Abstract
Understanding potential disease causation due to stenosis and thrombosis and its treatment by utilising catheters and magnetic field has gained increasing attention from experts worldwide. Endothelial injury or plaque rupture can trigger thrombosis, which can cut off the supply of blood to the heart or brain, causing stroke or a myocardial infarction. In the regions of stenosis, narrowing of lumen of arteries and high shear rate generate conditions that increase platelet build-up and blockage. Treatment like catheters and magnetic field are famously being implemented in modern medicine as a way of removing blood clots inside a constricted artery in light to improve the blood circulation inside a human body. This article reviews the impact of the simultaneous presence of stenosis and thrombosis on rheological properties of blood flow and the effects of using catheter in clearing the obstructions in the inner wall of blood vessel. We also introduce significant recent development on blood flow modelling relating to the subject matter. A sample mathematical model is considered from the literature to explain the influence of aforesaid arterial constrictions and clinical therapy for future directions in the medical field. Based on the collected literature, we note that the angioplasty catheter greatly increases blood flow as compared to infusion and guidewire catheters because it uses a balloon-tipped catheter to remove occlusions in the artery lumen. This comprehensive review and the proposed mathematical model together with the clinical data may offer directions for further studies, especially on one specific type of catheter for balloon angioplasty as the best treatment for clearing the occlusions in the diseased artery.














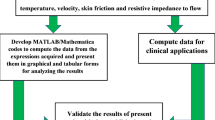
Adapted from Ref. [105]


Similar content being viewed by others
Abbreviations
- CAD:
-
Coronary artery diseases
- LDL:
-
Low-density lipoproteins
- SMCs:
-
Smooth muscle cells
- AP:
-
Activated platelets
- AF:
-
Atrial fibrillation
- TF:
-
Tissue factor
- PLS:
-
Plasminogens
- RBCs:
-
Red blood cells
- WBCs:
-
White blood cells
- ADP:
-
Adenine di-phosphate
- GpIb:
-
Glycoprotein Ib
- LMWH:
-
Low molecular weight heparin
- VADs:
-
Ventricular assist devices
- DVT:
-
Deep venous thrombosis
- PE:
-
Pulmonary thromboembolism
- ATIII:
-
Antithrombin III
- Rx:
-
Rapid exchange
- OTW:
-
Over-the-wire
- POBA:
-
Plain old balloon angioplasty
References
Thomas, B., Sumam, K.S.: Blood flow in human arterial system—a review. Procedia Technol. 24, 339–346 (2016). https://doi.org/10.1016/j.protcy.2016.05.045
Schlichting, H., Gersten, K.: Boundary-layer theory. McGraw-Hill Book Company, New York (1968)
Biswas, D.: Blood flow models: a comparative study. Mittal Publications, New Delhi (2000)
Ling, S.C., Atabek, H.B.: A nonlinear analysis of pulsatile flow in arteries. J. Fluid Mech. 55, 493–511 (1972)
Korakianitis, T., Shi, Y.: Numerical simulation of cardiovascular dynamics with healthy and diseased heart valves. J. Biomech. 39, 1964–1982 (2006). https://doi.org/10.1016/j.jbiomech.2005.06.016
Ku, D.N.: Blood flow in arteries. Annu. Rev. Fluid Mech. 29, 399–434 (1997). https://doi.org/10.1146/annurev.fluid.29.1.399
Stein, P.D., Sabbah, H.N.: Turbulent blood flow in the ascending aorta of humans with normal and diseased aortic valves. Circ. Res. 39, 58–65 (1976). https://doi.org/10.1161/01.RES.39.1.58
Chandran, K.B., Rittgers, S.E., Yoganathan, A.P.: The Human Circulation. Biofluid Mechanics. CRC Press, Hoboken (2012)
Mendis, S., Puska, P., Norrving, B., Organization, W.H., Federation, W.H., Organization, W.S.: Global atlas on cardiovascular disease prevention and control/edited by: Shanthi Mendis ... [et al.] https://apps.who.int/iris/handle/10665/44701 (2011)
Calvet, D., Touzé, E., Varenne, O., Sablayrolles, J.-L., Weber, S., Mas, J.-L.: Prevalence of asymptomatic coronary artery disease in ischemic stroke patients. Circulation 121, 1623–1629 (2010). https://doi.org/10.1161/CIRCULATIONAHA.109.906958
Ralapanawa, U., Sivakanesan, R.: Epidemiology and the magnitude of coronary artery disease and acute coronary syndrome: a narrative review. J. Epidemiol. Glob. Health. 11, 169–177 (2021). https://doi.org/10.2991/jegh.k.201217.001
Badimon, L., Padró, T., Vilahur, G.: Atherosclerosis, platelets and thrombosis in acute ischaemic heart disease. Eur. Hear. J. Acute Cardiovasc. Care 1, 60–74 (2012). https://doi.org/10.1177/2048872612441582
Mundi, S., Massaro, M., Scoditti, E., Carluccio, M.A., van Hinsbergh, V.W.M., Iruela-Arispe, M.L., De Caterina, R.: Endothelial permeability, LDL deposition, and cardiovascular risk factors-a review. Cardiovasc. Res. 114, 35–52 (2018). https://doi.org/10.1093/cvr/cvx226
Chen, J., Su, Y., Pi, S., Hu, B., Mao, L.: The dual role of low-density lipoprotein receptor-related protein 1 in atherosclerosis. Front. Cardiovasc. Med. 8, 682389 (2021). https://doi.org/10.3389/fcvm.2021.682389
Ross, R.: Atherosclerosis—an inflammatory disease. N. Engl. J. Med. 340, 115–126 (1999). https://doi.org/10.1056/NEJM199901143400207
Cassar, A., Holmes, D.R., Jr., Rihal, C.S., Gersh, B.J.: Chronic coronary artery disease: diagnosis and management. Mayo Clin. Proc. 84, 1130–1146 (2009). https://doi.org/10.4065/mcp.2009.0391
Young, D.F., Tsai, F.Y.: Flow characteristics in models of arterial stenosis—II Unsteady flow. J. Biomech. 6, 547–559 (1973). https://doi.org/10.1016/0021-9290(73)90012-2
Young, D.F., Tsai, F.Y.: Flow characteristics in models of arterial stenosis—I Steady flow. J. Biomech. (1973). https://doi.org/10.1016/0021-9290(73)90099-7
Back, L.D., Radbill, J.R., Cronfold, D.A.: Analysis of pulsatile viscous flow through diseased coronary arteries of man. J. Biomech. 10, 339–353 (1977)
Padmanabban, N.: Mathematical model of arterial stenosis. Med. Biol. Eng. Comput. 18, 281–286 (1980)
Mehrotra, R., Jayaraman, G., Padmanabhan, N.: Pulsatile blood flow in a stenosed artery—a theoretical model. Med. Biol. Eng. Comput. 23, 55–62 (1985). https://doi.org/10.1007/BF02444028
Mishra, J.C., Chakravorty, S.: Flow in arteries in the presence of stenosis. J. Biomech. 19, 1907–1918 (1986)
Mustapha, N., Mandal, P.K., Johnston, P.R., Amin, N.: A numerical simulation of unsteady blood flow through multi-irregular arterial stenoses. Appl. Math. Model. 34, 1559–1573 (2010). https://doi.org/10.1016/j.apm.2009.09.008
Chakravarty, S., Mandal, P.K.: Two-dimensional blood flow through tapered arteries under stenotic conditions. Int. J. Non-Linear Mech. 35, 779–793 (2000). https://doi.org/10.1016/S0020-7462(99)00059-1
Sankar, D.S., Ismail, A.: Two-fluid mathematical models for blood flow in Stenosed arteries: a comparative study. Bound. Value Probl. 2009, 568657 (2009). https://doi.org/10.1155/2009/568657
Sankar, D.S.: Two-fluid nonlinear mathematical model for pulsatile blood flow through stenosed arteries. Bull. Malays. Math. Sci. Soc. 35, 487–495 (2012)
Sankar, D.S., Jaafar, N.A.B., Yatim, Y.: Nonlinear analysis for shear augmented dispersion of solutes in blood flow through narrow arteries. J. Appl. Math. 2012, 812535 (2012). https://doi.org/10.1155/2012/812535
Gauthier, P.: Mathematics in Atmospheric Sciences: An Overview. Springer, Berlin (2009)
Ismail, Z., Abdullah, I., Mustapha, N., Norsarahaida, A.: A power-law model of blood flow through a tapered overlapping stenosed artery. Appl. Math. Comput. 195, 669–680 (2008). https://doi.org/10.1016/j.amc.2007.05.014
Afiqah, W.S., Sankar, D.S.: Effects of porosity in four-layered non-linear blood rheology in constricted narrow arteries with clinical applications. Comput. Methods Programs Biomed. 199, 105907 (2020). https://doi.org/10.1016/j.cmpb.2020.105907
Afiqah, W.S., Sankar, D.S.: Two-phase nonlinear rheological analysis of blood flow in small diameter blood vessels with constriction. ARPN J. Eng. Appl. Sci. 15, 1129–1143 (2020)
Sankar, D.S., Yatim, Y.: Comparative analysis of mathematical models for blood flow in tapered constricted arteries. Abstr. Appl. Anal. (2012). https://doi.org/10.1155/2012/235960
Sankar, D.S., Lee, U., Nagar, A.K., Morsidi, M.: Mathematical analysis of Carreau fluid model for blood flow in tapered constricted arteries. AIP Conf. Proc. 2016, 1–20 (2018). https://doi.org/10.1063/1.5055530
Pokhrel, P., Kafle, J., Kattel, P., Gaire, H.: Analysis of blood flow through artery with mild stenosis. J. Inst. Sci. Technol. 25, 33–38 (2020). https://doi.org/10.3126/jist.v25i2.33732
Manisha, Nasha, V., Kumar, S.: Non-Newtonian blood flow model with the effect of different geometry of stenosis. J. Math. Comput. Sci. (2022). https://doi.org/10.28919/jmcs/7104
Sarwar, L., Hussain, A.: Flow characteristics of Au-blood nanofluid in stenotic artery. Int. Commun. Heat Mass Transf. 127, 105486 (2021). https://doi.org/10.1016/j.icheatmasstransfer.2021.105486
Anand, M., Rajagopal, K., Rajagopal, K.R.: A model incorporating some of the mechanical and biochemical factors underlying clot formation and dissolution in flowing blood. J. Theor. Med. 5, 183–218 (2003). https://doi.org/10.1080/10273660412331317415
Alfeo, M., Pagotto, A., Barbieri, G., Foster, T., Vanhoorelbeke, K., De Filippis, V., Speziale, P., Pietrocola, G.: Staphylococcus aureus iron-regulated surface determinant B (IsdB) protein interacts with von Willebrand factor and promotes adherence to endothelial cells. Sci. Rep. (2021). https://doi.org/10.1038/s41598-021-02065-w
Lowe, G.D.: Rheological influences on thrombosis. Baillieres’s Clin. Haematol. 12, 435–449 (1999)
Sankar, D.S.: Perturbation analysis for pulsatile flow of Carreau fluid through tapered stenotic arteries. Int. J. Biomath. 09, 1650063 (2015). https://doi.org/10.1142/S1793524516500637
Palta, S., Saroa, R., Palta, A.: Overview of the coagulation system. Indian J. Anaesth. 58, 515–523 (2014). https://doi.org/10.4103/0019-5049.144643
Gimbrone, M.A.: Endothelial dysfunction, hemodynamic forces, and atherosclerosis. Thromb. Haemost. 82, 722–726 (1999)
Roka-Moiia, Y., Walk, R., Palomares, D.E., Ammann, K.R., Dimasi, A., Italiano, J.E., Sheriff, J., Bluestein, D., Slepian, M.J.: Platelet activation via shear stress exposure induces a differing pattern of biomarkers of activation versus biochemical agonists. Thromb. Haemost. 120, 776–792 (2020). https://doi.org/10.1055/s-0040-1709524
Macfarlane, R.G.: An enzyme cascade in the blood clotting mechanism, and its function as a biochemical amplifier. Nature 202, 498–499 (1964). https://doi.org/10.1038/202498a0
Chien, S., Usami, S., Taylor, H.M., Lundberg, J.L., Gregersen, M.I.: Effects of hematocrit and plasma proteins on human blood rheology at low shear rates. J. Appl. Physiol. 21, 81–87 (1966). https://doi.org/10.1152/jappl.1966.21.1.81
Evans, E.A., Hochmuth, R.M.: Membrane viscoelasticity. Biophys. J. 16, 1–11 (1976). https://doi.org/10.1016/S0006-3495(76)85658-5
Schmid-Schönbein, G.W., Sung, K.L., Tözeren, H., Skalak, R., Chien, S.: Passive mechanical properties of human leukocytes. Biophys. J. 36, 243–256 (1981). https://doi.org/10.1016/S0006-3495(81)84726-1
Thurston, G.B.: Viscoelasticity of human blood. Biophys. J. 12, 1205–1217 (1972). https://doi.org/10.1016/S0006-3495(72)86156-3
Chien, S., Usami, S., Dellenback, R.J., Gregersen, M.I.: Blood viscosity: influence of erythrocyte deformation. Science 157, 827–829 (1967). https://doi.org/10.1126/science.157.3790.827
Chien, S., Sung, K.L., Skalak, R., Usami, S., Tözeren, A.: Theoretical and experimental studies on viscoelastic properties of erythrocyte membrane. Biophys. J. 24, 463–487 (1978). https://doi.org/10.1016/S0006-3495(78)85395-8
Thurston, G.B.: Frequency and shear rate dependence of viscoelasticity of blood. Biorheology 10, 375–381 (1973)
Anand, M., Rajagopal, K.R.: A shear-thinning viscoelastic model for describing the flow of blood. Int. J. Cardiovasc. Med. Sci. 4, 59–68 (2004)
Lasslo, A.: Blood Platelet Function and Medicinal Chemistry. Elsevier Biomedical, New York (1984)
Ruggeri, Z.M., Dent, J.A., Saldivar, E.: Contribution of distinctive adhesive interactions to platelet aggregation in flowing blood. Blood 94, 172–178 (1999)
Frojmovic, M.M., Mooney, R.F., Wong, T.: Dynamics of platelet glycoprotein IIb-IIIa receptor expression and fibrinogen binding. I. Quantal activation of platelet subpopulations varies with adenosine diphosphate concentration. Biophys. J. 67, 2060–2068 (1994). https://doi.org/10.1016/S0006-3495(94)80689-7
Baumgartner, H.R.: The role of blood flow in platelet adhesion, fibrin deposition, and formation of mural thrombi. Microvasc. Res. 5, 167–179 (1973). https://doi.org/10.1016/0026-2862(73)90069-1
Affeld, K., Reininger, A.J., Gadischke, J., Grunert, K., Schmidt, S., Thiele, F.: Fluid mechanics of the stagnation point flow chamber and its platelet deposition. Artifical Organs. 19, 597–602 (1995)
Tschopp, T.B., Baumgartner, H.R., Silberbauer, K., Sinzinger, H.: Platelet adhesion and platelet thrombus formation on Subendothelium of human arteries and veins exposed to flowing blood in vitro. A comparison with Rabbit Aorta. Pathophysiol. Haemost. Thromb. 8, 19–29 (1979). https://doi.org/10.1159/000214287
Christodoulides, N., Feng, S.J., Resendic, J.C., Kroll, M.H.: Shear stress induces dynamic association of GpIbalpha with ABP and actin in human platelets. In: Thrombosis and Haemostasis (1999)
Wurzinger, L.J.: Histophysiology of the circulating platelet. In: Advances in anatomy, embryology and cell biology (1990)
Karsaj, I., Humphrey, J.D.: A mathematical model of evolving mechanical properties of intraluminal thrombus. Biorheology 46, 509–527 (2009). https://doi.org/10.3233/BIR-2009-0556
Tsapikouni, T., Missirlis, Y.: PH and ionic strength effect on single fibrinogen molecule adsorption on mica studied with AFM. Colloids Surf. B Biointerfaces 57, 89–96 (2007). https://doi.org/10.1016/j.colsurfb.2007.01.011
Gillespie, A.H., Doctor, A.: Red blood cell contribution to hemostasis. Front. Pediatr. 9, 1–9 (2021). https://doi.org/10.3389/fped.2021.629824
MacIntyre, C.R., Bui, C.M.: Pandemics, public health emergencies and antimicrobial resistance - putting the threat in an epidemiologic and risk analysis context. Arch. Public Heal. 75, 54 (2017). https://doi.org/10.1186/s13690-017-0223-7
Gillinov, A.M., McCarthy, P.M.: Curative surgery for atrial fibrillation: current status and minimally invasive approaches. Expert Rev. Cardiovasc. Ther. 1, 595–603 (2003). https://doi.org/10.1586/14779072.1.4.595
Melillo, E., Palmiero, G., Ferro, A., Mocavero, P.E., Monda, V., Ascione, L.: Diagnosis and Management of Left Atrium Appendage Thrombosis in Atrial Fibrillation Patients Undergoing Cardioversion. Medicina (Kaunas) 55, 511 (2019). https://doi.org/10.3390/medicina55090511
Hirsh, J.: Current anticoagulant therapy–unmet clinical needs. Thromb. Res. 109(Suppl), S1-8 (2003). https://doi.org/10.1016/s0049-3848(03)00250-0
Thachil, J.: Antiplatelet therapy—a summary for the general physicians. Clin. Med. 16, 152–160 (2016). https://doi.org/10.7861/clinmedicine.16-2-152
Ezekowitz, M.D., Netrebko, P.I.: Anticoagulation in management of atrial fibrillation. Curr. Opin. Cardiol. 18, 26–31 (2003). https://doi.org/10.1097/00001573-200301000-00004
Cox, J.L., Schuessler, R.B., D’Agostino, H.J., Stone, C.M., Chang, B.-C., Cain, M.E., Corr, P.B., Boineau, J.P.: The surgical treatment of atrial fibrillation: III. Development of a definitive surgical procedure. J. Thorac. Cardiovasc. Surg. 101, 569–583 (1991). https://doi.org/10.1016/S0022-5223(19)36684-X
Lampert, B.C., Dyke, D.B.S., Koelling, T.M.: Heart failure due to left ventricular systolic dysfunction BT - Practical Cardiology: Evaluation and Treatment of Common Cardiovascular Disorders. Presented at the (2020)
Jiang, Y.-X., Jing, L.-D., Jia, Y.-H.: Clinical characteristics and risk factors of left ventricular thrombus after acute myocardial infarction: a matched case-control study. Chin Med J (Engl) 128, 2415–2419 (2015). https://doi.org/10.4103/0366-6999.164869
Yavuzgil, O., Gürgün, C., Apaydin, A., Cinar, C., Kültürsay, H.: A giant inferoposterior true aneurysm of the left ventricle mimicking a pseudoaneurysm. Int. J. Cardiovasc. Imaging 22, 205–212 (2006). https://doi.org/10.1007/s10554-005-9013-3
Okuyan, E., Okcun, B., Dinçkal, M.H., Mutlu, H.: Risk factors for development of left ventricular thrombus after first acute anterior myocardial infarction-association with anticardiolipin antibodies. Thromb. J. 8, 15 (2010). https://doi.org/10.1186/1477-9560-8-15
Buckberg, G.D.: Congestive heart failure: treat the disease, not the symptom: return to normalcy/Part II—the experimental approach. J. Thorac. Cardiovasc. Surg. 134, 844–849 (2007). https://doi.org/10.1016/j.jtcvs.2007.05.053
Oz, M.C., Gelijns, A.C., Miller, L., Wang, C., Nickens, P., Arons, R., Aaronson, K., Richenbacher, W., van Meter, C., Nelson, K., Weinberg, A., Watson, J., Rose, E.A., Moskowitz, A.J.: Left ventricular assist devices as permanent heart failure therapy: the price of progress. Ann. Surg. 238, 575–577 (2003). https://doi.org/10.1097/01.sla.0000090447.73384.ad
Gürsoy, M.O., Kalçık, M., Yesin, M., Karakoyun, S., Bayam, E., Gündüz, S., Özkan, M.: A global perspective on mechanical prosthetic heart valve thrombosis: diagnostic and therapeutic challenges. Anatol. J. Cardiol. 16, 980 (2016)
Cox, J.L.: The surgical treatment of atrial fibrillation: IV. Surgical technique. J. Thorac. Cardiovasc. Surg. 101, 584–592 (1991). https://doi.org/10.1016/S0022-5223(19)36685-1
Blum, K.M., Zakko, J., Fong, P., Maxfield, M.W., Cleary, M.A., Breuer, C.K.: Chapter 34 - Heart valve tissue engineering. Presented at the (2020)
Kim, D., Bresette, C., Liu, Z., Ku, D.N.: Occlusive thrombosis in arteries. APL Bioeng. 3, 41502 (2019). https://doi.org/10.1063/1.5115554
Violi, F., Pastori, D., Pignatelli, P.: Mechanisms and management of thrombo-embolism in atrial fibrillation. J. Atr. Fibrillation 7, 1112 (2014). https://doi.org/10.4022/jafib.1112
Yamakawa, K., Umemura, Y., Hayakawa, M., Kudo, D., Sanui, M., Takahashi, H., Yoshikawa, Y., Hamasaki, T., Fujimi, S., group, J.S.D.I.C. (J-S.D. study: Benefit profile of anticoagulant therapy in sepsis: a nationwide multicentre registry in Japan. Crit. Care 20, 229 (2016) https://doi.org/10.1186/s13054-016-1415-1
Hillegass, E., Puthoff, M., Frese, E.M., Thigpen, M., Sobush, D.C., Auten, B., Group, for the G.D.: Role of physical therapists in the management of individuals at risk for or diagnosed with venous thromboembolism: evidence-based clinical practice guideline. Phys. Ther. 96, 143–166 (2016). https://doi.org/10.2522/ptj.20150264
Dahl, O.E.: Mechanisms of hypercoagulability. Thromb. Haemost. 82, 902–906 (1999)
Rogers, H.J., Nakashima, M.O., Kottke-Marchant, K.: Hemostasis and Thrombosis. In: Hsi, E.D.B.T.H., Third, E. (eds.) Foundations in Diagnostic Pathology, pp. 57–105. Elsevier, Philadelphia (2018)
Tans, G., Nicolaes, G.A., Rosing, J.: Regulation of thrombin formation by activated protein C: effect of the factor V Leiden mutation. Semin. Hematol. 34, 244–255 (1997)
Tollefson, D.F., Friedman, K.D., Marlar, R.A., Bandyk, D.F., Towne, J.B.: Protein C deficiency. A cause of unusual or unexplained thrombosis. Arch. Surg. 123, 881–884 (1988). https://doi.org/10.1001/archsurg.1988.01400310095016
Berruyer, M., Francina, A., Ffrench, P., Negrier, C., Boneu, B., Dechavanne, M.: Increased thrombosis incidence in a family with an inherited protein S deficiency and a high oxygen affinity hemoglobin variant. Am. J. Hematol. 46, 214–217 (1994). https://doi.org/10.1002/ajh.2830460310
Lu, Z., Wang, F., Liang, M.: SerpinC1/Antithrombin III in kidney-related diseases. Clin. Sci. (Lond.) 131, 823–831 (2017). https://doi.org/10.1042/CS20160669
Morris, R.J., Woodcock, J.P.: Evidence-based compression: prevention of stasis and deep vein thrombosis. Ann. Surg. 239, 162–171 (2004). https://doi.org/10.1097/01.sla.0000109149.77194.6c
Line, B.R.: Pathophysiology and diagnosis of deep venous thrombosis. Semin. Nucl. Med. 31, 90–101 (2001). https://doi.org/10.1053/snuc.2001.21406
Eklof, B., Arfvidsson, B., Kistner, R.L., Masuda, E.M.: Indications for surgical treatment of iliofemoral vein thrombosis. Hematol. Oncol. Clin. North Am. 14, 471–482 (2000). https://doi.org/10.1016/s0889-8588(05)70146-5
Turetz, M., Sideris, A.T., Friedman, O.A., Triphathi, N., Horowitz, J.M.: Epidemiology, pathophysiology, and natural history of pulmonary embolism. Semin. Intervent. Radiol. 35, 92–98 (2018). https://doi.org/10.1055/s-0038-1642036
Khalaj, R., Douroumis, D.: 4—Applications of long-lasting and implantable drug delivery systems for cardiovascular disease treatment. In: Larrañeta, E., Raghu Raj Singh, T., Donnelly, R.F.B.T.L.A.D.D.S. (eds.) Woodhead Publishing Series in Biomaterials, pp. 83–127. Woodhead Publishing, Sawston (2022)
Sartoretti, C., Sartoretti-Schefer, S., Duff, C., Buchmann, P.: Angioplasty balloon catheters used for distraction of the ankle joint. Arthroscopy 12, 82–86 (1996). https://doi.org/10.1016/S0749-8063(96)90224-8
Balaji, N.R., Shah, P.B.: Radial artery catheterization. Circulation 124, e407–e408 (2011). https://doi.org/10.1161/CIRCULATIONAHA.111.019802
Byrne, R.A., Stone, G.W., Ormiston, J., Kastrati, A.: Coronary balloon angioplasty, stents, and scaffolds. Lancet 390, 781–792 (2017). https://doi.org/10.1016/S0140-6736(17)31927-X
McKavanagh, P., Zawadowski, G., Ahmed, N., Kutryk, M.: The evolution of coronary stents. Expert Rev. Cardiovasc. Ther. 16, 219–228 (2018). https://doi.org/10.1080/14779072.2018.1435274
Zhao, X., Liu, D., Yu, C., Sun, Y., Chen, S.: Treatment of aortic and iliac artery occlusion by catheter thrombolysis combined with catheter thrombectomy and aortic bifurcation endovascular stent reconstruction. Case Rep. Vasc. Med. 2021, 6084226 (2021). https://doi.org/10.1155/2021/6084226
Chaves, F., Garnacho-Montero, J., del Pozo, J.L., Bouza, E., Capdevila, J.A., de Cueto, M., Domínguez, M.Á., Esteban, J., Fernández-Hidalgo, N., Fernández Sampedro, M., Fortún, J., Guembe, M., Lorente, L., Paño, J.R., Ramírez, P., Salavert, M., Sánchez, M., Vallés, J.: Diagnosis and treatment of catheter-related bloodstream infection: clinical guidelines of the Spanish Society of Infectious Diseases and Clinical Microbiology and (SEIMC) and the Spanish Society of Spanish Society of Intensive and Critical Care Medicine a. Med. Intensiva 42, 5–36 (2018). https://doi.org/10.1016/j.medin.2017.09.012
MacDonald, D.A.: Pulsatile flow in a catheterised artery. J. Biomech. 19, 239–249 (1986). https://doi.org/10.1016/0021-9290(86)90156-9
Choi, S.U.S.: Nanofluids: From vision to reality through research. J. Heat Transfer 131, 1–9 (2009). https://doi.org/10.1115/1.3056479
Nsofor, C.E.: Recent Patents on Nanofluids (Nanoparticles in Liquids) Heat Transfer, http://www.eurekaselect.com/node/95146/article (2008)
Nadeem, S., Ul Haq, R., Khan, Z.H.: Heat transfer analysis of water-based nanofluid over an exponentially stretching sheet. Alexandria Eng. J. 53, 219–224 (2014). https://doi.org/10.1016/j.aej.2013.11.003
Afiqah, W.S., Sankar, D.S., Nagar, A.K.: Effects of catheter, stenosis and thrombosis in non-Newtonian blood flow through narrow arteries with clinical applications: a mathematical model. Int. J. Appl. Comput. Math. 8, 136 (2022). https://doi.org/10.1007/s40819-022-01335-z
Elnaqeeb, T., Mekheimer, K.S., Alghamdi, F.: Cu-blood flow model through a catheterized mild stenotic artery with a thrombosis. Math. Biosci. 282, 135–146 (2016). https://doi.org/10.1016/j.mbs.2016.10.003
Srivastava, V.P., Rastogi, R.: Blood flow through a stenosed catheterized artery: effects of hematocrit and stenosis shape. Comput. Math. Appl. 59, 1377–1385 (2010). https://doi.org/10.1016/j.camwa.2009.12.007
Lasne, D., Jude, B., Susen, S.: From normal to pathological hemostasis. Can. J. Anaesth. 53, S2-11 (2006). https://doi.org/10.1007/BF03022247
Sagripanti, A., Carpi, A.: Antithrombotic and prothrombotic activities of vascular endothelium. Biomed. Pharmacother. 54, 107–111 (2000). https://doi.org/10.1016/S0753-3322(00)88861-7
Ajjan, R.A., Kietsiriroje, N., Badimon, L., Vilahur, G., Gorog, D.A., Angiolillo, D.J., Russell, D.A., Rocca, B., Storey, R.F.: Antithrombotic therapy in diabetes: which, when, and for how long? Eur. Heart J. 42, 2235–2259 (2021). https://doi.org/10.1093/eurheartj/ehab128
Yamazaki, H., Mustard, J.F.: Platelet activation. Academic Press, Orlando, FL (1987)
Anthony Ware, J., Coller, B. S.: Platelet morphology, biochemistry, and function. In: Williams Hematology. McGraw Hill Publication. pp. 1161–1201 (1995)
Robinson, W.F., Robinson, N.A.: Cardiovascular system. Jubb, Kennedy Palmer’s Pathol. Domest. Anim. 3, 1-101.e1 (2016). https://doi.org/10.1016/B978-0-7020-5319-1.00012-8
Burki, S., Adachi, I.: Pediatric ventricular assist devices: current challenges and future prospects. Vasc. Health Risk Manag. 13, 177–185 (2017). https://doi.org/10.2147/VHRM.S82379
Butchart, E.G., Gohlke-Bärwolf, C., Antunes, M.J., Tornos, P., De Caterina, R., Cormier, B., Prendergast, B., Iung, B., Bjornstad, H., Leport, C., Hall, R.J.C., Vahanian, A., on behalf of the Working Groups on Valvular Heart Disease and Cardiac Rehabilitation and Exercise Physiology, European Society of Cardiology, T.: Recommendations for the management of patients after heart valve surgery. Eur. Heart J. 26, 2463–2471 (2005) https://doi.org/10.1093/eurheartj/ehi426
Van de Weerdt, E.K., Biemond, B.J., Baake, B., Vermin, B., Binnekade, J.M., van Lienden, K.P., Vlaar, A.P.J.: Central venous catheter placement in coagulopathic patients: risk factors and incidence of bleeding complications. Transfusion 57, 2512–2525 (2017). https://doi.org/10.1111/trf.14248
Gleich, S.J., Wong, A.V., Handlogten, K.S., Thum, D.E., Nemergut, M.E.: Major short-term complications of arterial cannulation for monitoring in children. Anesthesiology 134, 26–34 (2021). https://doi.org/10.1097/ALN.0000000000003594
Sankar, D.S., Hemalatha, K.: Pulsatile flow of Herschel-Bulkley fluid through stenosed arteries—a mathematical model. Int. J. Non. Linear. Mech. 41, 979–990 (2006). https://doi.org/10.1016/j.ijnonlinmec.2006.02.007
Sankar, D.S., Nagar, A.K.: Nonlinear fluid models for biofluid flow in constricted blood vessels under body accelerations: a comparative study. J. Appl. Math. 2012, 950323 (2012). https://doi.org/10.1155/2012/950323
Zidan, A.M., McCash, L.B., Akhtar, S., Saleem, A., Issakhov, A., Nadeem, S.: Entropy generation for the blood flow in an artery with multiple stenosis having a catheter. Alexandria Eng. J. 60, 5741–5748 (2021). https://doi.org/10.1016/j.aej.2021.04.058
Mekheimer, K.S., Elmaboud, Y.A.: The influence of a micropolar fluid on peristaltic transport in an annulus: application of the clot model. Appl. Bionics Biomech. 5, 302195 (2008). https://doi.org/10.1080/11762320802256666
Srinivasacharya, D., Mishra, M., Rao, A.R.: Peristaltic pumping of a micropolar fluid in a tube. Acta Mech. 161, 165–178 (2003). https://doi.org/10.1007/s00707-002-0993-y
Ellahi, R., Rahman, S.U., Nadeem, S., Akbar, N.S.: Blood flow of nanofluid through an artery with composite stenosis and permeable walls. Appl. Nanosci. 4, 919–926 (2014). https://doi.org/10.1007/s13204-013-0253-6
Ahmed, A., Nadeem, S.: The study of (Cu, TiO2, Al2O3) nanoparticles as antimicrobials of blood flow through diseased arteries. J. Mol. Liq. 216, 615–623 (2016). https://doi.org/10.1016/j.molliq.2016.01.059
Sankar, D.S., Lee, U.: Two-fluid Herschel–Bulkley model for blood flow in catheterized arteries. J. Mech. Sci. Technol. 22, 1008–1018 (2008). https://doi.org/10.1007/s12206-008-0123-4
Sankar, D.S.: A two-fluid model for pulsatile flow in catheterized blood vessels. Int. J. Non. Linear. Mech. 44, 337–351 (2009). https://doi.org/10.1016/j.ijnonlinmec.2008.12.008
Srivastava, V.P., Srivastava, R.: Particulate suspension blood flow through a narrow catheterized artery. Comput. Math. Appl. 58, 227–238 (2009). https://doi.org/10.1016/j.camwa.2009.01.041
Srivastava, V.P., Vishnoi, R., Mishra, S., Sinha, P.: Blood flow through a composite stenosis in catheterized arteries. J. Sci. Technol. 5, 55–64 (2010)
Mekheimer, K.S., Salama, F., Elkot, M.: The unsteady flow of a carreau fluid through inclined catheterized arteries having a balloon with time-variant overlapping stenosis. Walailak J. Sci. Technol. 12, 863–883 (2015)
El Kot, M.A., Abbas, W.: Numerical technique of blood flow through catheterized arteries with overlapping stenosis. Comput. Methods Biomech. Biomed. Engin. 20, 45–58 (2017). https://doi.org/10.1080/10255842.2016.1196198
Acknowledgements
The authors acknowledge the financial support extended by Universiti Teknologi Brunei for conducting this research through its internal Grant Scheme (UTB/GSR/2/2022 (15)).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they do not have any conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wajihah, S.A., Sankar, D.S. & Nagar, A.K. Influence of thrombosis, stenosis and catheter on rheological characteristics of blood: a systematic review. Arch Appl Mech 93, 4279–4304 (2023). https://doi.org/10.1007/s00419-023-02496-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00419-023-02496-z