Abstract
Purpose
Endothelial dysfunction is an early and integral event in the development of atherosclerosis and coronary artery disease (CAD). Reduced NO bioavailability, oxidative stress, vasoconstriction, inflammation and senescence are all implicated in endothelial dysfunction. However, there are limited data examining associations between these pathways and direct in vivo bioassay measures of endothelial function in CAD patients. This study aimed to examine the relationships between in vivo measures of vascular function and the expression of atherogenic risk-modulating proteins in endothelial cells (ECs) isolated from the radial artery of CAD patients.
Methods
Fifty-six patients with established CAD underwent trans-radial catheterization. Prior to catheterization, radial artery vascular function was assessed using a) flow-mediated dilation (FMD), and b) exercise-induced dilation in response to handgrip (HE%). Freshly isolated ECs were obtained from the radial artery during catheterization and protein content of eNOS, NAD(P)H oxidase subunit NOX2, NFκB, ET-1 and the senescence markers p53, p21 and p16 were evaluated alongside nitrotyrosine abundance and eNOS Ser1177 phosphorylation.
Results
FMD was positively associated with eNOS Ser1177 phosphorylation (r = 0.290, P = 0.037), and protein content of p21 (r = 0.307, P = 0.027) and p16 (r = 0.426, P = 0.002). No associations were found between FMD and markers of oxidative stress, vasoconstriction or inflammation. In contrast to FMD, HE% was not associated with any of the EC proteins.
Conclusion
These data revealed a difference in the regulation of endothelium-dependent vasodilation measured in vivo between patients with CAD compared to previously reported data in subjects without a clinical diagnosis, suggesting that eNOS Ser1177 phosphorylation may be the key to maintain vasodilation in CAD patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Coronary artery disease (CAD) is a leading cause of death in the Western world with over 370,000 deaths annually (Mozaffarian et al. 2016). Atherosclerosis is proposed as the underlying cause of CAD (Ross 1993). In this context, endothelial (dys)function has emerged as an early and integral event in the atherogenic process (Davignon and Ganz 2004; Thijssen et al. 2019). Indeed, markers of endothelial function are typically lower in CAD patients compared to aged-matched controls (Oz et al. 2012) and worsen with the progression of CAD (Manganaro et al. 2014).
Endothelial dysfunction is often characterized by a reduction in nitric oxide (NO) bioavailability. NO bioavailability is determined by the balance between NO synthesis and scavenging by superoxide anions and related reactive oxygen species. It is hypothesized that increased production of reactive oxygen species (Elahi et al. 2009) plays a major role in reduced NO bioavailability within CAD patients (Cai and Harrison 2000; Ohara et al. 1993). In support of this, elevated markers of oxidative stress have been associated with coronary endothelial dysfunction in CAD patients (Lavi et al. 2008). Furthermore, mRNA expression of NOX2, the catalytic subunit of the NAD(P)H oxidase complex, was elevated in the coronary arteries of CAD patients compared to those without CAD (Guzik et al. 2006). Age-associated reductions in endothelial function are also associated with markers of oxidative stress [NADPH oxidase-p47phox (Donato et al. 2009) and nitrotyrosine (Donato et al. 2007)].
In contrast, coronary endothelial dysfunction was not associated with reduced basal NO production in CAD patients (Lavi et al. 2008). In addition, age-associated reductions in endothelium-dependent dilation were not associated with eNOS protein content or eNOS Ser1177 phosphorylation (Donato et al. 2007; Pierce et al. 2011). Indeed, NO production was increased in hypercholesterolemic rabbits despite the severely impaired endothelium-dependent dilation (Minor et al. 1990). This suggests that signaling pathways leading to eNOS activation remained intact. In summary, the above suggests a causal role for increased NO scavenging in the development of endothelial dysfunction and CAD. Conversely, reduced NO production appears unlikely to play a major role in the development of CAD.
Increased reactive oxygen species production may also stimulate the expression of other pro-atherogenic factors. Endothelin 1 (ET-1) (Lerman et al. 1991; Donato et al. 2009) and nuclear factor κB (NFκB) (Cominacini et al. 2005; Real et al. 2010; Silver et al. 2007; Donato et al. 2007) were elevated in CAD patients and/or subjects with an atherosclerotic-prone phenotype. Endothelial ET-1 expression is associated with reduced endothelium-dependent dilation in aging (Donato et al. 2007, 2009), suggesting its involvement in endothelial dysfunction.
A pro-oxidant and -inflammatory milieu may trigger cellular senescence in the vasculature (Katsuumi et al. 2018; Campisi and d'Adda di Fagagna 2007; Childs et al. 2017). Cellular senescence is a stress response resulting in irreversible growth arrest of a cell. Senescence has emerged as a potential driver for endothelial dysfunction (Donato et al. 2015) and atherosclerotic diseases (Katsuumi et al. 2018). Although there is limited evidence toward endothelial cell (EC) senescence and endothelial (dys)function, the expression of senescence markers (p53, p21 and p16) was inversely associated with endothelium-dependent dilation in older humans and mice (Bhayadia et al. 2016; Rossman et al. 2017). These studies may suggest the potential role of senescent phenotype in endothelial dysfunction and subsequent development of atherosclerosis.
All the above demonstrate a complex vicious cycle with multiple interactions between markers of oxidative stress, inflammation, vasoconstriction and cellular senescence. All these directly and/or indirectly have an impact on NO bioavailability and thereby contribute to the development of CAD. However, how the changes in these atherogenic-modulating proteins influence the progression of endothelial dysfunction in patients with established CAD has limited direct evidence.
Most studies have used flow-mediated dilation (FMD) to assess in vivo endothelial function in humans. However, recent data from our team have shown impaired FMD but preserved dilation in response to localized exercise in CAD patients (Tryfonos et al. 2020). As such, these tests may reflect different components of vascular function. Hyperemic response to exercise represents an integrated response involving autonomic activity and numerous endothelium- and non-endothelium-dependent vasoactive systems (Hellsten et al. 2012). Importantly, exercise-induced dilation demonstrates a redundancy where there is an ability to compensate for an impaired pathway with alternative mechanisms (Hellsten et al. 2012). Assessing multiple pathways using distinct stimuli provides important information when presented alongside measurement of FMD (Nyberg et al. 2012). It is currently unknown whether exercise-induced dilation in CAD patients is associated with changes in the expression of atherogenic-modulating proteins.
Therefore, the primary aim of this study was to determine whether the endothelial expression of atherogenic-modulating proteins can predict FMD and/or exercise vasomotor responses in patients with established CAD. We hypothesized that both FMD and exercise-induced dilation would be negatively associated with the expression of proteins related to NO scavenging, inflammation, vasoconstriction and senescence. In contrast, there would be no relation between these tests and eNOS protein content or Ser1177 phosphorylation as markers of NO production.
Methods
Ethical approval
All participants provided written informed consent, and the study was approved by the Liverpool East NHS Research Ethics Committee (approval reference no. 13/NW/0088) and conformed to the Declaration of Helsinki.
Participants
Sixty-four patients undergoing prospective percutaneous transluminal coronary angiography (PTCA) and/or percutaneous coronary intervention (PCI; angioplasty) were recruited from Liverpool Heart and Chest Hospital (LHCH). Patients were excluded if they were unable to give informed consent or had undergone a trans-radial cardiac catheterization or acute coronary syndrome within the last 3 months. Eight patients had angiographically normal coronaries following PTCA and were retrospectively excluded. As such, data from 56 patients with established CAD were included in this study. A summary of patient characteristics, medications, hemodynamic variables, and previous catheterization is included in Table 1.
Study design
Vascular function measurements were assessed prior to catheterization (1–4 h). In brief, the catheterized radial artery was assessed using two non-invasive measurements: (a) flow-mediated dilation (FMD) followed by (b) vascular dilation to incremental handgrip exercise. The order of these tests was maintained in all participants. A standardized period of 10 min was observed between tests to allow artery function to recover to baseline levels. Patients then underwent PTCA and/or PCI and ECs were collected from the catheterized radial artery, as described below.
Trans-radial cardiac catheterization and EC collection
PTCA and/or PCI were performed predominantly via the right radial artery under local anesthesia, as previously described (Tryfonos et al. 2020). Briefly, the catheterized artery was punctured with a 21-gage needle and a 5-7F hydrophilic sheath introducer (PreludeEase, MeritMedical, UK) was inserted. All patients received a weight-adjusted dose of heparin. Thirty patients received an additional ~ 1.5 mg/ml of vasodilator isosorbide di-nitrate, as indicated by the interventional cardiologist. Once the procedure was finished, the J-shaped guidewire (3 mm J TEF 150 cm × 0.35″, KIMAL, UK) was transferred immediately to ice-cold dissociation solution (~ 30 ml) (0.5% bovine serum albumin, 2 mmol/L EDTA, and 100 ug/mL heparin in Dulbecco's Phosphate-Buffered Saline (DPBS)). An additional sterile J-shaped guidewire was advanced into the radial artery (~ 3–4 cm above the sheath), run back and forth to collect ECs and transferred immediately to the dissociation buffer. All introducer sheaths were removed at the end of the procedure.
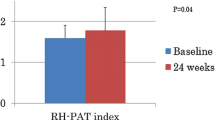
Vascular function assessment
Vascular function measurements were completed in a quiet room between 0800 and 1100 h. Patients were fasted (including caffeine and alcohol) and asked to abstain from exercise and cigarettes for 12 h before the visit (Thijssen et al. 2019, 2011). Part of the vascular data (33 patients) has been published elsewhere (Tryfonos et al. 2020), where the methods have been described in detail. Briefly, patients rested in the supine position for > 10 min before blood pressure (BP) and heart rate (HR) were measured using an automated sphygmomanometer (GE Pro 300V2, Dinamap, Tampa, FL, USA). FMD and arterial response to exercise were then measured in the catheterized radial artery (10–15 cm proximal from the scaphoid bone in the wrist), using a 12-MHz multi-frequency linear array probe attached to a high-resolution ultrasound machine (T3000; Terason, Burlington, MA, USA) (Tryfonos et al. 2020). For the exercise protocol, patients performed a 3 × 3-min bout of handgrip exercise, in a seated position, at 5%, 10% and 15% of their pre-determined maximal voluntary contraction (MVC) (Takei 5420 Grip-D Digital Hand Grip Dynamometer, Japan), with 1-min rest between bouts. Arterial diameter/velocity recordings were measured at baseline and during the 1-min rest. The percentage difference in diameter from the baseline to peak in response to handgrip exercise (the maximum value at either 5%, 10% or 15% MVC) was then calculated (HE%) and used for further analysis. Custom-designed edge-detection and wall-tracking software was used to analyze both the FMD and handgrip exercise to minimize investigator bias (Woodman et al. 2001; Thijssen et al. 2011).
Immunofluorescence microscopy
EC isolation and protein expression measurements were performed as previously described (Pierce et al. 2011; Donato et al. 2007). Briefly, ECs were recovered from the two J-shaped guidewires by washing and centrifugation. Cells were then fixed with 3.7% formaldehyde, plated on glass slides (VWR, REF number: 631-0705, USA) and frozen at − 80 °C until analysis. At the time of analysis, cells were re-hydrated and incubated for 1 h at room temperature with primary antibodies against eNOS (610,297, BD, USA), Phospho-eNOS Ser1177 (peNOS Ser1177) (07-428-I, Merck), NAD(P)H oxidase subunit NOX2 (kind gift from Prof Mark Quinn, Montana State University), tumor suppressor protein p53 (p53) (Ab26, Abcam, UK), cyclin-dependent kinase inhibitor 1 (p21) (Ab109520, Abcam, UK), cyclin-dependent kinase inhibitor 2A (p16) (Abc51243, Abcam, UK), nitrotyrosine (Ab7048, Abcam, UK), ET-1 (PA3-067, Thermo Fisher Scientific, USA), NFκB p65 (NB100-56,712, Novus, UK). Cells were also stained for vascular–endothelial (VE) cadherin (NB600-1409, Novus, UK) for positive identification of the endothelial phenotype and DAPI for nuclear integrity.
Image capture
Images were acquired using an inverted confocal microscope (Zeiss LSM-710, Carl Zeiss, Germany) with a 63 × 1.3NA oil immersion objective. Positive staining for VE cadherin coupled with a single intact nucleus was used to reliably select ECs (Casey et al. 2017). DAPI was excited using the 405 nm line of the diode laser and detected with 371–422 nm emission. Alexa Fluor 488 was excited with the 488 nm line of the argon laser and detected with 493–559 nm emission. Alexa Fluor 546 and 633 fluorophores were excited with 543 nm and 633 nm lines of the helium–neon laser and 548–623 nm and 638–747 nm emission, respectively. The images were acquired at a resolution of 1,024 X 1,024 pixels and stored in 24-bit tagged image format file format.
Image analysis
All images were analyzed using ImagePro Plus 5.1 (Media Cybernetics Inc, Bethesda, MD, USA). To ensure only the cytosolic fraction was assessed, nuclear regions of the ECs, identified through the DAPI stain, were extracted from the rest of the EC image identified using the VE cadherin image. The resulting mask was then overlaid onto the corresponding protein of interest image. Mean fluorescence intensity of the protein of interest signal was then quantified within the endothelial cytosolic-specific area. EC protein expression data are reported as ratios to human umbilical vein EC (HUVEC) protein expression. Slides were systematically scanned and at least 25 consecutive ECs were captured and analyzed for each protein in each patient, as previously suggested (Colombo et al. 2002). A single technician analyzed each batch of slides. Technicians were blinded to subject identity during the staining and analysis procedures.
Statistical analysis
All statistical analyses were performed using IBM SPSS statistics for Windows, version 25.0. (Armonk, NY: IBM Corp). Pearson’s correlation analysis was used to determine relations of interest. In addition, hierarchical multiple regression models were performed when statistically significant Pearson’s correlations revealed between protein expression and in vivo vascular responses (FMD and/or HE%), to further examine whether patients’ characteristics (sex, age, BMI, and/or MAP) explain such associations. Data are presented as mean ± SD and statistical significance for all analyses was set at P ≤ 0.05.
Results
Out of 56 patients, FMD was performed in 54 patients (2 × equipment failure) and HE data were available in 46 patients (2 × equipment failure, 1 × avoid exercise due to dizziness following FMD, 2 × previous injury to their hand, 1 × lack of time due to catheterization preparation, 4 × quality of images). In addition, EC samples were not taken from 2 patients (2 × complications during catheterization).
Relationship between EC protein expression with endothelium-dependent dilation and exercise response
FMD was positively correlated with eNOS Ser1177 phosphorylation (r = 0.290, P = 0.037) (Fig. 1) and p16 (r = 0.426, P = 0.002) and p21 protein expression (r = 0.307 P = 0.027) (Fig. 2). When eNOS Ser1177 phosphorylation was normalized to eNOS content, the significant correlation was no longer present (r = 0.218, P = 0.121) (Table 2). Further, hierarchical multiple regression models suggested that p16 protein expression remained significantly associated with FMD (P = 0.008), despite accounting for MAP, BMI, sex and age. In contrast, p21 and eNOS Ser1177 phosphorylation associations with FMD appeared to be affected by the patients’ characteristics (P = 0.099 and P = 0.175, respectively), and the limiting factor in both cases was the MAP (P = 0.129 and P = 0.522). In contrast, BMI, sex and age appeared to not affect the associations between p21 and eNOS Ser1177 phosphorylation with FMD (P < 0.05). No significant association was observed between FMD and eNOS, NOX2, ET-1 and NFκB protein expression or nitrotyrosine abundance in patient ECs (Table 2). HE-mediated dilation was not correlated with any of the proteins examined (Table 2).
Positive correlation between flow-mediated dilation (FMD%) and eNOS Ser1177 phosphorylation (peNOS Ser1177) in endothelial cells (ECs) obtained from radial arteries of coronary artery disease patients. Representative images of the immunofluorescence images of peNOS Ser1177 from CAD patients with low and high FMD are shown. AU: arbitrary units EC protein expression data are reported as ratios to human umbilical vein endothelial cells (HUVEC) protein expression
Positive correlation between flow-mediated dilation (FMD%) with p16 (a) and p21 (b) protein expression in endothelial cells (ECs) obtained from radial arteries of coronary artery disease patients. Representative images of the immunofluorescence images of p16 (a) and p21 (b) from CAD patients with low and high FMD are shown. AU arbitrary units EC protein expression data are reported as ratios to human umbilical vein endothelial cells (HUVEC) protein expression, p16 cyclin-dependent kinase inhibitor 2A, p21 cyclin-dependent kinase inhibitor 1
Relationship between endothelium-dependent dilation (FMD) and arterial response to exercise
There was no correlation between FMD and the percentage change in diameter (%HE) during handgrip exercise (r = − 0.015, P = 0.985).
Associations among EC protein expression in CAD patients
eNOS Ser1177 phosphorylation is related to oxidative stress and senescence markers
There was a significant positive correlation between eNOS Ser1177 phosphorylation and NOX2 (r = 0.306, P = 0.029). When eNOS Ser1177 was normalized to eNOS content (peNOS Ser1177/eNOS), the correlation with NOX2 was close to significant (r = 0.271, P = 0.055). eNOS Ser1177 phosphorylation was also correlated with the expression of p21 (r = 0.269, P = 0.049) (Fig. 3). eNOS content and Ser1177 phosphorylation were not associated with any other EC protein (Table 3).
Positive relations between eNOS Ser1177 phosphorylation with NOX2 (a) and senescence marker p21 (b) of endothelial cells (ECs) obtained from radial artery of coronary artery disease patients. NFκB is correlated with ET-1 (c) and NOX2 (d). AU arbitrary units EC protein expression data are reported as ratios to human umbilical vein endothelial cells (HUVEC) protein expression; NOX2: NADPH oxidase subunit 2, p21 cyclin-dependent kinase inhibitor 1, NFκB nuclear factor kappa-light-chain-enhancer of activated B cells, ET-1 endothelin-1, peNOS phospho-endothelial nitric oxide synthase
Relation between NFκB expression with vasoconstriction and oxidative stress
A strong positive correlation was observed between ET-1 and inflammatory marker NFκB (r = 0.633, P < 0.0001). A weak correlation was also reported between the expression of NOX2 and NFκB (r = 0.283, P = 0.046) (Fig. 3). NFκB was not associated with any other EC protein (Table 3).
Senescence markers are related to oxidative stress
The expression of p16 (r = 0.638, P < 0.0001) p21 (r = 0.308, P = 0.025) and p53 (r = 0.434, P = 0.001) in ECs was positively correlated with the expression of nitrotyrosine. In addition, the expression of NOX2 was positively associated with the expression of p21(r = 0.423, P = 0.002) and p53 (r = 0.459, P = 0.001). Finally, there was a strong positive correlation between the expression of the senescence markers p21 and p53 (r = 0.598, P < 0.0001). These correlations are presented in Fig. 4. The senescence and oxidative stress markers were not associated with any other EC proteins (Table 3).
Positive correlations between senescence and oxidative stress expression of endothelial cells (ECs) obtained from radial artery of coronary artery disease patients. NT expression is related to p16 (a), p21 (b) and p53 (c), NOX2 expression is correlated to p21 (d) and p53 (e), and p21 expression is associated with p53 (f). AU arbitrary units EC protein expression data are reported as ratios to human umbilical vein endothelial cells (HUVEC) protein expression, NT nitrotyrosine, p16 Cyclin-dependent kinase inhibitor 2A, p21 cyclin-dependent kinase inhibitor 1, p53 tumor protein 53, NOX2 NADPH oxidase subunit 2
Discussion
To our knowledge, the current study is the first to assess relationships between endothelium-dependent vasodilation and the expression of atherogenic risk-modulating proteins in patients with established CAD. Contrary to our hypothesis, the key novel findings were that: (1) endothelium-dependent dilation, assessed using FMD, was positively associated with eNOS Ser1177 phosphorylation seen in the isolated ECs and (2) markers of oxidative stress (NOX2 and nitrotyrosine) were not associated with FMD. In addition, positive associations were observed between FMD and the protein expression of the senescence markers p16 and p21. Interestingly, markers of inflammation (NFκB) and vasoconstriction (ET-1) were not associated with FMD. Moreover, no associations were observed between any of the proteins measured and arterial dilation in response to handgrip exercise. This finding together with the absence of correlation between FMD and exercise-induced vasodilation may suggest that different mechanisms underpin such responses.
Association between endothelium-dependent dilation (FMD) and proteins involved in no production and scavenging
Previous work in individuals with CVD risk factors but without established CAD suggests that impaired endothelium-dependent dilation in humans is largely related to elevated oxidative stress (Donato et al. 2009; Seals et al. 2011; Gates et al. 2007; Lavi et al. 2008; O'Driscoll et al. 1999; O'Driscoll et al. 1997a, b; Cheetham et al. 2000) rather than impaired NO production (Donato et al. 2009; Pierce et al. 2011). In contrast with these observations in pre-clinical populations, we report that markers of oxidative stress (expression of NOX2 and nitrotyrosine content) were not associated with endothelium-dependent vasodilation in patients with established CAD. However, total eNOS Ser1177 phosphorylation, reflecting the overall activation of eNOS, was positively associated with endothelium-dependent dilation in these patients. Together with the lack of association between FMD and eNOS content or peNOS Ser1177/eNOS ratio may suggest that both lower eNOS content and ability to phosphorylate the available eNOS combine to reduce overall eNOS phosphorylation. The overall phosphorylation of eNOS is relevant (Hambrecht et al. 2003) as this appears to determine NO production and not the content or ability to phosphorylate the available eNOS (Mount et al. 2007).
Taken together the above evidence may indicate a difference in the regulation of endothelium-dependent dilation between patients with established CAD and pre-clinical subjects. Our data seem to suggest that further elevations in oxidative stress do not contribute to progressive declines in endothelium-dependent vasodilation in patients with diagnosed CAD. On the other hand, the activation of eNOS by Ser1177 phosphorylation becomes increasingly important to maintain NO production. In support of this, Hambrecht et al. (2003) reported a positive association between increased eNOS Ser1177 phosphorylation and endothelium-dependent dilation in the arteries of CAD patients. Furthermore, a number of drugs used to treat CVD and improve endothelium-dependent dilation act by stimulating eNOS Ser1177 phosphorylation (Huang 2009). Estrogens (Hisamoto et al. 2001), statins (Kureishi et al. 2000) and peroxisome proliferator activated receptors agonists (Aikawa et al. 2004) are all examples of such drugs.
In our ECs, we also demonstrated a positive association between endothelial eNOS Ser1177 phosphorylation and oxidative stress (NOX2 protein content). It has previously been shown that reactive oxygen species can modulate NO production by influencing eNOS activity (Li et al. 2014). Specifically, H2O2 has been shown to increase phosphorylation of eNOS at Ser1177 (Thomas et al. 2002). As such, the association between eNOS Ser1177 phosphorylation and NOX2 could reflect an attempt to increase NO production and overcome elevated NO scavenging by superoxide, as it has been hypothesized in aging (Donato et al. 2007, 2015).
Association of endothelium-dependent dilation with markers of endothelial senescence
Cellular senescence, a stress-response resulting in irreversible growth arrest of a cell, is emerging as a potential driver of endothelial dysfunction and the development of atherosclerosis (Katsuumi et al. 2018). The accumulation of these cells alongside the pro-inflammatory and pro-oxidative phenotype of these cells have been proposed as mediators of the adverse effects of senescence (Childs et al. 2015; Minamino et al. 2002). Direct evidence associating senescence with endothelial function in humans is limited. However, recent work suggests that age-associated reductions in endothelium-dependent dilation were negatively associated with endothelial p53, p21 and p16 protein content (Rossman et al. 2017). In contrast to this, we report that FMD was positively associated with endothelial protein content of p21 and p16 in patients with established CAD. These positive associations were unexpected. Given the lack of human studies investigating vascular senescence in CAD, we cannot fully explain these observations. To explore the above paradoxical associations, we ran hierarchical multiple regressions accounting for patients’ characteristics. The results showed that endothelial senescence (at least p16 protein expression) was associated with higher endothelial function in these patients independently of individual characteristics. Mean arterial pressure appeared to influence the association between FMD and p21 expression. Endothelial (dys)function and arterial pressure are mechanistically (Konukoglu and Uzun 2017) and statistically related (Holder et al. 2021). Thus, it is difficult to differentiate the effect of arterial pressure on FMD, especially in our study which included uncontrolled hypertensives, controlled hypertensive and non-hypertensive patients. The prevailing hypothesis is that endothelial senescence leads to vascular dysfunction. However, studies in murine models have shown that knockout of p53 (Mercer et al. 2005) and p21 (Khanna 2009) resulted in greater severity of atherosclerotic lesions. As such, the role of senescence within the vasculature may depend on the stage of the progression of atherosclerosis (Childs et al. 2015, 2016). It is possible that senescence initially plays a protective role in atherosclerosis. Indeed, it has been proposed that senescent cells may delay the atherosclerotic process in the beginning as they prevent cell growth by activating cell arrest and/or perhaps apoptosis pathways (Mercer et al. 2005). Future studies should test the causal contribution of senescence at different stages of CAD pathology.
Markers of senescence (p53, p21 and p16) were associated with oxidative stress (EC nitrotyrosine abundance and NOX2 protein content). These associations are supported by previous work showing that oxidative stress leads to senescence through the activation of p53/p21 and p16 pathways (Bhayadia et al. 2016; Childs et al. 2015; Muñoz-Espín and Serrano 2014). Surprisingly, endothelial inflammation (NFκB) was not associated with any marker of senescence. Importantly, NFκB is known to initiate and maintain the senescence associated secretory phenotype via upregulating inflammatory mediators and reactive oxidative species (Salminen et al. 2012; Childs et al. 2015).
In addition, p21 protein content was associated with eNOS Ser1177 phosphorylation. This finding is also in contrast to previous data surrounding the role of senescence in ECs. In vitro data from human aortic ECs showed that senescence reduced eNOS protein content and activity (Matsushita et al. 2001). However, the positive association may provide a link between elevated expression of senescence markers and improved endothelium-dependent dilation, given that eNOS Ser1177 phosphorylation was also positively associated with endothelium-dependent dilation. The apparent disconnect between in vitro and in vivo data stresses the need for future human studies to evaluate the role of senescence at different stages of CAD development.
Associations between inflammation (NFKB), oxidative stress (NOX2) and vasoconstrictor (ET-1)
NFκB is a key transcription factor in the regulation of pro-inflammatory markers (Kempe et al. 2005). Endothelial expression NFκB had a positive correlation with NOX2 protein content. This association suggests that NFκB may be an important link between inflammation and oxidative stress (Donato et al. 2009; Marchio et al. 2019). Indeed, previous work demonstrates the potential for NAD(P)H oxidase-dependent induction of NFκB (Clark and Valente 2004). In support of this, NFκB inhibition reduced NOX2 expression and improved endothelium-dependent dilation in obese subjects (Pierce et al. 2009). This suggests a vicious cycle between inflammation and oxidative stress.
The expression of the potent vasoconstrictor ET-1 had a strong positive correlation with NFκB expression. ET-1 has been proposed to affect endothelial function via inflammatory pathways (Bohm and Pernow 2007; Bohm et al. 2007). Cardiac overexpression of ET-1 in mice is associated with increased activation of NFκB (Yang et al. 2004). In turn, NFκB stimulates ET-1 expression (Bohm and Pernow 2007; Virdis and Schiffrin 2003). As such, our data further highlight the critical role of NFκB as a key regulator in the development of endothelial dysfunction in CAD.
FMD does not predict arterial response to exercise
FMD was not correlated with the dilation induced during handgrip exercise. Exercise-induced dilation was also not associated with any of the atherogenic risk-modulating proteins assessed. Our team previously showed impaired FMD but preserved exercise-induced dilation in CAD patients following catheterization-induced damage (Tryfonos et al. 2020). This suggests different mechanisms may be responsible for dilation in these two tests. FMD is determined by a large and transient increase in shear stress. This is opposed to a more gradual increase in shear stress observed during exercise (Tremblay and Pyke 2018). FMD response is also known to be endothelium-dependent and mediated to a large extent though endothelial NO production (Green et al. 2014). In contrast, regulation of blood flow during exercise is a more complex process that involves a number of mechanisms (e.g., transmural pressure and vasoactive compounds) with multiple interactions and redundancy (Hellsten et al. 2012; Schrage et al. 2004, 2007; Green et al. 2017; Padilla et al. 2006). We believe the lack of association between FMD and exercise response in CAD patients add weight to the argument of different mechanisms underlined among these physiological responses.
A limitation of this study is that vascular measurements were taken on the day of catheterization. As such, although guidelines for FMD were followed (Thijssen et al. 2019), patients continued their medications as instructed by their consultant. Such medications could have affected the in vivo assessments of vascular function but are unlikely to affect the protein expression of ECs. Previous studies in CAD patients suggest that our radial FMD data are within the normal range (Dawson et al. 2010, 2012). Handgrip exercise was conducted 10 min after FMD assessment. To our knowledge, the influence of prior FMD assessment on response to handgrip exercise has not been established. Therefore, it is possible that the response to the handgrip exercise was influenced by the earlier hyperaemic stimulus. However, previous work has shown that FMD response was not influenced by earlier FMD assessment when the vessel was allowed to rest for ~ 5 min (Barton et al. 2011). Finally, the current study only measured total EC expression of NFκB p65. Given that translocation of NFκB to the nucleus is required to exert its actions on gene transcription, future work should expand this preliminary assessment and investigate nuclear abundance of NFκB p65 (Donato et al. 2008).
Summary and conclusions
The results of this study provide new insight into the molecular events underlying the continued development of endothelial dysfunction in patients with established CAD. In contrast to our hypothesis, we demonstrated that FMD in patients with established CAD was positively associated with markers of NO production (eNOS Ser1177 phosphorylation). Again, contrary to our hypothesis, FMD was not associated with markers of oxidative stress and inflammation (nitrotyrosine abundance and protein content of NOX2, NFκB and ET-1). Comparing to previous studies, our data suggest that there is a difference in the regulation of endothelium-dependent vasodilation between patients with established CAD and those without a clinical diagnosis. Our data in the isolated ECs suggest that patients with established CAD manage to maintain vasodilation by activating eNOS at Ser1177 residue. Given the association between senescence markers and FMD, future work should examine the role of senescence in the progression of CAD.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- BP:
-
Blood pressure
- CAD:
-
Coronary artery disease
- CVD:
-
Cardiovascular disease
- EC(s):
-
Endothelial cell(s)
- eNOS:
-
Endothelial nitric oxide synthase
- ET-1:
-
Endothelin 1
- FMD:
-
Flow-mediated dilation
- HE:
-
Handgrip exercise
- HR:
-
Heart rate
- HUVEC:
-
Human umbilical vein endothelial cell
- LHCH:
-
Liverpool Heart and Chest Hospital
- MVC:
-
Maximal voluntary contraction
- NFκB:
-
Nuclear factor kappa-light-chain-enhancer of activated B cell
- NO:
-
Nitric oxide
- NOX-2:
-
NADPH oxidase subunit NOX2
- NT:
-
Nitrotyrosine
- PCI:
-
Percutaneous coronary intervention
- peNOS Ser 1177:
-
Phospo-eNOS Ser1177
- PTCA:
-
Percutaneous transluminal coronary angiography
- p16:
-
Cyclin-dependent kinase inhibitor 2A
- p21:
-
Cyclin-dependent kinase inhibitor 1
- p53:
-
Tumor suppressor p53
- VE-cadherin:
-
Vascular endothelial cadherin
References
Aikawa K, Saitoh S, Muto M, Osugi T, Matsumoto K, Onogi F, Maehara K, Yaoita H, Maruyama Y (2004) Effects of antioxidants on coronary microvascular spasm induced by epicardial coronary artery endothelial injury in pigs. Coron Artery Dis 15(1):21–30
Barton M, Turner AT, Newens KJ, Williams CM, Thompson AK (2011) Minimum recovery time between reactive hyperemia stimulus in the repeated measurement of brachial flow-mediated dilatation. Ultrasound Med Biol 37(6):879–883. https://doi.org/10.1016/j.ultrasmedbio.2011.03.007
Bhayadia R, Schmidt BM, Melk A, Hömme M (2016) Senescence-induced oxidative stress causes endothelial dysfunction. J Gerontol A Biol Sci Med Sci 71(2):161–169. https://doi.org/10.1093/gerona/glv008
Bohm F, Pernow J (2007) The importance of endothelin-1 for vascular dysfunction in cardiovascular disease. Cardiovasc Res 76(1):8–18. https://doi.org/10.1016/j.cardiores.2007.06.004
Bohm F, Settergren M, Pernow J (2007) Vitamin C blocks vascular dysfunction and release of interleukin-6 induced by endothelin-1 in humans in vivo. Atherosclerosis 190(2):408–415. https://doi.org/10.1016/j.atherosclerosis.2006.02.018
Cai H, Harrison DG (2000) Endothelial dysfunction in cardiovascular diseases: the role of oxidant stress. Circ Res 87(10):840–844. https://doi.org/10.1161/01.res.87.10.840
Campisi J, d’Adda di Fagagna F (2007) Cellular senescence: when bad things happen to good cells. Nat Rev Mol Cell Biol 8(9):729–740. https://doi.org/10.1038/nrm2233
Casey DP, Ueda K, Wegman-Points L, Pierce GL (2017) Muscle contraction induced arterial shear stress increases endothelial nitric oxide synthase phosphorylation in humans. Am J Physiol Heart Circ Physiol 313(4):H854-h859. https://doi.org/10.1152/ajpheart.00282.2017
Cheetham C, Collis J, O’Driscoll G, Stanton K, Taylor R, Green D (2000) Losartan, an angiotensin type 1 receptor antagonist, improves endothelial function in non-insulin-dependent diabetes. J Am Coll Cardiol 36(5):1461–1466. https://doi.org/10.1016/s0735-1097(00)00933-5
Childs BG, Baker DJ, Wijshake T, Conover CA, Campisi J, van Deursen JM (2016) Senescent intimal foam cells are deleterious at all stages of atherosclerosis. Science 354(6311):472–477. https://doi.org/10.1126/science.aaf6659
Childs BG, Durik M, Baker DJ, van Deursen JM (2015) Cellular senescence in aging and age-related disease: from mechanisms to therapy. Nat Med 21(12):1424–1435. https://doi.org/10.1038/nm.4000
Childs BG, Gluscevic M, Baker DJ, Laberge RM, Marquess D, Dananberg J, van Deursen JM (2017) Senescent cells: an emerging target for diseases of ageing. Nat Rev Drug Discov 16(10):718–735. https://doi.org/10.1038/nrd.2017.116
Clark RA, Valente AJ (2004) Nuclear factor kappa B activation by NADPH oxidases. Mech Ageing Dev 125(10–11):799–810. https://doi.org/10.1016/j.mad.2004.08.009
Colombo PC, Ashton AW, Celaj S, Talreja A, Banchs JE, Dubois NB, Marinaccio M, Malla S, Lachmann J, Ware JA, Le Jemtel TH (2002) Biopsy coupled to quantitative immunofluorescence: a new method to study the human vascular endothelium. J Appl Physiol (1985) 92(3):1331–1338. https://doi.org/10.1152/japplphysiol.00680.2001
Cominacini L, Anselmi M, Garbin U, Fratta Pasini A, Stranieri C, Fusaro M, Nava C, Agostoni P, Keta D, Zardini P, Sawamura T, Lo Cascio V (2005) Enhanced plasma levels of oxidized low-density lipoprotein increase circulating nuclear factor-kappa B activation in patients with unstable angina. J Am Coll Cardiol 46(5):799–806. https://doi.org/10.1016/j.jacc.2005.05.063
Davignon J, Ganz P (2004) Role of endothelial dysfunction in atherosclerosis. Circulation. https://doi.org/10.1161/01.CIR.0000131515.03336.f8
Dawson EA, Alkarmi A, Thijssen DH, Rathore S, Marsman DE, Cable NT, Wright DJ, Green DJ (2012) Low-flow mediated constriction is endothelium-dependent: effects of exercise training after radial artery catheterization. Circ Cardiovasc Interv 5(5):713–719. https://doi.org/10.1161/circinterventions.112.971556
Dawson EA, Rathore S, Cable NT, Wright DJ, Morris JL, Green DJ (2010) Impact of introducer sheath coating on endothelial function in humans after transradial coronary procedures. Circ Cardiovasc Interv 3(2):148–156. https://doi.org/10.1161/circinterventions.109.912022
Donato AJ, Black AD, Jablonski KL, Gano LB, Seals DR (2008) Aging is associated with greater nuclear NF kappa B, reduced I kappa B alpha, and increased expression of proinflammatory cytokines in vascular endothelial cells of healthy humans. Aging Cell 7(6):805–812. https://doi.org/10.1111/j.1474-9726.2008.00438.x
Donato AJ, Eskurza I, Silver AE, Levy AS, Pierce GL, Gates PE, Seals DR (2007) Direct evidence of endothelial oxidative stress with aging in humans: relation to impaired endothelium-dependent dilation and upregulation of nuclear factor-kappaB. Circ Res 100(11):1659–1666. https://doi.org/10.1161/01.RES.0000269183.13937.e8
Donato AJ, Gano LB, Eskurza I, Silver AE, Gates PE, Jablonski K, Seals DR (2009) Vascular endothelial dysfunction with aging: endothelin-1 and endothelial nitric oxide synthase. Am J Physiol Heart Circ Physiol 297(1):H425-432. https://doi.org/10.1152/ajpheart.00689.2008
Donato AJ, Morgan RG, Walker AE, Lesniewski LA (2015) Cellular and molecular biology of aging endothelial cells. J Mol Cell Cardiol 89(Pt B):122–135. https://doi.org/10.1016/j.yjmcc.2015.01.021
Elahi MM, Kong YX, Matata BM (2009) Oxidative stress as a mediator of cardiovascular disease. Oxid Med Cell Longev 2(5):259–269. https://doi.org/10.4161/oxim.2.5.9441
Gates PE, Boucher ML, Silver AE, Monahan KD, Seals DR (2007) Impaired flow-mediated dilation with age is not explained by L-arginine bioavailability or endothelial asymmetric dimethylarginine protein expression. J Appl Physiol (1985) 102(1):63–71. https://doi.org/10.1152/japplphysiol.00660.2006
Green DJ, Dawson EA, Groenewoud HM, Jones H, Thijssen DH (2014) Is flow-mediated dilation nitric oxide mediated?: A meta-analysis. Hypertension 63(2):376–382. https://doi.org/10.1161/hypertensionaha.113.02044
Green DJ, Hopman MT, Padilla J, Laughlin MH, Thijssen DH (2017) Vascular adaptation to exercise in humans: role of hemodynamic stimuli. Physiol Rev 97(2):495–528. https://doi.org/10.1152/physrev.00014.2016
Guzik TJ, Mangalat D, Korbut R (2006) Adipocytokines - novel link between inflammation and vascular function? J Physiol Pharmacol 57(4):505–528
Hambrecht R, Adams V, Erbs S, Linke A, Krankel N, Shu Y, Baither Y, Gielen S, Thiele H, Gummert JF, Mohr FW, Schuler G (2003) Regular physical activity improves endothelial function in patients with coronary artery disease by increasing phosphorylation of endothelial nitric oxide synthase. Circulation 107(25):3152–3158. https://doi.org/10.1161/01.cir.0000074229.93804.5c
Hellsten Y, Nyberg M, Jensen LG, Mortensen SP (2012) Vasodilator interactions in skeletal muscle blood flow regulation. J Physiol 590(24):6297–6305. https://doi.org/10.1113/jphysiol.2012.240762
Hisamoto K, Ohmichi M, Kurachi H, Hayakawa J, Kanda Y, Nishio Y, Adachi K, Tasaka K, Miyoshi E, Fujiwara N, Taniguchi N, Murata Y (2001) Estrogen induces the Akt-dependent activation of endothelial nitric-oxide synthase in vascular endothelial cells. J Biol Chem 276(5):3459–3467. https://doi.org/10.1074/jbc.M005036200
Holder SM, Bruno RM, Shkredova DA, Dawson EA, Jones H, Hopkins ND, Hopman MTE, Bailey TG, Coombes JS, Askew CD, Naylor L, Maiorana A, Ghiadoni L, Thompson A, Green DJ, Thijssen DHJ (2021) Reference intervals for brachial artery flow-mediated dilation and the relation with cardiovascular risk factors. Hypertension 77(5):1469–1480. https://doi.org/10.1161/hypertensionaha.120.15754
Huang PL (2009) eNOS, metabolic syndrome and cardiovascular disease. Trends Endocrinol Metab 20(6):295–302. https://doi.org/10.1016/j.tem.2009.03.005
Katsuumi G, Shimizu I, Yoshida Y, Minamino T (2018) Vascular senescence in cardiovascular and metabolic diseases. Front Cardiovasc Med 5:18. https://doi.org/10.3389/fcvm.2018.00018
Kempe S, Kestler H, Lasar A, Wirth T (2005) NF-kappaB controls the global pro-inflammatory response in endothelial cells: evidence for the regulation of a pro-atherogenic program. Nucleic Acids Res 33(16):5308–5319. https://doi.org/10.1093/nar/gki836
Khanna AK (2009) Enhanced susceptibility of cyclin kinase inhibitor p21 knockout mice to high fat diet induced atherosclerosis. J Biomed Sci 16(1):66–66. https://doi.org/10.1186/1423-0127-16-66
Konukoglu D, Uzun H (2017) Endothelial Dysfunction and Hypertension. Adv Exp Med Biol 956:511–540. https://doi.org/10.1007/5584_2016_90
Kureishi Y, Luo Z, Shiojima I, Bialik A, Fulton D, Lefer DJ, Sessa WC, Walsh K (2000) The HMG-CoA reductase inhibitor simvastatin activates the protein kinase Akt and promotes angiogenesis in normocholesterolemic animals. Nat Med 6(9):1004–1010. https://doi.org/10.1038/79510
Lavi S, Yang EH, Prasad A, Mathew V, Barsness GW, Rihal CS, Lerman LO, Lerman A (2008) The interaction between coronary endothelial dysfunction, local oxidative stress, and endogenous nitric oxide in humans. Hypertension 51(1):127–133. https://doi.org/10.1161/hypertensionaha.107.099986
Lerman A, Edwards BS, Hallett JW, Heublein DM, Sandberg SM, Burnett JC Jr (1991) Circulating and tissue endothelin immunoreactivity in advanced atherosclerosis. N Engl J Med 325(14):997–1001. https://doi.org/10.1056/nejm199110033251404
Li H, Horke S, Förstermann U (2014) Vascular oxidative stress, nitric oxide and atherosclerosis. Atherosclerosis 237(1):208–219. https://doi.org/10.1016/j.atherosclerosis.2014.09.001
Manganaro A, Ciracì L, Andrè L, Trio O, Manganaro R, Saporito F, Oreto G, Andò G (2014) Endothelial dysfunction in patients with coronary artery disease: insights from a flow-mediated dilation study. Clin Appl Thromb Hemost 20(6):583–588. https://doi.org/10.1177/1076029614524620
Marchio P, Guerra-Ojeda S, Vila JM, Aldasoro M, Victor VM, Mauricio MD (2019) Targeting early atherosclerosis: a focus on oxidative stress and inflammation. Oxid Med Cell Longev 2019:8563845–8563845. https://doi.org/10.1155/2019/8563845
Matsushita H, Chang E, Glassford AJ, Cooke JP, Chiu CP, Tsao PS (2001) eNOS activity is reduced in senescent human endothelial cells: preservation by hTERT immortalization. Circ Res 89(9):793–798. https://doi.org/10.1161/hh2101.098443
Mercer J, Figg N, Stoneman V, Braganza D, Bennett MR (2005) Endogenous p53 protects vascular smooth muscle cells from apoptosis and reduces atherosclerosis in ApoE knockout mice. Circ Res 96(6):667–674. https://doi.org/10.1161/01.RES.0000161069.15577.ca
Minamino T, Miyauchi H, Yoshida T, Ishida Y, Yoshida H, Komuro I (2002) Endothelial cell senescence in human atherosclerosis: role of telomere in endothelial dysfunction. Circulation 105(13):1541–1544. https://doi.org/10.1161/01.cir.0000013836.85741.17
Minor RL, Myers PR, Guerra R, Bates JN, Harrison DG (1990) Diet-induced atherosclerosis increases the release of nitrogen oxides from rabbit aorta. J Clin Invest 86(6):2109–2116. https://www.jci.org/articles/view/114949
Mount PF, Kemp BE, Power DA (2007) Regulation of endothelial and myocardial NO synthesis by multi-site eNOS phosphorylation. J Mol Cell Cardiol 42(2):271–279. https://doi.org/10.1016/j.yjmcc.2006.05.023
Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, Das SR, de Ferranti S, Despres JP, Fullerton HJ, Howard VJ, Huffman MD, Isasi CR, Jimenez MC, Judd SE, Kissela BM, Lichtman JH, Lisabeth LD, Liu S, Mackey RH, Magid DJ, McGuire DK, Mohler ER 3rd, Moy CS, Muntner P, Mussolino ME, Nasir K, Neumar RW, Nichol G, Palaniappan L, Pandey DK, Reeves MJ, Rodriguez CJ, Rosamond W, Sorlie PD, Stein J, Towfighi A, Turan TN, Virani SS, Woo D, Yeh RW, Turner MB (2016) Executive summary: heart disease and stroke statistics–2016 update: a report from the American Heart Association. Circulation 133(4):447–454. https://doi.org/10.1161/cir.0000000000000366
Muñoz-Espín D, Serrano M (2014) Cellular senescence: from physiology to pathology. Nat Rev Mol Cell Biol 15(7):482–496. https://doi.org/10.1038/nrm3823
Nyberg M, Jensen LG, Thaning P, Hellsten Y, Mortensen SP (2012) Role of nitric oxide and prostanoids in the regulation of leg blood flow and blood pressure in humans with essential hypertension: effect of high-intensity aerobic training. J Physiol 590(6):1481–1494. https://doi.org/10.1113/jphysiol.2011.225136
O’Driscoll G, Green D, Maiorana A, Stanton K, Colreavy F, Taylor R (1999) Improvement in endothelial function by angiotensin-converting enzyme inhibition in non-insulin-dependent diabetes mellitus. J Am Coll Cardiol 33(6):1506–1511. https://doi.org/10.1016/s0735-1097(99)00065-0
O’Driscoll G, Green D, Rankin J, Stanton K, Taylor R (1997a) Improvement in endothelial function by angiotensin converting enzyme inhibition in insulin-dependent diabetes mellitus. J Clin Invest 100(3):678–684. https://doi.org/10.1172/jci119580
O’Driscoll G, Green D, Taylor RR (1997b) Simvastatin, an HMG-coenzyme A reductase inhibitor, improves endothelial function within 1 month. Circulation 95(5):1126–1131. https://doi.org/10.1161/01.cir.95.5.1126
Ohara Y, Peterson TE, Harrison DG (1993) Hypercholesterolemia increases endothelial superoxide anion production. J Clin Invest 91(6):2546–2551. https://doi.org/10.1172/jci116491
Oz F, Elitok A, Bilge AK, Mercanoglu F, Oflaz H (2012) Relationship between brachial artery flow-mediated dilation, carotid artery intima-media thickness and coronary flow reserve in patients with coronary artery disease. Cardiol Res 3(5):214–221. https://doi.org/10.4021/cr219w
Padilla J, Harris RA, Fly AD, Rink LD, Wallace JP (2006) The effect of acute exercise on endothelial function following a high-fat meal. Eur J Appl Physiol 98(3):256–262. https://doi.org/10.1007/s00421-006-0272-z
Pierce GL, Donato AJ, LaRocca TJ, Eskurza I, Silver AE, Seals DR (2011) Habitually exercising older men do not demonstrate age-associated vascular endothelial oxidative stress. Aging Cell 10(6):1032–1037. https://doi.org/10.1111/j.1474-9726.2011.00748.x
Pierce GL, Lesniewski LA, Lawson BR, Beske SD, Seals DR (2009) Nuclear factor-{kappa}B activation contributes to vascular endothelial dysfunction via oxidative stress in overweight/obese middle-aged and older humans. Circulation 119(9):1284–1292. https://doi.org/10.1161/circulationaha.108.804294
Real JT, Martínez-Hervás S, García-García AB, Civera M, Pallardó FV, Ascaso JF, Viña JR, Chaves FJ, Carmena R (2010) Circulating mononuclear cells nuclear factor-kappa B activity, plasma xanthine oxidase, and low grade inflammatory markers in adult patients with familial hypercholesterolaemia. Eur J Clin Invest 40(2):89–94. https://doi.org/10.1111/j.1365-2362.2009.02218.x
Ross R (1993) The pathogenesis of atherosclerosis: a perspective for the 1990s. Nature 362(6423):801–809. https://doi.org/10.1038/362801a0
Rossman MJ, Kaplon RE, Hill SD, McNamara MN, Santos-Parker JR, Pierce GL, Seals DR, Donato AJ (2017) Endothelial cell senescence with aging in healthy humans: prevention by habitual exercise and relation to vascular endothelial function. Am J Physiol Heart Circ Physiol 313(5):H890-h895. https://doi.org/10.1152/ajpheart.00416.2017
Salminen A, Kauppinen A, Kaarniranta K (2012) Emerging role of NF-κB signaling in the induction of senescence-associated secretory phenotype (SASP). Cell Signal 24(4):835–845. https://doi.org/10.1016/j.cellsig.2011.12.006
Schrage WG, Eisenach JH, Joyner MJ (2007) Ageing reduces nitric-oxide- and prostaglandin-mediated vasodilatation in exercising humans. J Physiol 579(Pt 1):227–236. https://doi.org/10.1113/jphysiol.2006.124313
Schrage WG, Joyner MJ, Dinenno FA (2004) Local inhibition of nitric oxide and prostaglandins independently reduces forearm exercise hyperaemia in humans. J Physiol 557(Pt 2):599–611. https://doi.org/10.1113/jphysiol.2004.061283
Seals DR, Jablonski KL, Donato AJ (2011) Aging and vascular endothelial function in humans. Clin Sci (lond) 120(9):357–375. https://doi.org/10.1042/cs20100476
Silver AE, Beske SD, Christou DD, Donato AJ, Moreau KL, Eskurza I, Gates PE, Seals DR (2007) Overweight and obese humans demonstrate increased vascular endothelial NAD(P)H oxidase-p47(phox) expression and evidence of endothelial oxidative stress. Circulation 115(5):627–637. https://doi.org/10.1161/circulationaha.106.657486
Thijssen DH, Black MA, Pyke KE, Padilla J, Atkinson G, Harris RA, Parker B, Widlansky ME, Tschakovsky ME, Green DJ (2011) Assessment of flow-mediated dilation in humans: a methodological and physiological guideline. Am J Physiol Heart Circ Physiol 300(1):H2-12. https://doi.org/10.1152/ajpheart.00471.2010
Thijssen DHJ, Bruno RM, van Mil A, Holder SM, Faita F, Greyling A, Zock PL, Taddei S, Deanfield JE, Luscher T, Green DJ, Ghiadoni L (2019) Expert consensus and evidence-based recommendations for the assessment of flow-mediated dilation in humans. Eur Heart J. https://doi.org/10.1093/eurheartj/ehz350
Thomas SR, Chen K, Keaney JF Jr (2002) Hydrogen peroxide activates endothelial nitric-oxide synthase through coordinated phosphorylation and dephosphorylation via a phosphoinositide 3-kinase-dependent signaling pathway. J Biol Chem 277(8):6017–6024. https://doi.org/10.1074/jbc.M109107200
Tremblay JC, Pyke KE (2018) Flow-mediated dilation stimulated by sustained increases in shear stress: a useful tool for assessing endothelial function in humans? Am J Physiol Heart Circ Physiol 314(3):H508–H520. https://doi.org/10.1152/ajpheart.00534.2017
Tryfonos A, Cocks M, Mills J, Green DJ, Dawson EA (2020) Exercise-induced vasodilation is not impaired following radial artery catheterization in coronary artery disease patients. J Appl Physiol (1985) 128(2):422–428. https://doi.org/10.1152/japplphysiol.00695.2019
Virdis A, Schiffrin EL (2003) Vascular inflammation: a role in vascular disease in hypertension? Curr Opin Nephrol Hypertens 12(2):181–187. https://doi.org/10.1097/00041552-200303000-00009
Woodman RJ, Playford DA, Watts GF, Cheetham C, Reed C, Taylor RR, Puddey IB, Beilin LJ, Burke V, Mori TA, Green D (2001) Improved analysis of brachial artery ultrasound using a novel edge-detection software system. J Appl Physiol (1985) 91(2):929–937. https://doi.org/10.1152/jappl.2001.91.2.929
Yang LL, Gros R, Kabir MG, Sadi A, Gotlieb AI, Husain M, Stewart DJ (2004) Conditional cardiac overexpression of endothelin-1 induces inflammation and dilated cardiomyopathy in mice. Circulation 109(2):255–261. https://doi.org/10.1161/01.Cir.0000105701.98663.D4
Acknowledgements
We thank Rafaella Rodighiero and James Shelley for help during the data collection, as well as the staff at the Liverpool Heart and Chest Hospital for support during the patient recruitment and data collection.
Funding
Prof. Green is funded by the National Health and Medical Research Council of Australia Principal Research Fellowship (1080914). Andrea Tryfonos was supported by a PhD scholarship from Liverpool John Moores University.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by AT, JM, ED, and MC. The first draft of the manuscript was written by AT and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Liverpool East NHS Research Ethics Committee (13/NW/0088).
Consent to participate
Informed consent was obtained from all individual patients included in the study.
Consent to publish
Patients signed informed consent regarding publishing of their data.
Additional information
Communicated by Fabio Fischetti.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Tryfonos, A., Mills, J., Green, D.J. et al. Association between atherogenic risk-modulating proteins and endothelium-dependent flow-mediated dilation in coronary artery disease patients. Eur J Appl Physiol 123, 367–380 (2023). https://doi.org/10.1007/s00421-022-05040-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00421-022-05040-z