2001) Pain and functional impairment 1 year after inguinal herniorrhaphy: a nationwide questionnaire study. Ann Surg 233:1–7
Mui WL, Ng CS, Fung TM et al (2006) Prophylactic ilioinguinal neurectomy in open inguinal hernia repair: a double-blind randomized controlled trial. Ann Surg 244:27–33
Aasvang E, Kehlet H (2005) Surgical management of chronic pain after inguinal hernia repair. Br J Surg 92:795–801
Alfieri S, Rotondi F, Di Giorgio A et al (2006) Influence of preservation versus division of ilioinguinal, iliohypogastric, and genital nerves during open mesh herniorrhaphy: prospective multicentric study of chronic pain. Ann Surg 243:553–558
Diitrik GW, Ridl K, Kuhn JA et al (2004) Routine ilioinguinal nerve excision in inguinal hernia repairs. Am J Surg 188:736–740
Smeds S, Löfström L, Eriksson O (2010) Influence of nerve identification and the resection of nerves ‘at risk’ on postoperative pain in open inguinal hernia repair. Hernia 14:265–270
Tsakayannis DE, Kiriakopoulos AC, Linos DA (2004) Elective neurectomy during open, “tension free” inguinal hernia repair. Hernia 8:67–69
Ravichandran D, Kalambe BG, Pain JA (2000) Pilot randomized controlled study of preservation or division of ilioinguinal nerve in open mesh repair of inguinal hernia. Br J Surg 87:1166–1167
Malekpour F, Mirhasgemi SH, Hajinasrolah MD et al (2008) Ilioinguinal nerve excision in open mesh repair of inguinal hernia: results of randomized clinical trial—simple solution for difficult problem. Am J Surg 195:735–740
Johner A, Faulds J, Wiseman SM (2011) Planned ilioinguinal nerve excision for prevention of chronic pain after inguinal hernia repair: a meta-analysis. Surgery 150:534–541
Crea N, Pata G (2010) Effects of prophylactic ilioinguinal nerve excision in mesh groin hernia repair: short- and long-term follow-up of a randomized clinical trial. Am Surg 76:1275–1281
Karakayali F, Oksuz E, Turk E et al (2010) Effectiveness if multiple neurectomies to prevent chronic groin pain after tension-free hernia repair. Int Surg 95:40–48
Liberati A, Altman DG, Tetzlaff J et al (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol 62:e1–e34
Moher D, Cook DJ, Eastwood S et al (2000) Improving the quality of reports of meta-analyses of randomised controlled trials: the QUOROM statement. QUOROM Group. Br J Surg 87:1448–1454
DerSimonian R, Laird N (1986) Meta-analysis in clinical trials. Control Clin Trials 7:177–188
Picchio M, Palimento D, Attanasio U et al (2004) Randomized controlled trial of preservation or elective division of ilioinguinal nerve on open inguinal hernia repair with polypropylene mesh. Arch Surg 139:755–758
Trabucco EE (1993) The office hernioplasty and the Trabucco repair. Ann Ital Chir 64:127–149
Wanz GE (1984) Complications of inguinal hernial repair. Surg Clin N Am 64:287–298
Amid PK, Hiatt JR (2007) New understanding of the causes and surgical treatment of postherniorrhaphy inguinodynia and orchialgia. J Am Coll Surg 205:381–385
Starling JR, Harms BA (1989) Diagnosis and treatment of genitofemoral and ilioinguinal neuralgia. World J Surg 13:586–591. doi:10.1007/BF01658875
Vuilleumier H, Hübner M, Demartines N (2009) Neuropathy after herniorrhaphy: indication for surgical treatment and outcome. World J Surg 33:841–845. doi:10.1007/s00268-008-9869-1
Lichtenstein IL, Shulman AG, Amid PK et al (1988) Cause and prevention of postherniorrhaphy neuralgia: a proposed protocol for treatment. Am J Surg 155:786–790
Amid PK (2004) Causes, prevention, and surgical treatment of postherniorrhaphy neuropathic inguinodynia: triple neurectomy with proximal end implantation. Hernia 8:343–349
Conflict of Interest
The authors (Wayne Hsu, Ching-Shyang Chen, Hung-Chia Lee, Hung-Hua Liang, Li-Jen Kuo, Po-Li Wei, and Ka-Wai Tam) have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hsu, W., Chen, CS., Lee, HC. et al. Preservation Versus Division of Ilioinguinal Nerve on Open Mesh Repair of Inguinal Hernia: A Meta-analysis of Randomized Controlled Trials. World J Surg 36, 2311–2319 (2012). https://doi.org/10.1007/s00268-012-1657-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-012-1657-2