Abstract
Background
Endothelial dysfunction may play a key role in non-obstructive coronary artery atherosclerosis. Our study aimed to evaluate the vascular endothelial function and its influencing factors in patients with non-obstructive coronary artery atherosclerosis.
Methods
A total of 131 consecutive patients with non-obstructive coronary artery atherosclerosis were enrolled. Flow-mediated dilatation (FMD) was measured at baseline and 1-year follow-up. Endothelial progenitor cells (EPCs) were counted by staining the fasting venous blood with antibodies against CD34 and vascular endothelial growth factor receptor 2.
Results
Systolic blood pressure, pulse pressure and the levels of HbA1c in participants with baseline FMD < 6% (n = 65) were significantly higher than those with baseline FMD ≥ 6% (n = 66). Baseline FMD was negatively associated with EPC counts (r = − 0.199, P < 0.05) and systolic blood pressure (r = − 0.315, P < 0.01). The 1-year FMD was significantly increased compared to the baseline FMD [(9.31 ± 5.62) % vs (7.31 ± 5.26) %, P < 0.001]. Independent predictors of FMD improvement included elevated EPC counts (OR = 1.104, 95% CI: 1.047–1.165, P < 0.001) and decreased levels of serum creatinine (OR = 0.915, 95% CI: 0.843–0.993, P = 0.034).
Conclusions
Family history of premature cardiovascular diseases, hypertension, elevated systolic pressure, and HbA1c > 6.5% are independent risk factors for endothelial dysfunction in non-obstructive atherosclerotic patients. Elevated peripheral blood EPC counts and decreased levels of serum creatinine are independent predictors of endothelial function improvement.
Similar content being viewed by others
Introduction
Non-obstructive coronary artery atherosclerosis is characterized by coronary artery stenosis less than 50% [1,2,3]. Vascular endothelial dysfunction, plaque rupture and thrombosis may be the main pathologic mechanism of acute or chronic myocardial ischemia [4, 5]. The vascular endothelium is a multifunctional organ that maintains vascular homeostasis, regulates cell proliferation and angiogenesis and preserves a non-thrombogenic blood-tissue interface. Endothelium dysfunction may play a key role in non-obstructive coronary artery atherosclerosis [6, 7]. Previous studies suggested that impaired endothelial function may be reversed by medicine treatment and lifestyle changes [8, 9].
Endothelial function can be directly evaluated by measuring the changes of arterial diameter in response to vasoactive drugs like nitric oxide that is directly injected into the coronary artery or the brachial artery [10,11,12]. However, this method is poorly accepted due to its invasiveness and high cost. On the contrary, flow-mediated dilatation (FMD) [13,14,15] and vascular reactive hyperemia index are noninvasive methods for evaluating endothelial function. They both use the principle of endothelium-dependent vessel diastolic function [16].
It has been shown that high-sensitivity C-reactive protein levels and neutrophil-to-lymphocyte ratio are significantly associated with vascular endothelial dysfunction [17, 18]. Endothelial cells can be regenerated by bone marrow-derived circulating endothelial progenitor cells (EPCs), which accelerates endothelialization and prevents atherosclerosis [19, 20]. Elevated EPC counts are thought to represent the ability of endothelial repair and atherosclerosis inhibition [21].
Our study aimed to investigate the influencing factors of vascular endothelial function in patients with non-obstructive coronary artery atherosclerosis.
Methods
Participants
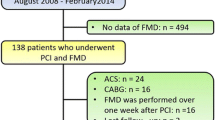
The prospective observation study included 131 consecutive patients with non-obstructive coronary artery atherosclerosis with atypical symptoms and/or non-specific electrocardiogram changes at the Xuanwu Hospital of Capital Medical University. Non-obstructive coronary atherosclerosis was diagnosed using angiography as the absence of obstructive coronary artery disease, i.e. no coronary artery stenosis ≥50% in any coronary artery. This includes patients with normal coronary arteries (no stenosis to stenosis < 30%) or mild coronary atheromatosis (stenosis of 30 to 50%) [PMID: 28158518]. The study was carried out from August 2013 to August 2015. All patients underwent coronary angiography or coronary computed tomographic angiography and had been conformed with coronary stenosis < 50%.
Patients with the following conditions were excluded: (1) coronary artery stenosis > 50% shown by imaging, or previous history of coronary artery interventional therapy or coronary artery bypass graft; (2) previous positive treadmill test, or transient elevation of ST-segment; (3) previous imaging suggesting myocardial ischemia; (4) previous tests showing levels of troponin I, troponin T, or creatine kinase-MB exceeding the upper limits of normal ranges; (5) patients with symptomatic heart failure, atrial fibrillation, cardiomyopathy or valvular diseases; (6) history of aortic dissection aneurysm, stroke or symptomatic peripheral artery diseases; (7) surgery, trauma or infection within 30 days; (8) renal or liver dysfunction; (9) secondary hypertension, hypertension emergency, or diabetes emergency; (10) rheumatic diseases, cancers, thyroid dysfunction, severe anemia, or use of glucocorticoid; (11) the informed consents were not signed.
Data collection and follow-up
Patient general information such as gender, age, smoking, height and weight were collected. The family history of premature cardiovascular disease was defined as having a first-degree male relative aged < 55 years and/or a first-degree female relative aged < 65 years.
Blood pressure was measured using a mercury sphygmomanometer for three times with intervals of 2 min [22]. The mean blood pressure and the pulse pressure were calculated. Fasting blood was drawn from the median cubital vein in the morning. Blood routine was performed by a hematology analyzer (Sysmex XE-2100). Serum levels of glycated hemoglobin (HbA1c), homocysteine and high-sensitivity C-reactive protein were measured by a biochemical analyzer (HITACHI 7600). To exclude myocardial injury/infarction, levels of cardiac troponin I were measured by a triage quantitative myocardial infarction/heart failure diagnostic device (Biosite, USA).
Patients were followed 1 year ±30 days later from the time of enrollment. The following events during the year were registered: myocardial infarction, percutaneous coronary intervention, coronary artery bypass grafting, heart failure, angina, hospitalization related to cardiovascular diseases, stroke (ischemic and/or hemorrhagic), transient ischemia attack, cardiac death and all-cause death.
Evaluation of vascular endothelial function
Vascular endothelial function was evaluated using the flow-mediated dilatation (FMD) on the day after admission and on the morning of follow-up visit [23]. Participants were required to fasted for 8 h and to avoided exercising, smoking, drinking, coffee, tea, and high-fat food (at least 12 h). Medicines that contain vasoactive agents were stopped for at least 24 h. The evaluation was performed by one investigator blinded to the study design in a quiet room after rest for 20 min. Color Doppler ultrasonography of the brachial artery was performed using a L12–3 transducer (10–13 MHz, Philips IE33). Electrocardiogram was recorded synchronously. FMD was calculated using the following formula: FMD = (D1 - D0) / D0 × 100%. D1 was the inner diameter of the brachial artery at the end of diastole. D0 was the basal inner diameter of the brachial artery. FMD < 6% was considered abnormal [24]. ΔFMD was calculated using the formula: ΔFMD = (1-year FMD - baseline FMD) / baseline FMD × 100%.
EPC counting
EPCs in the whole blood were identified and counted by detecting the expression of CD34 and vascular endothelial growth factor receptor 2 (VEGFR2) using flow cytometry (BD Biosciences, USA) [25,26,27]. The data were processed by the BD FACS Diva software (BD Biosciences, USA).
Statistical analysis
Data normality was examined using the Kolmogorov-Smirnov test. Quantitative variables with a normal distribution were presented as means ± standard deviations. Variables with a skewed distribution were presented as medians (interquartile ranges). Categorical variables were shown as numbers and percentage values.
One-way analysis of variance test or Kruskal-Wallis test was used to compare the continuous variables. Chi-square test or Fisher’s exact test was used for comparing the categorical variables. Spearman or Pearson correlation coefficient was used to represent the relationships between the variables.
Multivariate logistic regression was used to analyze the influencing factors of FMD. The dependent variable was FMD, and the independent variables were age > 65, male gender, smoking, hypertension, family history of premature cardiovascular diseases, HbA1c ≥ 6.5%, total cholesterol, low-density lipoprotein cholesterol, systolic blood pressure, pulse pressure and EPC count.
Differences were considered statistically significant if the two-sided P < 0.05. All analyses were performed with SPSS statistical software version 19.0 (SPSS, Chicago, IL).
Results
Our study included 131 consecutive patients with non-obstructive coronary artery atherosclerosis (Tables 1). The male to female ratio was 1:1.11. FMD was (7.31 ± 5.26) % at baseline. FMD ≥ 6% was considered to suggest a normal endothelial function. The general information and laboratory results were compared between patients with FMD < 6% and those with FMD ≥ 6% (Table 2). No significant difference in inflammatory biomarkers and CD34 + VEGFR2+ EPC counts was found between patients with FMD < 6% and those with FMD ≥ 6% (Table 2).
The mean EPC count was 43 cells per 106 cells. Heart rate, systolic blood pressure and pulse pressure in patients with EPC counts < 43 cells per 106 cells were significantly lower than that in those with EPC counts ≥43 cells per 106 cells. FMD in patients with lower EPC counts was significantly higher than that in those with higher EPC counts (Table 3). There was no significant difference in inflammatory factors between patients with lower EPC counts and those with higher EPC counts (Table 3). Pearson correlation analysis showed that EPC count was negatively associated with FMD (r = − 0.199, P < 0.05), and that FMD was negatively associated with systolic blood pressure (r = − 0.315, P < 0.01). However, no significant correlation was noticed between EPC count and systolic blood pressure/heart rate/white blood cell count, FMD and heart rate/white blood cell count, and systolic blood pressure and heart rate/white blood cell count.
Multivariate logistic regression showed that hypertension (odds ratio [OR] = 24.335, 95% confidence interval [CI]: 2.467–240.048), family history of premature cardiovascular (OR = 0.068, 95% CI 0.006–0.720), HbA1c ≥ 6.5% (OR = 0.059, 95% CI 0.007–0.485) and elevated systolic blood pressure (OR = 0.902, 95% CI: 0.821–0.990) were independently related to FMD decline at 1-year follow-up (Table 4).
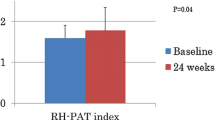
Five participants were lost to follow-up (3.82%). The 1-year FMD was significantly improved from the baseline [(9.31 ± 5.62) % vs (7.31 + 5.26) %, P < 0.001). The use of antiplatelet therapy, angiotensin-converting-enzyme inhibitor / angiotensin II receptor blockers, β-blockers and statins were significantly higher at 1-year follow-up than that at baseline (Table 5).
Participants with ΔFMD ≥10% had significantly higher proportions of hypertension, elevated systolic blood pressure, elevated pulse pressure and lower baseline FMD than those ΔFMD < 10%. Participants with ΔFMD < 10% had significantly more patients with diabetes and hypoglycemic therapy (biguanides, sulfonylureas, glinides and alpha-glucosidase inhibitors) than those with ΔFMD ≥10% (Table 6). EPC counts in participants with ΔFMD ≥10% was significantly higher than those with ΔFMD < 10% (59.14 ± 24.36 per 106 cells vs 36.11 ± 15.16 per 106 cells) at baseline (Table 6).
Multivariate logistic regression analysis showed that elevated EPC counts (OR = 1.104, 95% CI: 1.047–1.165) and decreased levels of serum creatinine (OR = 0.915, 95% CI: 0.843–0.993) were independently associated with FMD improvement at 1-year follow-up (Table 7).
Discussion
Increased blood flow-associated shear stress in hypertensive patients can significantly affect endothelial permeability [28, 29]. Our study found that systolic blood pressure and pulse pressure were significantly higher in the participants with FMD < 6% than those with FMD ≥ 6%. We also found that hypertension, systolic blood pressure and pulse pressure were independent risk factors in predicting endothelial dysfunction. It has been suggested that oxidative stress and endothelial dysfunction are associated with impaired vasodilatory capacity, which leads to hypertension [PMID: 28035582, 25,136,585, 27,203,578]. In addition, endothelial dysfunction is also associated with increased pulse pressure and hypertension in type 1 diabetes [PMID: 29101422].
Our study included 30 participants with diabetes and found elevated HbA1c levels were an independent influencing factor of endothelial dysfunction, suggesting diabetes may be associated with endothelial dysfunction. Hyperglycemia in diabetes is associated with inflammation and oxidative stress, which can result in endothelial dysfunction [PMID: 26781070, 30,274,207].
It has been shown that the phenotypic EPCs are independently associated with the severity of coronary artery lesion and carotid intima-media thickness and can be used as an independent predictor of cardiovascular outcomes [30, 31]. Our study found that the CD34 + VEGFR2+ EPC count was associated with the baseline FMD. Heart rate, systolic blood pressure and pulse pressure in participants with higher EPC counts were significantly higher than that in those with lower EPC counts. These results suggest that elevated systolic blood pressure and pulse pressure were more likely to be associated with differentiation and release of bone marrow-derived EPCs into the blood in comparison with to other risk factors of endothelial dysfunction. However, multivariate logistic regression analysis did not find independent association between EPC counts and baseline FMD.
A previous study found that high-sensitivity C-reactive protein was an independent risk factor for coronary heart disease and its level was significantly associated with the risk of future cardiovascular events, such as sudden death, acute myocardial infarction, and peripheral vascular disease [32, 33]. Another study showed that neutrophil-to-lymphocyte ratio was significantly associated with urinary albumin-to-creatinine ratio in asymptomatic stable coronary heart disease populations and was an independent predictor of systemic endothelial dysfunction [34, 35]. Neutrophil-to-lymphocyte ratio was independently associated to endothelial dysfunction and could predict composite cardiovascular endpoints [36, 37]. However, our study found that high-sensitivity C-reactive protein, white blood cell count and neutrophil-to-lymphocyte ratio were not significantly associated with FMD, suggesting that these inflammatory factors have no definite diagnostic value in low-risk patients with non-obstructive coronary atherosclerosis.
All our participants received intensive blood-pressure control, antiplatelet and statins therapy. No major cardiovascular events occurred during the 1-year follow-up. We found participants with worse baseline endothelial function had greater increase in 1-year FMD. Our study suggests that patients with hypertension, elevated systolic blood pressure and elevated pulse pressure at baseline are more likely to benefit from antihypertensive treatment. It has been shown that aliskiren, a direct renin inhibitor, can improve endothelial function and arterial stiffness when being used as an antihypertensive agent [PMID: 24994608, 24,708,382]. Another study showed that bisoprolol improved endothelial function in patients with hypertension and stable angina [PMID: 23609363]. Further research is needed to illustrate the detailed mechanisms between antihypertensive treatment and endothelial dysfunction.
In our study, participants with diabetes and elevated HbA1c did not show FMD improvements despite the same antihypertensive, antiplatelet and antihyperlipidemic treatments with the non-diabetic participants. We speculate the conventional antidiabetic medications have limited protective effect for vascular endothelial function. Diabetes can induce endothelial dysfunction, leading to increased risks of cardiovascular diseases [PMID: 28044409]. In addition, hyperglycemia is associated with EPCs dysfunction and endothelial dysfunction [PMID: 28718318]. Dapagliflozin is used to treated type 2 diabetes and showed improvements in endothelial function and arterial stiffness [PMID: 29061124]. New antidiabetic drugs, such as dipeptidyl peptidase-4 inhibitors, sodium-glucose cotransporter-2 inhibitors and glucagon-like peptide-1 receptor agonists also showed differentia effect on endothelial function and arterial stiffness [PMID: 30622967].
Chronic kidney disease and cardiovascular disease share similar risk factors. It has been shown that vascular endothelial function and FMD decreased significantly in patients with end-stage renal disease [38, 39]. Similarly, our study found that elevated levels of serum creatinine were associated with continuous endothelial injury. We speculate that major cardiovascular risk factors such as hypertension, diabetes and renal dysfunction can aggravate atherosclerosis partly by impairing the endothelial function. Our findings suggest that vascular endothelial dysfunction induced by hypertension is can be improved with antihypertensive treatment, while that associated with diabetes and renal dysfunction is more difficult to reverse.
Our study has limitations. Our study excluded patients with non-obstructive coronary atherosclerosis who present with symptoms of typical myocardial ischemia and acute coronary syndrome, suggesting worse endothelial dysfunction. This may underestimate the incidence and severity of endothelial dysfunction in patients with early atherosclerosis. At the 1-year follow-up, blood pressure, low-density lipoprotein cholesterol and HbA1c were not included in the analysis, making it difficult to assess the effect of anti-atherosclerosis treatment on vascular endothelial function.
Conclusion
Family history of premature cardiovascular diseases, hypertension, elevated systolic pressure, and HbA1c > 6.5% are independent risk factors for endothelial dysfunction in non-obstructive atherosclerotic patients. Elevated circulating EPC counts and decreased levels of serum creatinine are independent predictors of endothelial function improvement. Our findings may help to facilitate the risk stratification of patients with mild coronary atherosclerosis, and to explore intervention methods to repair vascular endothelial function.
Availability of data and materials
The datasets used and/or analyzed during the current study will be available from the corresponding author on reasonable request.
Abbreviations
- EPCs:
-
Endothelial progenitor cells
- FMD:
-
Flow-mediated dilatation
- VEGFR2:
-
Vascular endothelial growth factor receptor 2
References
Pepine CJ, Ferdinand KC, Shaw LJ, Light-McGroary KA, Shah RU, Gulati M, Duvernoy C, Walsh MN, Bairey Merz CN, ACC CVD in women committee. Emergence of nonobstructive coronary artery disease: a Woman's problem and need for change in definition on angiography. J Am Coll Cardiol. 2015;66(17):1918–33.
Jespersen L, Hvelplund A, Abildstrøm SZ, Pedersen F, Galatius S, Madsen JK, Jørgensen E, Kelbæk H, Prescott E. Stable angina pectoris with no obstructive coronary artery disease is associated with increased risks of major adverse cardiovascular events. Eur Heart J. 2012;33:734–44. https://doi.org/10.1093/eurheartj/ehr331.
Bairey Merz CN, Pepine CJ, Walsh MN, Fleg JL. Ischemia and no obstructive coronary artery disease (INOCA): developing evidence-based therapies and research agenda for the next decade. Circ. 2017;135(11):1075–92.
Libby P, Ridker PM, Hansson GK. Progress and challenges in translating the biology of atherosclerosis. Nat. 2011;473(7347):317–25.
Godo S, Shimokawa H. Endothelial functions. Arterioscler Thromb Vasc Biol. 2017;37(9):e108–14.
Choi BJ, Prasad A, Gulati R, Best PJ, Lennon RJ, Barsness GW, Lerman LO, Lerman A. Coronary endothelial dysfunction in patients with early coronary artery disease is associated with the increase in intravascular lipid core plaque. Eur Heart J. 2013;34(27):2047–54.
Mayranpaa MI, Heikkila HM, Lindstedt KA, Walls AF, Kovanen PT. Desquamation of human coronary artery endothelium by human mast cell proteases: implications for plaque erosion. Coron Artery Dis. 2006;17(7):611–21.
Vita JA. Endothelial function. Circ. 2011;124(25):906–12.
Whyte JJ, Laughlin MH. The effects of acute and chronic exercise on the vasculature. Acta Physiologica (Oxford, England). 2010;199(4):441–50.
Tousoulis D, SimopoulouC PN, Oikonomou E, Hatzis G, Siasos G, Tsiamis E, Stefanadis C. endothelial dysfunction in conduit arteries and in microcirculation. Novel therapeutic approaches. Pharmacol Ther. 2014;144(3):253–67.
Flammer AJ, Lüscher TF. Three decades of endothelium research: from the detection of nitric oxide to the everyday implementation of endothelial function measurements in cardiovascular diseases. Swiss Med Wkly. 2010;140:w13122.
Feletou M, Vanhoutte PM. Endothelial dysfunction: a multifaceted disorder (the Wiggers award lecture). Am J Phys Heart Circ Phys. 2006;291(3):H985–1002.
DS SKE, Gooch VM, et al. Non-invasive detection of endothelial dysfunction in children and adults at risk of atherosclerosis. Lancet. 1992;340:1111–5 [PubMed: 1359209].
Corretti MC, Anderson TJ, Benjamin EJ, et al. Guidelines for the ultrasound assessment of endotheilal-dependent flow-mediated vasodilation of the brachial artery: a report of the international brachial artery reactivity task force. J Am Coll Cardiol. 2002;39:257–65.
Higashi Y. Assessment of endothelial function. History, methodological aspects, and clinical perspectives. Int Heart J. 2015;56(2):125–34.
Takayama T, Wada A, Tsutamoto T, Ohnishi M, Fujii M, Isono T, Horie M. Contribution of vascular NAD(P)H oxidase to endothelial dysfunction in heart failure and the therapeutic effects of HMG-CoA reductase inhibitor. Circ J. 2004;68:1067–75.
Flammer AJ, Anderson T, Celermajer DS, Creager MA, Deanfield J, Ganz P, Hamburg NM, Lüscher TF, Shechter M, Taddei S, Vita JA, Lerman A. The assessment of endothelial function: from research into clinical practice. Circ. 2012;126(6):753–67.
Ross R. Atherosclerosis-an inflammatory disease. N Engl J Med. 1999;340(2):115–26.
Suzuki R, Fukuda N, Katakawa M, Tsunemi A, Tahira Y, Matsumoto T, Ueno T, Soma M. Effects of an angiotensin II receptor blocker on the impaired function of endothelial progenitor cells in patients with essential hypertension. Am J Hypertens. 2014;27(5):695–701.
Morikawal S, Takabe W, Mataki C, Kanke T, Itoh T, Wada Y, Izumi A, Saito Y, Hamakubo T, Kodama T. The effect of statins on mRNA levels of genes related to inflammation, coagulation and vascular constriction in HUVEC. J Atheroscler Thromb. 2002;9:178–83.
Ohkita M, Sugii M, Ka Y, Mori T, Hayashi T, Takaoka M, Matsumura Y. Differential effects of different statins on endothelin-1 gene expression and endothelial NOS phosphorylation in porcine aortic endothelial cells. Exp Biol Med. 2006;231:772–6.
The Seventh Report of the Joint Committee on Prevention. Detection, evaluation, and treatment of high blood pressure: the JNC 7 report. JAMA. 2003 May 21;289:2560–72.
Thijssen DH, Black MA, Pyke KE, et al. Assessment of flow-mediated dilation in humans: a methodological and physiological guideline. Am J Physiol Heart Circ Physiol. 2011;300(1):H2–H12.
Swift DL, Irving BA, Brock DW, Davis CK, Barrett EJ, Gaesser GA, Weltman A. Heart rate recovery does not predict endothelial function in obese women. Obes Metab. 2007 Sep 1;3(3):101–5.
Fadini GP, Baesso I, Albiero M, Sartore S, Agostini C, Avogaro A. Technical notes on endothelial progenitor cells: ways to escape from the knowledge plateau. Atherosclerosis. 2008;197(2):496–503.
Hou L, Kim JJ, Woo YJ, Huang NF. Stem cell-based therapies to promote angiogenesis in ischemic cardiovascular disease. Am J Physiol Heart Circ Physiol. 2016;310(4):H455–65.
Williams PA, Silva EA. The role of synthetic extracellular matrices in endothelial progenitor cell homing for treatment of vascular disease. Ann Biomed Eng. 2015;43(10):2301–13.
Tarbell JM. Shear stress and the endothelial transport barrier. Cardiovasc Res. 2010;87(2):320–30.
LaMack JA, Himburg HA, Li XM, Friedman MH. Interaction of wall shear stress magnitude and gradient in the prediction of arterial macromolecular permeability. Ann Biomed Eng. 2005;33(4):457–64.
Kunz GA, Ge L, Cuculi F, Gregg D, Vata KC, Shaw LK, Goldschmidt-Clermont PJ, Dong C, Taylor DA, Peterson ED. Circulating endothelial progenitor cells predict coronary artery disease severity. Am Heart J. 2006;152(1):190–5.
Keymel S, Kalka C, Rassaf T, Yeghiazarians Y, Kelm M, Heiss C. Impaired endothelial progenitor cell function predicts age-dependent carotid intimal thickening. Basic Res Cardiol. 2008;103(6):582–6.
Danesh J, Whincup P, Walker M, Lennon L, Thomson A, Appleby P, Gallimore JR, Pepys MB. Low grade inflammation and coronary heart disease: prospective study and updated meta-analyses. BMJ. 2000;321(7255):199–204.
Kuvin JT, Patel AR, Sliney KA, Pandian NG, Rand WM, Udelson JE, Karas RH. Peripheral vascular endothelial function testing as a noninvasive indicator of coronary artery disease. J Am Coll Cardiol. 2001;38(7):1843–9.
Martínez-Urbistondo D, Beltrán A, Beloqui O, Huerta A. The neutrophil-to-lymphocyte ratio as a marker of systemic endothelial dysfunction in asymptomatic subjects. Nefrol. 2016;36(4):397–403.
Kuvin JT, Patel AR, Sliney KA, Pandian NG, Sheffy J, Schnall RP, Karas RH, Udelson JE. Assessment of peripheral vascular endothelial function with finger arterial pulse wave amplitude. Am Heart J. 2003;146(1):168–74.
Solak Y, Yilmaz MI, Sonmez A, Saglam M, Cakir E, Unal HU, Gok M, Caglar K, Oguz Y, Yenicesu M, Karaman M, Ay SA, Gaipov A, Turk S, Vural A, Carrero JJ. Neutrophil to lymphocyte ratio independently predicts cardiovascular events in patients with chronic kidney disease. Clin Exp Nephrol. 2013 Aug;17(4):532–40.
Shechter M, Shechter A, Koren-Morag N, Feinberg MS, Hiersch L. Usefulness of brachial artery flow-mediated dilation to predict long-term cardiovascular events in subjects without heart disease. Am J Cardiol. 2014;113(1):162–7.
Chen J, Hamm LL, Mohler ER, Hudaihed A, Arora R, Chen C-S, Liu Y, Browne G, Mills KT, Kleinpeter MA, Simon EE, Rifai N, Klag MJ, He J. Interrelationship of multiple endothelial dysfunction biomarkers with chronic kidney disease. PLoS One. 2015;10(7):e0132047.
Asahara T, Murohara T, Sullivan A, Silver M, van der Zee R, Li T, Witzenbichler B, Schatteman G, Isner JM. Isolation of putative progenitor endothelial cells for angiogenesis. Sci. 1997;275(5302):964–7.
Acknowledgements
Not applicable.
Funding
This study was supported by National Natural Science Foundation of China (No.81470491). The funders had no role in the designing and conducting of this study and collection, analysis, and interpretation of data and in writing the manuscript.
Author information
Authors and Affiliations
Contributions
YPL, ZXF, QH and JL contributed to the design of the study. YPL, ZXF, JG, XPS, GHZ and YHZ dealt with patients’ follow up and contributed to the analysis, while YPL, ZXF, JG, JS, XBZ and ZL contributed to the interpretation of data. YPL and ZXF drafted the manuscript. All the authors critically revised the manuscript and gave final approval, and agree to be accountable for all aspects of the work, ensuring both its integrity and accuracy. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Our study was approved by the ethics committee of the Xuanwu Hospital of Capital Medical University. All participants have signed the informed consents.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no cmpeting interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Li, YP., Fan, ZX., Gao, J. et al. Influencing factors of vascular endothelial function in patients with non-obstructive coronary atherosclerosis: a 1-year observational study. BMC Cardiovasc Disord 20, 40 (2020). https://doi.org/10.1186/s12872-020-01326-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12872-020-01326-2