Abstract
Purpose
Multifocal intraocular lenses (IOLs) offer the possibility of spectacle-free vision following cataract surgery compared to standard IOLs. Existing systematic reviews have generally concluded that multifocal IOLs result in better uncorrected near vision and greater spectacle independence, but more unwanted visual phenomena such as glare and halos, compared to monofocal IOLs. However, the certainty of evidence has been low for most outcomes, and pooled analyses have grouped together technologically obsolete lenses with newer lenses, potentially obscuring differences in performance across different lens types.
Methods
We performed a systematic review searching for RCTs of a multifocal IOL to a standard IOL or monovision that reported spectacle independence, visual acuity, or quality of life. Databases were searched from 1/1/2006–4/30/2017. Existing reviews were used to identify older studies. Title/abstract screening and data extraction were done in duplicate. Where possible, random effects meta-analysis was performed to synthesize results. In addition to comparing multifocal IOLs as a group to monofocal IOLs, we also compared newer diffractive lenses to obsolete or refractive lenses.
Results
Twenty-five eligible studies were identified. There was no difference in pooled estimates of corrected or uncorrected distance vision between multifocal and standard IOLs. Compared to monofocal IOLs, multifocal IOLs had statistically significantly better pooled results for the outcome of near vision (10 studies, 1025 patients, mean difference in logMAR of ‐0.26 (95% CI ‐0.37, ‐0.15)); spectacle dependence (12 studies, 1237 patients, relative risk of 0.27 (95% CI 0.20, 0.38)) and borderline significantly better quality of vision (6 studies, 596 patients, standardized mean difference of ‐0.54, (95% CI ‐1.12, 0.04)). Compared to monofocal IOLs, multifocal IOLs had statistically significantly worse pooled results for the outcomes of glare (9 studies, 847 patients, risk ratio of 1.36 (95% CI 1.15, 1.61) and halos (7 studies, 754 patients, risk ratio of 3.14 (95% CI 1.63, 6.08). Newer multifocal lenses had statistically significantly better outcomes than older diffractive lenses or refractive lenses, when compared to monofocal IOLs, in near vision, quality of vision, and risk of halos.
Conclusions
Multifocal IOLs compared to standard IOLs or monovision result in better uncorrected near vision and a higher proportion of patients who achieve spectacle independence, but greater risk of unwanted visual phenomena. Newer diffractive lenses may be better than refractive lenses in near vision and quality of vision outcomes, with less risk of halos than older diffractive lenses and refractive lenses.
(PROSPERO registration CRD42017069949)
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Expectations following cataract surgery have become increasingly high with many patients now desiring spectacle independence as an outcome. Multifocal intraocular lenses (MFIOL) may offer improved uncorrected near vision (UCVA) and spectacle independence, there may also be downsides including increases in unwanted visual symptoms such as glare, halo, and decreased contrast sensitivity [1].
An early systematic review, published in 2003, identified 8 eligible randomized controlled trials (RCTs) [2], and concluded based on pooled analyses that there were no statistically significant differences in distance vision (corrected or uncorrected) but better near vision and spectacle independence for patients receiving MFIOLs compared to monofocal intraocular lenses (IOLs). Patients with MFIOLs had statistically significantly more glare/haloes and worse contrast sensitivity than patients receiving monofocal IOLs. However this review only included older lenses that are currently not used. Two more systematic reviews, published in 2011 [3] and 2012 [4], included 20 and 29 studies, respectively, but only 8 and 5 of these were RCTs, and the latter study did not perform statistical pooling of results. Meanwhile the most recent Cochrane review [5] included newer lenses but pooled the data from new and old lenses together, concluding that distance visual acuity was no different between multifocal IOLs and monofocal IOLs; there is low-certainty evidence that near visual acuity was better with multifocal IOLs; there is low-certainty evidence that multifocal IOLs resulted in less spectacle dependence; and moderate-certainty evidence that visual phenomena like halos are more common with multifocal IOLs.
We therefore undertook a systematic review and meta-analysis to assess visual outcomes in patients receiving MFIOLs compared to either monofocal IOLs or monovision, and to compare results between newer and older IOLs. The key questions for this review were (1) What is the rate of spectacle independence of multifocal lenses compared to monofocal lenses; (2) What is the effectiveness in terms of distance and near vision; and (3) what are the harms of multifocal IOls versus monofocal IOLs in the setting of cataract surgery?
Methods
This is part of a larger review commissioned by the Department of Veterans Affairs [6]. A formal protocol was developed and submitted to PROSPERO (CRD42017069949) and exempt by the Institutional Review Board.
Search methods for identifying studies
We conducted searches in PubMed from 1/1/2006 to 4/30/2017 (Appendix for full search strategy) and included terms relating to “cataract” or “cataract extraction” and “lenses, intraocular” or “lens implantation, intraocular” and terms of multifocal lenses.
Study selection
Two team members independently screened the titles of retrieved citations. Inclusion criteria included RCTs of adults undergoing cataract extraction and comparing a multifocal lens with a standard monofocal lens or monovision and reporting spectacle independence. Additional outcomes were uncorrected and corrected distance vision, uncorrected near vision, validated measures of vision function (such as the VF-14) or quality of life. Harms included the harms of the surgery itself plus effects such as contrast sensitivity and aberrations like glare and halos. Outcomes could be measured at any time point following surgery. When multiple time points were reported, later time points were preferred to earlier time points.
Data collection and risk of bias assessment
Data extraction was completed in duplicate. All discrepancies were resolved with full group discussion. We abstracted data on the following: study design, single vs multi-site study, patient characteristics, intervention lenses, comparison monofocal lens, sample size, duration of follow-up, outcomes, and data needed for the Cochrane Risk of bias tool. RCTs were assessed for quality (risk of bias) with the Cochrane Risk of Bias tool [7] (see appendix).
Data synthesis and analysis
The sample size, mean, and standard deviation for each treatment group were extracted from articles that reported visual acuity using Snellen or logMAR measurements. Data that reported visual acuity using Snellen charts were converted into logMAR values. A mean difference (MD) was calculated for each comparison of multifocal and monofocal lenses. Similar data were collected for quality of life measures but since the scales varied, a standardized effect size (SMD) was calculated for each comparison. The sample size and number or percent of patients with spectacle independence was collected and a risk ratio (RR) was calculated for each comparison.
Meta-analyses were conducted for the visual acuity and quality of life outcomes using trials that reported a monofocal lens comparator. Because several trials reported comparisons of more than one intervention, two-level multilevel random effects models were estimated. [8] For the two trials that reported a monovision comparator, a fixed-effects meta-analysis was performed [9].
We categorized lenses as “refractive” (AMO Array SA40, AMO Rezoom NXG1, Storz Truevista, Hoya Isert PY60MV); “older diffractive” if they were no longer in use (3M 815LE, Pharmacia 808X, Laboratories Domilens Progress 3); or “newer diffractive” (AMO Tecnis ZM900, Alcon Restor SA60D3, Alcon Restor SN6AD1, Alcon Restor SN6AD3, Zeiss Acri-Lisa 366D, Zeiss Acri.tec Twin).
We pooled all eligible studies within outcome, and also performed stratified analyses that compared pooled results for newer diffractive lenses with refractive lenses and older diffractive lenses. We compared these pooled results using mixed-effects meta-regression.
Test of heterogeneity was reported using the I2 statistic [10]. Values of the I2 statistic close to 100% represent high degrees of heterogeneity. Begg rank correlation [11] and Egger regression asymmetry test [12] were used to examine publication bias. R version 3.4.1 was used for all statistical analyses.
Results
Description of the evidence
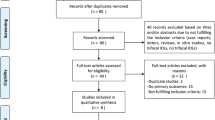
Our literature searches, expert recommendations, and reference mining identified 760 potentially relevant citations, of which 93 were included at the abstract screening. All 93 abstracts were included and obtained as full-text publications. Sixty-eight studies were excluded for the following reasons: No monofocal comparison group (n = 35); no multifocal comparison group (n = 8); not outcome of interest (n = 2); not RCT (n = 18); commentary (n = 1); background (n = 1); and duplicate (n = 3). A total of 25 publications were identified at full-text review that contributed to our final sample (Fig. 1). Details of included studies are provided in the Evidence Table (Appendix). A full list of excluded studies from the full-text review is included in Appendix D of the report [6].
All of the studies were single-site with seven exceptions [13,14,15,16,17,18,19,20]. Two studies were performed in the USA [16, 19], 4 studies were performed in China [22,23,24,25]. Sample sizes were modest, 9 studies enrolled 75 patients or less [17, 21, 23, 26,27,28,29,30,31], and only 2 studies enrolled more than 200 patients [13, 19]. The mean age of patients enrolled was 60–75 years of age, and patients were 50–60% female. Two studies compared the intervention lenses to monovision or mini-monovision [13, 28], where the two eyes have monofocal IOLs of different focal lengths, such that one eye sees predominantly distance vision and the other eye sees predominantly near vision. Nearly all studies reported visual acuity, 14 studies reported spectacle independence [13, 16, 18,19,20,21, 24,25,26, 28, 30,31,32,33] other outcomes were variably reported. We considered the two studies by Alio and colleagues [14, 27] and Allen and Haaskjold [17, 18] to potentially have overlapping patients. For the purpose of statistical pooling, we only used the Alio study with larger sample size and the Allen study because it had the outcomes of interest.
The quality of studies was in general low—one study was judged to be at low risk of bias across all domains [19] and three studies were at low risk of bias in all domains except one (Table 1) [16, 26, 31]. Since only two studies were reported as having had their protocol prospectively registered [13, 28], for example on clinicaltrials.gov, our ability to assess selective reporting bias is limited.
Effectiveness outcomes
Multifocal IOLs compared to monofocal IOLs—corrected and uncorrected distance vision
We identified 13 studies (with 24 comparisons and 1640 patients) [14, 18,19,20,21,22,23,24, 26, 31, 32, 34, 35] and 13 studies (with 23 comparisons and 1636 patients) [14, 16, 19,20,21, 24,25,26, 31, 32, 34,35,36] that reported corrected and uncorrected distance vision comparing multifocal IOLs to monofocal IOLs (that were not used for monovision). Figure 2 presents the data for uncorrected distance vision. The appendix presents the data for corrected distance vision. For both outcomes, there were no statistically significant differences in vision between the multifocal and monofocal IOLs.
Five older studies were not included in this analysis because they reported visual acuity outcomes as binary data, the proportion of patients seeing equal or better than some certain value [23, 29, 30, 37]. Pooled analyses of these 4 studies were consistent with the pooled results from the studies with logMAR outcomes, namely that there were no statistically significant differences between multifocal and monofocal IOLs for this outcome (appendix Figs. B and C).
Newer diffractive lenses compared to refractive lenses
There were no statistically significant differences between results for newer diffractive lenses as compared to refractive lenses.
Multifocal IOLs compared to monofocal IOLs—uncorrected near vision
We identified 10 studies (with 13 comparisons and 1025 patients) that reported uncorrected near vision comparing multifocal IOLs to monofocal IOLs (that were not used for monovision) [16, 19,20,21, 23,24,25,26, 31, 35]. Figure 3 presents the results. The random effects pooled estimate of effect in logMAR was − 0.26 (95% CI − 0.37, − 0.15) favoring multifocal IOLs. There was significant heterogeneity (I2 = 94.0%). There was no statistical evidence of publication bias (Begg’s test p = 0.86, Eggar’s test p = 0.30).
Six studies, four of which were not included in this analysis, reported their uncorrected near visual acuity outcomes as binary results, the proportion of patient seeing equal or better than some certain value [18, 23, 29, 33, 36, 37]. The pooled result of these studies was consistent with the pooled result of the studies with logMAR outcomes, with statistically significant benefits favoring multifocal IOLs (appendix Fig. D).
Newer diffractive lenses compared to refractive lenses
There was statistically significant evidence that newer diffractive lenses were better than refractive lenses (p = 0.01).
Multifocal IOLs compared to monofocal IOLs—spectacle independence
We identified 12 studies (with 17 comparisons and 1237 patients) that reported spectacle independence comparing multifocal IOLs to monofocal IOLs (that were not used for monovision) [16, 18,19,20,21, 24,25,26, 30,31,32,33]. Figure 4 presents the results. The random effects pooled estimate was a relative risk of 0.27 (95% CI 0.20, 0.38) favoring spectacle independence with multifocal IOLs. There was moderate heterogeneity (I2 = 40.2%). Begg’s and Eggar’s test for publication bias were p = .052 and .001, respectively. Removing the studies by Palmer and Kamlesh (showing 3x–10x greater benefits for spectacle independence than the other studies) made both publication bias tests nonsignificant while the result of better spectacle independence remained statistically significant.
Newer diffractive lenses compared to older lenses or refractive lenses
There was no evidence that newer diffractive lenses were better than refractive lenses or older diffractive lenses (p = 0.40 and 0.16, respectively).
Multifocal IOLs compared to monofocal IOLs—visual function/quality of life
Six studies presented data on visual function or quality of life for multifocal IOLs compared to monofocal IOLs [20, 24,25,26, 33, 35]. These studies included 9 comparisons and 596 patients. In 4 studies this outcome was measured with the VF-7 of VF-14, and in 2 studies it was measured as satisfaction with vision. The pooled random effects standardized mean difference was − 0.54 (95% CI − 1.12, 0.04) favoring multifocal IOLs (Fig. 5). There was substantial heterogeneity (I2 = 87.9%). There was no statistical evidence for publication bias (Begg’s test p = 0.35, Eggar’s test p = 0.58).
Newer diffractive lenses compared to refractive lenses
There was statistically significant evidence that newer diffractive lenses resulted in better visual function/satisfaction than refractive lenses (p < 0.01).
Multifocal IOLs compared to monofocal IOL as monovision
We identified 2 RCTs that compared multifocal IOLs to monofocal IOLs as monovision [13, 28]. We pooled these studies with a fixed-effect model. There was no statistically significant difference in uncorrected distance vision. Corrected distance vision was not reported. The pooled fixed-effect logMAR for uncorrected near vision was − 0.03 (95% CI − 0.07, 0.00) favoring multifocal IOLs. For spectacle independence, the pooled fixed-effect was a risk ratio of 0.40 (95% CI 0.29, 0.53) favoring multifocal IOLs. There was no statistical evidence of publication bias.
Harms
Surgical complications
Twelve of the 25 multifocal IOL studies specifically commented on the presence (or absence) of surgical adverse events, with varying degrees of detail [13, 18, 19, 22, 24,25,26,27, 29, 31, 35, 37]. These outcomes are presented in Table 2. We considered the two studies by Alio to have potentially overlapping patients, so we include here only the 1 study by Alio that reported adverse events.
Contrast sensitivity
There were 16 of the 25 multifocal IOL studies that reported contrast sensitivity [13, 16,17,18, 22,23,24,25,26, 28,29,30,31,32,33, 35]. In the older studies, Allen, Haaskjold, and Kamlesh showed worse contrast sensitivity with multifocal IOLs at all light levels compared with monofocal lenses. Zeng showed statistically significant contrast sensitivity issues for the Array SA40N compared to the monofocal lens. Cillino showed better contrast sensitivity with the monofocal lens (AR40) and multifocal lens (ZM900) compared to the Array and ReZoom lenses (p = 0.038). Palmer showed monofocal IOLs with statistically significant better contrast sensitivity compared to the ZM900 and TwinSet lens at all spatial frequencies and luminance. Meanwhile, the difference was only significant between the monofocal and ReZoom at high spatial frequencies in scotopic conditions.
Ji showed lower contrast sensitivity with the ReSTOR lens compared to monofocal lens under all 6 spatial frequencies with mesopic and photopic conditions. Compared to monovision, multifocal lenses had less contrast sensitivity according to Wilkins (2013). Meanwhile Steinert and Peng showed worse contrast with the multifocal lenses at low contrast but no difference at higher contrast. Rosetti showed no difference in contrast sensitivity. Percival, Sen, and Leyland both showed less contrast sensitivity with multifocal IOLs that did not reach statistical significance.
Zhao showed no difference in contrast sensitivity between the ReSTOR lens (SA60AD3) and the monofocal lens (SA60AT). Labiris and colleagues reported no difference in contrast comparing “mini-monovision” with a refractive multifocal lens.
Glare
There were 16 of 25 multifocal IOL studies reporting glare following surgery [13, 16, 18,19,20,21,22, 24,25,26, 28,29,30,31, 33, 35]. We pooled the nine studies reporting binary outcomes for glare, which totaled 847 patients [14, 19, 22, 26, 27, 30, 31, 34, 36]. The random effects pooled estimate was a risk ratio of 1.36 (95% CI 1.15, 1.61) favoring monofocal IOLs in minimizing glare. (Fig. 6) There was no heterogeneity (I2 = 0.0%). Begg’s and Eggar’s test did not show any evidence of publication bias.
Newer diffractive lenses compared to older lenses or refractive lenses
There was no evidence of differences between newer diffractive lenses and refractive lenses or older diffractive lenses.
Halos
There were 8 of 25 multifocal IOL studies reporting halos following surgery [13, 18, 24,25,26, 30, 33, 35]. We pooled the seven studies reporting binary outcomes for halo/unwanted images, which totaled 754 patients [13, 18, 25, 26, 30, 33, 35]. The random effects pooled estimate was a risk ratio of 3.14 (95% CI 1.63, 6.08) favoring monofocal IOLs. Heterogeneity was high (I2 = 64.2%). Begg’s test was nonsignificant (p = 0.40) but Eggar’s test for publication bias was significant (p = 0.01) (Fig. 7).
Newer diffractive lenses compared to older lenses or refractive lenses
There was statistically significant evidence that newer diffractive lenses were associated with a lower risk of increased halos than older diffractive lenses (p = 0.02) and borderline evidence that newer diffractive lenses were better than refractive lenses (p = 0.054).
Other visual phenomena
Palmer noted that more patients had complaints of dysphotopsias in the ZM900 group (81%) compared to the TwinSet (47%) and ReZoom (53%) and monofocal groups (48%) [32]. The authors also point out that no patient in the monofocal group complained on their own about photopsias compared to 16–18% of the multifocal IOL patients. Labiris commented on complaints of shadows following surgery being higher in the multifocal IOL group compared to mini monovision [28]. The study also commented there was no difference in stereopsis between multifocal IOL and mini monovision. This was in contrast to Jusufovic which described less stereopsis in the monofocal IOL group compared to the multifocal IOLs at higher levels of but not in lower levels [36].
Discussion
The principal findings from our systematic review and meta-analysis are that compared to monofocal lenses, multifocal intraocular lenses have benefits for UNVA and spectacle independence but also increased risk for reduced contrast sensitivity and other visual phenomena such as glare and halo. In addition, compared to monofocal IOLs newer MFIOLs had statistically significantly better outcomes than older lenses or refractive lenses for improved near vision, quality of vision and reduced unwanted visual phenomena.
In a majority of studies, intraoperative complications were reported as either none or there was no difference between multifocal and monofocal groups. There were few reports of late-onset complications in eyes treated with multifocal IOLs such as IOL decentration and posterior capsule opacification requiring further treatment. In one study, 6 patients ultimately required IOL exchange due to dissatisfaction with the multifocal lens [13]. For surgeons planning to implant these lenses, knowledge on how to address these issues is important.
Our results amplify and augment prior systematic reviews. We were able to include more eligible RCTs than any prior review, and additionally were able to perform subgroup analyses on certain categories of lens types. We found that newer diffractive lenses may result in better near visual acuity, better visual function/quality of life, and less risk of halos than refractive or older diffractive lenses, when compared to monofocal IOLs.
There were insufficient data for us to perform a specific analysis of intermediate vision outcomes or defocus curves, nor could we directly compare refractive and diffractive IOLs included in our review. Most of the included studies excluded patients due to pre-existing ocular conditions such as corneal astigmatism and macular disease. Detecting these conditions requires additional pre-operative testing such as corneal topography/tomography and macular optical coherence tomography. Additional resources may also be needed to counsel patients on the risks/benefits of multifocal IOLs and to manage suboptimal post-operative outcomes.
Our study has several limitations. As in all systematic reviews and meta-analyses, the primary limitation is the quantity and quality of the original trials with possibility of compromised by one or more key elements of bias. Only four studies were at low risk of bias in all [19] or four of the five domains [16, 26, 31] and only two trials were prospectively registered [13, 28], increasing concern about potential hidden methodological bias. Studies did not systematically report operative events and the need for re-operation, or the need for any additional resources pre-operatively or post-operatively in patients receiving multifocal IOLs as compared to monofocal IOLs. Also, for some pooled results, unexplained heterogeneity was substantial. This could be due to differences in the lenses being studied, the methods of the trials, the presence of publication bias, or random chance. Nevertheless, we judged that for most outcomes there were no serious limitations in terms of the consistency of the results. Lastly, we recognize that IOL technology is ever-evolving and that our review could not include newer IOLs and technologies that are currently in use or in late-phase clinical trials, and have yet to publish controlled trials comparing them to standard IOLs.
In summary, our review has expanded our knowledge about the potential benefits and risks of multifocal IOLs as compared to monofocal IOLs. Multifocal IOLs provide clear benefit in terms of uncorrected near visual acuity and spectacle independence but can cause unwanted and bothersome visual symptoms and reduced contrast sensitivity. Newer diffractive lenses may have advantages to older diffractive lenses or refractive lenses in terms of improved near vision, quality of vision and reduced unwanted visual phenomena. Additional resources may be required to evaluate, counsel, and manage patients receiving multifocal IOLs as compared to monofocal IOLs and these have not been quantified. Future research will be required to evaluate not only the potential benefits and risks but also the trade-offs of varying IOL technologies.
References
de Vries NE, Webers CA, Touwslager WR, Bauer NJ, de Brabander J, Berendschot TT, Nuijts RM (2011) Dissatisfaction after implanation of multifocal intraocular lenses. J Cataract Refract Surg 37(5):859–865
Leyland M, Zinicola E (2003) Multifocal versus monofocal intraocular lenses in cataract surgery: a systematic review. Ophthalmology 110(9):1789–1798. https://doi.org/10.1016/S0161-6420(03)00722-X
Cochener B, Lafuma A, Khoshnood B, Courouve L, Berdeaux G (2011) Comparison of outcomes with multifocal intraocular lenses: a meta-analysis. Clin Ophthalmol 5:45–56. https://doi.org/10.2147/OPTH.S14325
Agresta B, Knorz MC, Kohnen T, Donatti C, Jackson D (2012) Distance and near visual acuity improvement after implantation of multifocal intraocular lenses in cataract patients with presbyopia: a systematic review. J Refract Surg 28(6):426–435. https://doi.org/10.3928/1081597X-20120518-06
de Silva SR, Evans JR, Kirthi V, Ziaei M, Leyland M (2016) Multifocal versus monofocal intraocular lenses after cataract extraction. Cochrane Database Syst Rev 12:CD003169. https://doi.org/10.1002/14651858.CD003169.pub4
Khandelwal SS, Jun J, Mak S, Shanman R, Booth M, Beroes JM, Shekelle PG (2018) Comparative effectiveness of multifocal, accommodative, and monofocal intraocular lenses for cataract surgery and lens replacement. Department of Veterans Affairs, Washington DC
Higgins JP, Altman DG, Gotzsche PC, Juni P, Moher D, Oxman AD, Savovic J, Schulz KF, Weeks L, Sterne JA, Cochrane Bias Methods G, Cochrane Statistical Methods G (2011) The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 343:d5928. https://doi.org/10.1136/bmj.d5928
Konstantopoulos S (2011) Fixed effects and variance components estimation in three-level meta-analysis. Res Synth Methods 2(1):61–76. https://doi.org/10.1002/jrsm.35
Hedges LV, Vevea JL (1998) Fixed-and random-effects models in meta-analysis. Psychol Methods 3(4):486
Higgins JP, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analyses. BMJ 327(7414):557–560. https://doi.org/10.1136/bmj.327.7414.557
Begg CB, Mazumdar M (1994) Operating characteristics of a rank correlation test for publication bias. Biometrics 50(4):1088–1101
Egger M, Davey Smith G, Schneider M, Minder C (1997) Bias in meta-analysis detected by a simple, graphical test. BMJ 315(7109):629–634
Wilkins MR, Allan BD, Rubin GS, Findl O, Hollick EJ, Bunce C, Xing W, Moorfields IOLSG (2013) Randomized trial of multifocal intraocular lenses versus monovision after bilateral cataract surgery. Ophthalmology 120(12):2449–2455.e1. https://doi.org/10.1016/j.ophtha.2013.07.048
Alio JL, Grabner G, Plaza-Puche AB, Rasp M, Pinero DP, Seyeddain O, Rodriguez-Prats JL, Ayala MJ, Moreu R, Hohensinn M, Riha W, Dexl A (2011) Postoperative bilateral reading performance with 4 intraocular lens models: six-month results. J Cataract Refract Surg 37(5):842–852. https://doi.org/10.1016/j.jcrs.2010.11.039
Marchini G, Mora P, Pedrotti E, Manzotti F, Aldigeri R, Gandolfi SA (2007) Functional assessment of two different accommodative intraocular lenses compared with a monofocal intraocular lens. Ophthalmology 114(11):2038–2043. https://doi.org/10.1016/j.ophtha.2006.12.034
Steinert RF, Post CT Jr, Brint SF, Fritch CD, Hall DL, Wilder LW, Fine IH, Lichtenstein SB, Masket S, Casebeer C et al (1992) A prospective, randomized, double-masked comparison of a zonal-progressive multifocal intraocular lens and a monofocal intraocular lens. Ophthalmology 99(6):853–860 discussion 860–851
Haaskjold E, Allen ED, Burton RL, Webber SK, Sandvig KU, Jyrkkio H, Leite E, Liekfeld A, Philipson B, Nystrom A, Wollensak J (1998) Contrast sensitivity after implantation of diffractive bifocal and monofocal intraocular lenses. J Cataract Refract Surg 24(5):653–658
Allen ED, Burton RL, Webber SK, Haaskjold E, Sandvig K, Jyrkkio H, Leite E, Nystrom A, Wollensak J (1996) Comparison of a diffractive bifocal and a monofocal intraocular lens. J Cataract Refract Surg 22(4):446–451
Javitt JC, Steinert RF (2000) Cataract extraction with multifocal intraocular lens implantation: a multinational clinical trial evaluating clinical, functional, and quality-of-life outcomes. Ophthalmology 107(11):2040–2048
Nijkamp MD, Dolders MG, de Brabander J, van den Borne B, Hendrikse F, Nuijts RM (2004) Effectiveness of multifocal intraocular lenses to correct presbyopia after cataract surgery: a randomized controlled trial. Ophthalmology 111(10):1832–1839. https://doi.org/10.1016/j.ophtha.2004.05.023
Harman FE, Maling S, Kampougeris G, Langan L, Khan I, Lee N, Bloom PA (2008) Comparing the 1CU accommodative, multifocal, and monofocal intraocular lenses: a randomized trial. Ophthalmology 115(6):993–1001.e2. https://doi.org/10.1016/j.ophtha.2007.08.042
Zeng M, Liu Y, Liu X, Yuan Z, Luo L, Xia Y, Zeng Y (2007) Aberration and contrast sensitivity comparison of aspherical and monofocal and multifocal intraocular lens eyes. Clin Exp Ophthalmol 35(4):355–360. https://doi.org/10.1111/j.1442-9071.2007.01452.x
Ji J, Huang X, Fan X, Luo M (2013) Visual performance of Acrysof ReSTOR compared with a monofocal intraocular lens following implantation in cataract surgery. Exp Ther Med 5(1):277–281. https://doi.org/10.3892/etm.2012.740
Peng C, Zhao J, Ma L, Qu B, Sun Q, Zhang J (2012) Optical performance after bilateral implantation of apodized aspheric diffractive multifocal intraocular lenses with +3.00-D addition power. Acta Ophthalmol 90(8):e586–e593. https://doi.org/10.1111/j.1755-3768.2012.02497.x
Zhao G, Zhang J, Zhou Y, Hu L, Che C, Jiang N (2010) Visual function after monocular implantation of apodized diffractive multifocal or single-piece monofocal intraocular lens randomized prospective comparison. J Cataract Refract Surg 36(2):282–285. https://doi.org/10.1016/j.jcrs.2009.08.037
Cillino S, Casuccio A, Di Pace F, Morreale R, Pillitteri F, Cillino G, Lodato G (2008) One-year outcomes with new-generation multifocal intraocular lenses. Ophthalmology 115(9):1508–1516. https://doi.org/10.1016/j.ophtha.2008.04.017
Alio JL, Plaza-Puche AB, Pinero DP, Amparo F, Rodriguez-Prats JL, Ayala MJ (2011) Quality of life evaluation after implantation of 2 multifocal intraocular lens models and a monofocal model. J Cataract Refract Surg 37(4):638–648. https://doi.org/10.1016/j.jcrs.2010.10.056
Labiris G, Giarmoukakis A, Patsiamanidi M, Papadopoulos Z, Kozobolis VP (2015) Mini-monovision versus multifocal intraocular lens implantation. J Cataract Refract Surg 41(1):53–57. https://doi.org/10.1016/j.jcrs.2014.06.015
Percival SS, Setty SS (1993) Prospectively randomized trial comparing the pseudoaccommodation of the AMO ARRAY multifocal lens and a monofocal lens. J Cataract Refract Surg 19(1):26–31
Kamlesh, Dadeya S, Kaushik S (2001) Contrast sensitivity and depth of focus with aspheric multifocal versus conventional monofocal intraocular lens. Can J Ophthalmol 36(4):197–201
Leyland MD, Langan L, Goolfee F, Lee N, Bloom PA (2002) Prospective randomised double-masked trial of bilateral multifocal, bifocal or monofocal intraocular lenses. Eye (Lond) 16(4):481–490
Martinez Palmer A, Gomez Faina P, Espana Albelda A, Comas Serrano M, Nahra Saad D, Castilla Cespedes M (2008) Visual function with bilateral implantation of monofocal and multifocal intraocular lenses: a prospective, randomized, controlled clinical trial. J Refract Surg 24(3):257–264
Rossetti L, Carraro F, Rovati M, Orzalesi N (1994) Performance of diffractive multifocal intraocular lenses in extracapsular cataract surgery. J Cataract Refract Surg 20(2):124–128
Rasp M, Bachernegg A, Seyeddain O, Ruckhofer J, Emesz M, Stoiber J, Grabner G, Dexl AK (2012) Bilateral reading performance of 4 multifocal intraocular lens models and a monofocal intraocular lens under bright lighting conditions. J Cataract Refract Surg 38(11):1950–1961. https://doi.org/10.1016/j.jcrs.2012.07.027
Sen HN, Sarikkola AU, Uusitalo RJ, Laatikainen L (2004) Quality of vision after AMO Array multifocal intraocular lens implantation. J Cataract Refract Surg 30(12):2483–2493. https://doi.org/10.1016/j.jcrs.2004.04.049
Jusufovic V, Sarajlic D, Zvornicanin J, Musanovic Z, Halilbasic M (2011) Comparison of the binocular vision quality after implantation of monofocal and multifocal intraocular lenses. Acta Med Saliniana 40(2):63–68. https://doi.org/10.5457/ams.174.10
el-Maghraby A, Marzouky A, Gazayerli E, Van der Karr M, DeLuca M (1992) Multifocal versus monofocal intraocular lenses. Visual and refractive comparisons. J Cataract Refract Surg 18(2):147–152
Funding
The Veterans Affairs Quality Enhancement Research Initiative provided financial support. The sponsor had no role in the design or conduct of this research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This type of study is exempt by the Institutional Review Board.
Informed consent
For this type of study, formal consent is not required.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 623 kb)
Rights and permissions
OpenAccess This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Khandelwal, S.S., Jun, J.J., Mak, S. et al. Effectiveness of multifocal and monofocal intraocular lenses for cataract surgery and lens replacement: a systematic review and meta-analysis. Graefes Arch Clin Exp Ophthalmol 257, 863–875 (2019). https://doi.org/10.1007/s00417-018-04218-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-018-04218-6