Abstract
To assess the visual effects of trifocal intraocular lenses (IOLs) compared to bifocal IOLs in cataract surgery, a meta-analysis of prospective comparative clinical trials (including 4 randomized controlled trials and 4 cohorts) was conducted. The defocus curves showed a better distance-corrected intermediate visual acuity (VA) for the trifocal group (MD −0.07; 95% CI, −0.10 to −0.05; p < 0.00001), while the VA outcomes showed no significant difference in distance VA (MD −0.03; 95% CI, −0.06 to 0.01; p = 0.13 for uncorrected distance VA and MD −0.00; 95% CI, −0.01 to 0.01; p = 0.78 for distance-corrected distance VA), near VA (MD −0.01; 95% CI, −0.07 to 0.04; p = 0.68 for uncorrected near VA and MD −0.01; 95% CI, −0.06 to 0.04; p = 0.66 for distance-corrected near VA) or refraction between the two groups. Contrast sensitivity and subjective visual quality yielded less conclusive results. Overall, a patient may achieve better intermediate VA with a trifocal IOL than with a bifocal IOL without any adverse effect on distance or near VA. The findings on contrast sensitivity and subjective visual quality were heterogeneous, with no clear results favoring either option.
Similar content being viewed by others
Introduction
Cataracts are very common in older people, leading to a decrease in vision and quality of life. Surgery to remove the cloudy crystalline lens and replace it with an artificial intraocular lens (IOL) is the only effective treatment. More and more patients presenting for cataract surgery want to enjoy good vision at distance, intermediate, and near ranges without the use of spectacles. Multifocal IOLs that can provide a wide range of clear vision attempt to meet this objective1,2.
At present, most multifocal IOLs are bifocal, with only near and far foci; the quality of intermediate viewing activities such as computer use might be insufficient for daily life3,4,5. Manufacturers have recently introduced multifocal IOLs that are trifocal in design, providing functional far, intermediate, and near vision2,6,7,8. Optical evaluation of multifocal IOLs has demonstrated that trifocal IOLs achieved a useful third focus for intermediate vision but were associated with increased background glare and halos and reduced visual quality9,10.
Clinical evaluation of multifocal IOLs is less clear-cut. There have been several studies comparing visual outcomes after the implantation of bifocal and trifocal IOLs in recent years1,2,3,4,5,6,7,8. Some studies support the notion of trifocal IOLs as the next generation of multifocal IOLs, which improve intermediate vision and the continuum of functional vision without impairing distance and near vision5,6,7. However, another study reports that bifocal IOLs provide intermediate visual acuity (VA) similar to trifocal IOLs2. Other studies suggest that the diffractive design of trifocal IOLs splits more incoming light than bifocal IOLs, which has the potential to decrease contrast sensitivity and increase photic phenomena1,9. To our knowledge, no systematic review and meta-analysis has been reported on this topic. We sought to conduct a meta-analysis of the existing randomized controlled trials (RCTs) and prospective cohorts to compare the visual results achieved with trifocal IOLs and bifocal IOLs.
Results
Search results
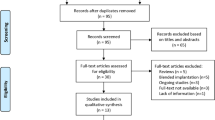
After adjusting for duplicates, 80 different studies were identified. Of these studies, 40 were excluded because their titles or abstracts did not meet the inclusion criteria. The full text of each of the remaining 40 citations was examined in more detail. From these 40 citations, 32 studies were excluded for the following reasons: 15 did not fulfill inclusion criteria, 15 studies did not provide primary outcomes, and two were duplications. Four RCTs2,3,4,5 and four prospective cohorts1,6,7,8 were ultimately included in this meta-analysis. Figure 1 shows the flow diagram for the search and selection process.
Study characteristics and quality
Eight studies that reported on 245 eyes (123 participants) with trifocal IOL implantation and 244 eyes (122 participants) with bifocal IOL implantation were included in this research. The eight studies were all conducted in European countries: France4, Norway1,5, the Netherlands2, the Czech Republic6, and Spain3,7,8. Table 1 summarizes the main characteristics of the included studies, and their quality is assessed in Supplementary Tables S1 and S2. Follow-up ranged from three to six months. Masking of surgeons is impossible in RCTs, and one study reported that patients were masked2. No RCT scored higher than three points. Of the prospective non-randomized comparative studies, one matched the preoperative VA of eyes in trifocal and bifocal groups7, two studies did not match preoperative VA6,8, and the other study did not discuss preoperative VA at all1. The age factor differed significantly between groups in two studies1,6. All four cohorts were of relatively low risk of bias, scoring equal to 7/8 on the Newcastle-Ottawa Scale (NOS). The overall quality of the meta-analysis is shown in Table 2. The assessment was considered to be of high to very low quality. Study design was the main reason to downgrade the overall quality of evidence, as the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) group suggested. Moreover, high heterogeneity and a limited number of eyes enrolled downgraded the quality of outcomes.
Primary outcome criteria
Visual acuity
Four RCTs reported uncorrected distance visual acuity (UDVA) or corrected distance visual acuity (CDVA) as outcomes (Fig. 2a and b, Table 2, Supplementary Table S3) and analyses including only RCTs did not reveal any statistically difference between the trifocal and bifocal groups (MD −0.03; 95% CI, −0.06 to 0.01; p = 0.13 for UDVA and MD −0.00; 95% CI, −0.01 to 0.01; p = 0.78 for CDVA)2,3,4,5. The quality of the evidence was moderate to high. Combined with cohorts, most studies reported these outcomes (Supplementary Figs S1 and S2)1,2,3,4,5,6,7,8. There was a statistically significant but small difference in the overall effect in each outcome that favored trifocal IOLs, with better distance vision compared with bifocal IOLs (MD −0.06; 95% CI, −0.10 to −0.02; p = 0.004 for UDVA and MD −0.02; 95% CI, −0.03 to −0.00; p = 0.04 for CDVA). The quality of the evidence was low.
(a) Forest plot showing the MD of UDVA comparing trifocal intraocular lens (IOL) with bifocal IOL postoperatively (only for RCTs). (b) Forest plot showing MD of CDVA comparing trifocal IOL with bifocal IOL postoperatively (only for RCTs). (c) Forest plot showing the MD of UNVA comparing trifocal IOL with bifocal IOL postoperatively. (d) Forest plot showing the MD of DCNVA comparing trifocal IOL with bifocal IOL postoperatively.
Two studies reported uncorrected intermediate visual acuity (UIVA) and distance-corrected intermediate visual acuity (DCIVA) as outcomes (Supplementary Figs S3 and S4)2,6. There was no significant difference in the overall effect in each outcome (MD −0.10; 95% CI, −0.36 to 0.17; p = 0.48 for UIVA and MD −0.12; 95% CI, −0.36 to 0.13; p = 0.35 for DCIVA), but only two studies, both characterized by high heterogeneity (I2 = 96%, Tau2 = 0.03), included this outcome.
Five studies reported uncorrected near visual acuity (UNVA) or distance-corrected near visual acuity (DCNVA) as outcomes (Fig. 2c and d, Table 2, Supplementary Table S3)2,4,6,7,8. Near VA was not significantly different between the trifocal and bifocal groups (MD −0.01; 95% CI, −0.07 to 0.04; p = 0.68 for UNVA and MD −0.01; 95% CI, −0.06 to 0.04; p = 0.66 for DCNVA). The quality of the evidence was low. However, the studies were characterized by high heterogeneity (I2 > 80%, Tau2 = 0.00). One trial (Mojzis et al.) had significant problems with comparability and we repeated relevant analysis excluding this trial6. Sensitivity analysis revealed Mojzis et al.’s study6 as the source of statistical heterogeneity for both the UNVA and DCNVA outcomes. After excluding Mojzis et al.’s study, no evidence of heterogeneity was detected (I2 = 41% for UNVA and I2 = 0% for DCNVA), but the results of the previous analysis did not change, as there was still no significant difference between the two groups.
Defocus curve
Similar defocus curves were recorded by seven studies (Table 3)1,2,3,4,5,6,7, all of which suggested that the trifocal group tended to perform better than the bifocal group, especially at the intermediate distance, although both groups demonstrated a decline in VA at that distance. However, two studies reported that the bifocal group achieved significantly better near VA than the trifocal group2,6. Among the seven studies, three provided distance-corrected defocus curve data for meta-analyses (Table 4)1,5,6. The results demonstrated that the trifocal group achieved better VA at defocus levels of −1.50 D to −0.50 D than the bifocal group, including a significant difference at intermediate vision (−1.50 D) with low heterogeneity (I2 = 23%).
Contrast sensitivity
Five studies assessed contrast sensitivity (Table 5)2,3,4,6,8. Findings differed between photopic and mesopic light conditions. Under photopic light conditions, Cochener4 and Jonker et al.2 reported that no statistically significant differences were observed between the two groups. However, a significantly higher level of contrast sensitivity was found for spatial frequency of three cpd in the trifocal group than in the bifocal group in Mojzis et al.’s study6. Under mesopic light conditions, Bilbao-Calabuig et al.3 and Plaza-Puche et al.8 reported no statistically significant differences between the two groups, but contrast sensitivity values were significantly better in the bifocal group at a frequency of six cpd under mesopic conditions in Jonker et al.’s study2.
Quality of vision
Visual quality as recorded by validated questionnaires was assessed in four studies (Table 6)1,2,4,5. High satisfaction was reported in both groups1,4. No statistically significant differences with respect to subjective visual quality, such as glare or halos, between the trifocal and bifocal groups were reported in most questionnaires2,4,5. However, Gundersen and Potvin1 reported that significantly fewer visual disturbances were present in the bifocal group. Spectacle independence was achieved more frequently with trifocal than with bifocal IOL implants in Jonker et al.’s study2.
Refraction
Postoperative refraction—cylinder, sphere, and spherical equivalent—were reported in six studies (Supplementary Figs S5–S7)1,2,5,6,7,8. This meta-analysis did not find any statistically significant difference with respect to postoperative refraction between the trifocal and bifocal groups (MD 0.09; 95% CI, −0.05 to 0.23; p = 0.20 for cylinder, MD 0.12; 95% CI, −0.13 to 0.37; p = 0.34 for sphere and MD 0.03; 95% CI, −0.06 to 0.13; p = 0.47 for spherical equivalent).
Publication bias
Publication bias was tested using Begg’s and Egger’s tests. These tests did not show significant results in all comparisons (Table 4 and Supplementary Table S3). These results indicated little publication bias.
Discussion
The present study analyzed whether and to what extent trifocal IOLs perform better than bifocal IOLs in terms of VA (including defocus curve), refraction, contrast sensitivity, and visual quality. The studies were similar in finding a better distance-corrected intermediate (as demonstrated by the defocus curves) VA with trifocal IOLs. However, there was no significant difference in distance VA, near VA or refraction between the two groups. Contrast sensitivity and subjective visual quality yielded less conclusive results.
The variation in follow-up intervals was a major difficulty in conducting this meta-analysis. Subgroup analysis with regard to follow-up length could not be performed due to the limited number of included studies. There is no general accepted follow-up duration for reporting the results of trials involving cataract surgeries. Based on previous studies and the authors’ own clinical experience, data for VA, refraction, contrast sensitivity, and subjective visual quality appears to remain stable at three months postoperatively and beyond, so we pooled the data reported at the end of follow-up for comparison. The combination of data from RCTs and cohort studies was another difficulty. We chose the results of analyses including only RCTs as the primary results for distance VA outcomes. Moreover, there were only one or two RCTs reporting the other outcomes, such as intermediate VA, near VA, refraction, and defocus curve. No heterogeneity between RCTs and cohorts was detected for those outcomes. Considering the inadequate number of RCTs and the high quality of cohorts, we retained cohorts to supplement existing randomized trial evidence.
Data from RCTs on distance VA did not reveal any significant difference between trifocal and bifocal IOLs. Combined with cohorts, the results demonstrated that trifocal IOL implantation provided a statistically significant but small advantage in UDVA and CDVA. The results confirmed that the generation of a third focal point by trifocal IOLs was not detrimental to the distance focal point6. The variability between studies in terms of sample size, clinical protocols used to obtain VA measurements, or patient features may have played a major role in the discrepancies among the studies6.
In terms of intermediate VA, the present study’s result would not be credible due to the limited number of studies available and their high heterogeneity. Combined with the results of the defocus curve, the trifocal group performed better than the bifocal group at the intermediate distance as expected, since bifocal IOLs have a greater decline in VA in the intermediate range. The meta results of the defocus curve demonstrated that the trifocal group achieved better VA at defocus levels of −1.50 D to −0.50 D than the bifocal group, including a significant but relatively small difference (−0.07) at −1.50 D (intermediate vision) with low heterogeneity (I2 = 23%), and small (−0.06) and modest (−0.12) differences with high heterogeneity (I2 = 76%) at −0.50 D and −1.00 D, respectively. Since all studies indicated that the trifocal group achieved better intermediate VA than the bifocal group1,2,3,4,5,6,7, there was reason to believe that the statistically significant difference was clinically meaningful. Previous bench studies comparing the multifocal components of both IOLs found that trifocal IOLs provide a true third intermediate focal point not found with bifocal IOLs9,10. Considering that no significant differences were present between the two groups in refraction outcomes, IOL optical behavior appears to be the main factor for this finding6. The defocus curve outcome also demonstrated that the trifocal group provided a continuum of functional VA at all three distance ranges. The intermediate focal point and continuum of VA are expected to improve patient satisfaction relative to bifocal IOLs, since bifocal IOLs have a greater decline in VA in the intermediate range11.
In terms of near VA, no significant differences were found between the two groups. It is worth noting that the additional intermediate focal point in trifocal IOLs did not appear to impact distance or near vision negatively5. However, the quality of evidence supporting the near VA is deemed to be low because of the study design and high heterogeneity. Thus, the conclusion should be interpreted cautiously. Mojzis et al.’s study6 with lower methodological quality was the source of statistical heterogeneity for the outcome. This study scored zero in comparability part of NOS scale, because it was the only one in which both the most important factor (preoperative VA) and the second important factor (age factor) differed significantly between groups. However, excluding this study did not change the effect estimates.
To understand the visual quality obtained with such multifocal IOLs, it is important to analyze more than just high-contrast VA and refraction. Decreases in contrast sensitivity are reported to be less satisfactory with multifocal IOLs than with monofocal IOLs8,12,13. There is always some concern that the additional focal point provided by a trifocal IOL may reduce contrast sensitivity more than bifocal IOLs by splitting light into three foci9. However, our findings show that contrast sensitivity was unlikely to be more problematic with trifocal IOLs. A possible explanation is that a relatively small percentage of energy is dedicated to intermediate vision, as compared to distance and near vision14,15.
With regard to subjective visual quality, visual function questionnaires such as the Visual Function Index-14 (VF-14) and National Eye Institute Visual Function Questionnaire-39 (NEI VFQ-39) have been adopted. The scores are high for all implants, suggesting satisfactory postoperative vision in both bifocal and trifocal IOLs. Gundersen and Potvin reported that fewer participants with bifocal IOLs experienced bothersome visual disturbances1. The authors explained that more participants in the trifocal group were younger than in the bifocal group, and younger people may have relatively higher visual demands or expectations. In any case, most studies reported that any such phenomena were acceptable. It is believed that visual disturbances with trifocal IOLs are minimized due to their smooth surface16. The results also showed a high level of spectacle independence and high rates of patient satisfaction in both patient groups1,2,4, especially in the trifocal group2.
To our knowledge, no previous systematic review and meta-analysis has been applied to compare trifocal with bifocal IOLs. Considering the various choices between and rapid development in IOL designs, the present study has provided useful guidelines when choosing an IOL is an option. However, the results of this study should be interpreted in the context of several important limitations. First, all of the trials were English-language studies from Europe, so the results may not be generalized to other parts of the world. Second, two studies1,2 received grants from Alcon Laboratories (Fort Worth, TX, USA), while another study5 was funded by FineVision (Liège, Belgium). However, the data extracted from these studies did not reveal any preference for any corporate connections. Finally, the quality assessment performed showed excellent quality for all of the included nonrandomized studies, but the RCTs were of low quality, so more studies, especially high-quality and adequately powered RCTs, are warranted.
In conclusion, good evidence exists that the use of the trifocal IOLs improves distance-corrected intermediate VA without negatively impacting distance or near VA, compared to bifocal IOLs. Contrast sensitivity and subjective visual quality were heterogeneous with no clear results favoring either option.
Materials and Methods
The systematic review and meta-analysis were performed without language or date restriction and reported according to the Meta-Analysis of Observational Studies in Epidemiology (MOOSE) and Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines17,18.
Search strategy
Two reviewers (X.L. and Y.Z.) independently searched the Cochrane Central Register of Controlled Trials (CENTRAL), PubMed, EMBASE, and Web of Science databases, using the following search terms as keywords: trifocal (trifocal, three foci), bifocal (bifocal, two foci), intraocular lens, and cataract. Supplementary Data S1 shows the PubMed search process, updated through November 4, 2016. Two reviewers (X.L. and Y.Z.) then independently screened the titles and abstracts, after which potentially relevant trials were closely analyzed as full manuscripts. Disagreement between the two reviewers was resolved initially by discussion; if agreement could not be reached, a third reviewer (Z.S.) was consulted.
Eligibility criteria and outcome variables
We strove to include in this study all RCTs and prospective cohorts comparing trifocal and bifocal IOLs in which adult participants were undergoing cataract surgery and multifocal IOL implantation or refractive lens exchanges in one or both eyes. Participants with localized ocular disease like corneal opacities, macular disease, and optic neuropathies were excluded. When multiple trials were reported by the same team from the same institution, only the most complete data set was included. As a further filter, inclusion demanded that studies provide quantified data using continuous variables with means and standard deviations. Study authors were contacted to provide sufficient information when necessary; four authors were contacted and two responded1,5,6.
The primary outcomes were defined as uncorrected VA and corrected VA at near, intermediate, and far distances, defocus curves, contrast sensitivity, and subjective perception of quality of vision. The VA measurements were included in the logarithm of the minimum angle of resolution (logMAR) scale, on which lower scores indicate better vision. The defocus curve is a universally accepted measure for evaluating the range of functional vision at all distances under standard testing conditions after implantation of multifocal IOLs7. Three important defocus levels define the most important viewing distances for tasks found in different parts of daily life: 0.00 D, corresponding to distance vision; −1.50 D, corresponding to intermediate vision; and −2.50 D, corresponding to near vision7. Contrast sensitivity values of 1.5, 3, 6, 12, and 18 cycles per degree (cpd) in sine-wave mode were included in the analysis. Because contrast sensitivity data was not present in all studies and the specific questions about patients’ subjective visual quality perception differed, these outcomes could not be combined in a meta-analysis. Instead, they are reported descriptively.
Postoperative refraction was defined as a secondary outcome. We recorded postoperative spherical equivalents, sphere, and cylinder in diopters for both trifocal and bifocal groups, conducting a meta-analysis on these results.
Data collection
Using a standard form, two reviewers (X.L. and Y.Z.) independently extracted study characteristics data and outcome measures. All data collection was double- checked, with discrepancies resolved by discussion.
Assessment of study quality
The quality of RCTs was assessed using the Jadad scale19; cohort quality was assessed on the NOS20. The Jadad scale uses the three primary domains of randomization, blinding, and participant dropout. Appropriate randomization and blinding each scored two points, with total scores ranging from zero to five. Studies scoring fewer than three points were considered to be of low quality. The maximum NOS score is nine, based on the assessment of three areas: selection quality (four points maximum), comparability (two points maximum), and outcome measures (three points maximum). Higher score indicated higher study quality. The overall quality of evidence was evaluated using the GRADE working group framework.
Statistical analysis
Data was analyzed with RevMan software (version 5.3; Cochrane Collaboration, Oxford, United Kingdom). Mean differences (MDs) with 95% confidence intervals (CIs) were calculated for the continuous measures; statistical significance in the level of difference was defined as p < 0.05. Forest plots were used to present the results, with lines representing the estimates from different studies and their CIs and boxes graphically representing the weight given to each study in calculating the pooled estimate for a given outcome21.
Substantial heterogeneity was detected when I2 was >50% or the p-value for heterogeneity was <0.10. Publication bias was measured using a Begg funnel plot22. The fixed effect model was used when no heterogeneity was observed throughout the studies that were included; otherwise, the random effect model was used23,24. Sensitivity analysis was performed to determine the influence of a single article on the overall pooled analysis.
Additional Information
How to cite this article: Shen, Z. et al. Clinical comparison of patient outcomes following implantation of trifocal or bifocal intraocular lenses: a systematic review and meta-analysis. Sci. Rep. 7, 45337; doi: 10.1038/srep45337 (2017).
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Gundersen, K. G. & Potvin, R. Comparison of visual outcomes and subjective visual quality after bilateral implantation of a diffractive trifocal intraocular lens and blended implantation of apodized diffractive bifocal intraocular lenses. Clin Ophthalmol. 10, 805–811 (2016).
Jonker, S. M. et al. Comparison of a trifocal intraocular lens with a +3.0 D bifocal IOL: results of a prospective randomized clinical trial. J Cataract Refract Surg. 41, 1631–1640 (2015).
Bilbao-Calabuig, R. et al. Comparison between mix-and-match implantation of bifocal intraocular lenses and bilateral implantation of trifocal intraocular lenses. J Refract Surg. 32, 659–663 (2016).
Cochener, B. Prospective clinical comparison of patient outcomes following implantation of trifocal or bifocal intraocular lenses. J Refract Surg. 32, 146–151 (2016).
Gundersen, K. G. & Potvin, R. Comparison of visual outcomes after implantation of diffractive trifocal toric intraocular lens and a diffractive apodized bifocal toric intraocular lens. Clin Ophthalmol. 10, 455–461 (2016).
Mojzis, P., Kukuckova, L., Majerova, K., Liehneova, K. & Pinero, D. P. Comparative analysis of the visual performance after cataract surgery with implantation of a bifocal or trifocal diffractive IOL. J Refract Surgery. 30, 666–672 (2014).
Plaza-Puche, A. B. & Alio, J. L. Analysis of defocus curves of different modern multifocal intraocular lenses. Eur J Ophthalmol. 0 (2016).
Plaza-Puche, A. B., Alio, J. L., Sala, E. & Mojzis, P. Impact of low mesopic contrast sensitivity outcomes in different types of modern multifocal intraocular lenses. Euro J Ophthalmol. 0 (2016).
Carson, D., Hill, W. E., Hong, X. & Karakelle, M. Optical bench performance of AcrySof(®) IQ ReSTOR(®), AT LISA(®) tri, and FineVision(®) intraocular lenses. Clin Ophthalmol. 8, 2105–2113 (2014).
Gatinel, D. & Houbrechts, Y. Comparison of bifocal and trifocal diffractive and refractive intraocular lenses using an optical bench. J Cataract Refract Surg. 39, 1093–1099 (2013).
Cochener, B. et al. Visual and refractive outcomes after implantation of a fully diffractive trifocal lens. Clin Ophthalmol. 6, 1421–1427 (2012).
Pepose, J. S. et al. Safety and effectiveness of a new toric presbyopia-correcting posterior chamber silicone intraocular lens. J Cataract Refract Surg. 41, 295–305 (2015).
Hayashi, K., Masumoto, M. & Takimoto, M. Comparison of visual and refractive outcomes after bilateral implantation of toric intraocular lenses with or without a multifocal component. J Cataract Refract Surg. 41, 73–83 (2015).
Gatinel, D., Pagnoulle, C., Houbrechts, Y. & Gobin, L. Design and qualification of a diffractive trifocal optical profile for intraocular lenses. J Cataract Refract Surg. 37, 2060–2067 (2011).
Vryghem, J. C. & Heireman, S. Visual performance after the implantation of a new trifocal intraocular lens. Clin Ophthalmol. 7, 1957–1965 (2013).
Marques, E. F. & Ferreira, T. B. Comparison of visual outcomes of 2 diffractive trifocal intraocular lenses. J Cataract Refract Surg. 41, 354–363 (2015).
Moher, D., Liberati, A. & Tetzlaff, J. Group DGAP. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 151, 264–269, W64 (2009).
Stroup, D. F., Berlin, J. A. & Morton, S. C. Meta-analysis of observational studies in epidemiology: a proposal for reporting. JAMA. 283, 2008–2012 (2000).
Jadad, A. R., Moore, R. A. & Carroll, D. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials. 17, 1–12 (1996).
Wells, G. A. et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomized studies in meta-analysis. Available: http://www.ohri.ca/programs/clinical_epidemiology/oxford.htm [2017 Jan 19].
Cochener, B., Lafuma, A., Khoshnood, B., Courouve, L. & Berdeaux, G. Comparison of outcomes with multifocal intraocular lenses: a meta-analysis. Clin Ophthalmol. 5, 45–56 (2011).
Begg, C. B. & Mazumdar, M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 50, 1088–1101 (1994).
Higgins, J. P., Thompson, S. G., Deeks, J. J. & Altman, D. G. Measuring inconsistency in meta-analyses. BMJ. 327, 557–560 (2003).
DerSimonian, R. & Kacker, R. Random-effects model for meta-analysis of clinical trials: an update. Contemp Clin Trials. 28, 105–114 (2007).
Acknowledgements
We thank Dr. Xiaoning Yu for providing guidance and support. And this work was supported by the Program of National Natural Science Foundation of China (Nos 81570822 and 81500704), the Zhejiang Key Laboratory Fund of China (No. 2011E10006), the Zhejiang Province Key Research and Development Program (No. 2015C03042), and the Zhejiang Provincial Natural Science Foundation of China (No. LQ15H120002). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
Z.S. and K.Y. conceived and designed the study. X.L. and Y.Z. performed literature searches and data collection. Y.L. and J.Y. conducted statistical analysis. Z.S. wrote the manuscript and K.Y. revised it.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Supplementary information
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Shen, Z., Lin, Y., Zhu, Y. et al. Clinical comparison of patient outcomes following implantation of trifocal or bifocal intraocular lenses: a systematic review and meta-analysis. Sci Rep 7, 45337 (2017). https://doi.org/10.1038/srep45337
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep45337
- Springer Nature Limited
This article is cited by
-
Effect of Long-Acting Diquafosol Sodium on Astigmatism Measurement Repeatability in Preoperative Cataract Cases with Dry Eyes: A Multicenter Prospective Study
Ophthalmology and Therapy (2024)
-
Cataract surgery with new monofocal intraocular lens enhanced for intermediate vision and standard monofocal intraocular lens for retinal disorder
International Ophthalmology (2024)
-
Effect of decentration and tilt on the in vitro optical quality of monofocal and trifocal intraocular lenses
Graefe's Archive for Clinical and Experimental Ophthalmology (2024)
-
Influence of implantation of diffractive trifocal intraocular lenses on standard automated perimetry
BMC Ophthalmology (2022)
-
Depth of field and visual performance after implantation of a new hydrophobic trifocal intraocular lens
BMC Ophthalmology (2022)