Abstract
Purpose
Women tend to have smaller lungs than men of the same size as well as narrower airways compared to men when matched for the same lung size. Additionally, women with smaller airways relative to lung size are more likely to experience expiratory flow limitation (EFL) as well as exercise-induced arterial hypoxemia (EIAH). One of the possible causes of EIAH includes excessive widening in the alveolar-to-arterial oxygen pressure difference (A-aDO2) due to diffusion limitation. This study investigated if lung diffusing capacity (D LCO) is lower in women with EFL compared to non-flow limited (NEFL) women during exercise.
Methods
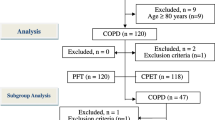
D LCO was measured using the rebreathing technique at rest and at 40, 60, and 80 % of \(\dot{V}{\text{O}}_{2\text{max}}\) on a treadmill in healthy women with EFL (n = 7; 21.6 ± 2.3) and without EFL (NEFL, n = 9; 21.2 ± 2.3). Arterial oxygen saturation was measured using pulse oximetry (SpO2).
Results
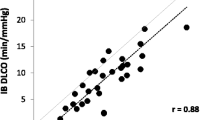
There was no difference (p > 0.05) in D LCO between groups at rest or during exercise; however, SpO2 was significantly lower in the EFL females compared to NEFL females during exercise.
Conclusion
Due to the lack of differences in D LCO between women with EFL and without EFL, our results suggest that this is not a possible cause for the significant differences in SpO2 between the two groups.


Similar content being viewed by others
Abbreviations
- A-aDO2 :
-
Alveolar-arterial oxygen difference
- ANOVA:
-
Analysis of variance
- CO:
-
Carbon monoxide
- C18O:
-
Carbon monoxide isotope 18
- D LCO :
-
Lung diffusing capacity of carbon monoxide
- EIAH:
-
Exercise-induced arterial hypoxemia
- EFL:
-
Expiratory flow limitation
- FEF50 %:
-
Forced expiratory flow rate at 50 % of lung volume
- FEV1.0 :
-
Forced expiratory volume in 1.0 s of FVC maneuver
- FV:
-
Flow volume
- FVC:
-
Forced vital capacity
- He:
-
Helium
- IC:
-
Inspiratory capacity
- MEFV:
-
Maximal expiratory flow-volume
- N2 :
-
Nitrogen
- NEFL:
-
Non-expiratory flow limited
- O2 :
-
Oxygen
- PaO2 :
-
Arterial partial pressure of oxygen
- Pst(L)50 :
-
Static lung recoil pressure at 50 % lung volume
- Q :
-
Cardiac output
- RPE:
-
Rate of perceived exertion
- SpO2 :
-
Pulse oxygen saturation
- VC :
-
Vital capacity
- V max50 :
-
Maximal flow rate at 50 % of lung volume
- \(\dot{V}{\text{O}}_{2\text{max}}\) :
-
Maximal rate of oxygen consumption per kilogram body weight
- W:
-
Watts
References
American Thoracic Society (1995) Standardization of Spirometry, 1994 Update. Am J Respir Crit Care Med 152:1107–1136
Babb TG (2013) Exercise ventilatory limitation: the role of expiratory flow limitation. Exerc Sport Sci Rev 41:11–18
Babb TG, Beck KC, Johnson BD (2012) Dysanapsis: importance of measured lung static recoil pressure. Med Sci Sports Exerc 44:1194; author reply 1195
Baldi JC, Cassuto NA, Foxx-Lupo WT, Wheatley CM, Snyder EM (2010) Glycemic status affects cardiopulmonary exercise response in athletes with type I diabetes. Med Sci Sports Exerc 42:1454–1459
Dempsey JA (1986) Wolffe memorial lecture: is the lung built for exercise? Med Sci Sports Exerc 16:143–155
Dempsey JA, Wagner PD (1999) Exercise-induced arterial hypoxemia. J Appl Physiol 87:1997–2006
Dempsey JA, McKenzie DC, Haverkamp HC, Eldridge MW (2008) Update in the understanding of respiratory limitations to exercise performance in fit, active adults. Chest 134:613–622
Derchak PA, Stager JM, Tanner DA, Chapman RF (2000) Expiratory flow limitation confounds ventilatory response during exercise in athletes. Med Sci Sports Exerc 32:1873–1879
Dominelli PB, Guenette JA, Wilkie SS, Foster GE, Sheel AW (2011) Determinants of expiratory flow limitation in healthy women during exercise. Med Sci Sport Exerc 43:1666–1674
Dominelli PB, Foster GE, Dominelli GS, Henderson WR, Koehle MS, McKenzie DC, Sheel AW (2013) Exercise-induced arterial hypoxaemia and the mechanics of breathing in healthy young women. J Physiol 591:3017–3034
Green M, Mead J, Turner JM (1974) Variability of maximum expiratory flow-volume curves. J Appl Physiol 37:67–74
Guenette JA, Witt JD, McKenzie DC, Road JD, Sheel AW (2007) Respiratory mechanics during exercise in endurance-trained men and women. J Physiol 581:1309–1322
Harms CA, McClaran SR, Nickele GA, Pegelow DF, Nelson WB, Dempsey JA (1998) Exercise-induced arterial hypoxaemia in healthy young women. J Physiol 507:619–628
Hopkins SR, Harms CA (2004) Gender and pulmonary gas exchange during exercise. Exerc Sports Sci Rev 32:50–56
Hsia CCW, McBrayer DG, Ramanathan M (1995) Reference values of pulmonary diffusing capacity during exercise by a rebreathing technique. Am J Respir Crit Care Med 152:658–665
Jensen RL, Crapo RO, Mason JD, Yanowitz FG (1990) Small-sample reproducibility estimates: an example using rebreathing measurements. J Appl Physiol 68:1717–1720
Johnson RL Jr (1967) Pulmonary diffusion as a limiting factor in exercise stress. Circ Res 20:154–160
Johnson BD, Reddan WG, Seow KC, Dempsey JA (1991) Mechanical constraints on exercise hypernea in a fit aging population. Am Rev Respir Dis 143:968–977
McClaran SR, Harms CA, Pegelow DF, Dempsey JA (1998) Smaller lungs in women affect exercise hyperpnea. J Appl Physiol 84:1872–1881
McKenzie DC (2012) Respiratory physiology: adaptations to high-level exercise. Br J Sports Med 46:381–384
Mead J (1980) Dysanapsis in normal lungs assessed by the relationship between maximal flow, static recoil, and vital capacity. Am Rev Respir Dis 121:339–342
Olafsson S, Hyatt RE (1969) Ventilatory mechanics and expiratory flow limitation during exercise in normal subjects. J Clin Investig 48:564–573
Pellegrino R, Brusasco V, Rodarte JR, Babb TG (1985) Expiratory flow limitation and regulation of end-expiratory lung volume during exercise. J Appl Physiol 74:2552–2558
Rose GL, Cassidy SS, Johnson RL Jr (1979) Diffusing capacity at different lung volumes during breath holding and rebreathing. J Appl Physiol 47:32–37
Roughton FJ, Forster RE (1957) Chemical reaction rates in determining rate of exchange of gases in the human lung, with special reference to true diffusing capacity of pulmonary membrane and volume of blood in the lung capillaries. J Appl Physiol 11:290–302
Saltin B, Calbet JA (2006) Point: in health and in a normoxic environment, \(\dot{V}{\text{O}}_{2\text{max}}\) is limited primarily by cardiac output and locomotor muscle blood flow. J Appl Physiol 100:744–745
Sheel AW, Guenette JA, Yuan R, Holy L, Mayo JR, McWilliams AM, Lam S, Coxson HO (2009) Evidence of dysanapsis using computed tomographic imaging of the airways in older ex-smokers. J Appl Physiol 107:1622–1628
Smith JR, Rosenkranz SK, Harms CA (2014) Dysanapsis ratio as a predictor for expiratory flow limitation. Respir Physiol Neurobiol 198:25–31
Triebwasser JH, Johnson RL Jr, Burpo RP, Campbell JC, Reardon WC, Blomqvist CG (1977) Noninvasive determination of cardiac output by a modified acetylene rebreathing procedure utilizing mass spectrometer measurements. Aviat Space Environ Med 48:203–209
Turner JM, Mead J, Wohl ME (1968) Elasticity of human lungs in relation to age. J Appl Physiol 25:664–671
Wheatley CM, Baldi JC, Cassuto NA, Foxx-Lupo WT, Snyder EM (2011) Glycemic control influences lung membrane diffusion and oxygen saturation in exercise-trained subjects with type 1 diabetes: alveolar-capillary membrane conductance in type 1 diabetes. Eur J Appl Physiol 111:567–578
Wilkie SS, Guenette JA, Dominelli PB, Sheel AW (2012) Effects of an aging pulmonary system on expiratory flow limitation and dyspnoea during exercise in healthy women. Eur J Appl Physiol 112:2195–2204
Author information
Authors and Affiliations
Corresponding author
Additional information
Communicated by David C. Poole.
Rights and permissions
About this article
Cite this article
Nordin, K.C., Lee, M.J., Harms, C.A. et al. Is lung diffusing capacity lower in expiratory flow limited women compared to non-flow limited women during exercise?. Eur J Appl Physiol 115, 755–761 (2015). https://doi.org/10.1007/s00421-014-3053-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00421-014-3053-0