Abstract
Background
More accurate estimation of the general height of the visual field may improve our ability to detect and monitor progression of diseases affecting visual function such as glaucoma. General height (GH) can be affected by factors such as cataracts, pupillary miosis, refractive error, and learning and fatigue effects. The conventional GH index, consisting of subtracting the 85th largest value from the total-deviation map, has been shown to overestimate the height in patients with moderate and advanced glaucoma. We aimed at developing an improved estimator for general height based on ranking of total-deviation values that are within normal limits (GHr).
Methods
Two datasets were used for the comparisons between GH and GHr estimates: one with 369 visual fields for 102 controls, and another with 500 visual fields for 124 patients. For controls, we compared the distributions of mean of total deviation (MD) and of mean of pattern deviation (MPD) derived from both the GH and the GHr estimates. For patients, we assessed agreement between both estimates and between pairs of consecutive visits. We also compared linear fits in progression analyses. All data were collected with 24–2 SITA Standard.
Results
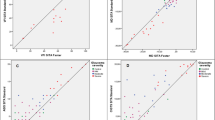
For control subjects and patients with MD above −5.5 dB, estimates with the GHr estimator were not significantly different than with the GH estimator. For patients with glaucoma with MD below −5.5 dB, as MD became more negative the GH estimates were increasingly greater than GHr estimates. For patients with glaucoma, test–retest variability was lower with the GHr estimator: between visits agreement was better for GHr estimates than for GH estimates (SD of 0.8 dB versus 1.5 dB; p < 0.0001). Linear-regression analysis fitted better estimates obtained with the GHr estimator. Root mean square error for GHr was 0.4 dB; lower than the 0.8 dB for GH (p < 0.0001).
Conclusions
The novel GHr estimator is very different from the conventional GH estimator, has more solid foundations, and better statistical properties. Nevertheless, it is not always better than the GH estimator, in particular if no focal loss is present. Pattern-deviation maps obtained with GHr reduce systematic underestimation of glaucomatous damage.




Similar content being viewed by others
References
Wild JM, Dengler-Harles M, Searle AE, O’Neill EC, Crews SJ (1989) The influence of the learning effect on automated perimetry in patients with suspected glaucoma. Acta Ophthalmol 67:537–545
Heijl A, Lindgren G, Olsson J (1989) The effect of perimetric experience in normal subjects. Arch Ophthalmol 107:81–86
Marra G, Flammer J (1991) The learning and fatigue effect in automated perimetry. Graefes Arch Clin Exp Ophthalmol 229:501–504
Frisén L (1989) Perimetric variability: importance of criterion level. Doc Ophthalmol 70:323–330
Greve EL (1980) Visual fields, glaucoma and cataract. Doc Ophthalmol Proc Ser 22:79–88
Guthauser U, Flammer J (1988) Quantifying visual field damage caused by cataract. Am J Ophthalmol 106:480–484
Heijl A (1989) Lack of diffuse loss of differential light sensitivity in early glaucoma. Acta Ophthalmol 67:353–360
Drance SM (1969) The early field defects in glaucoma. Invest Ophthalmol 8:84–91
Flammer J (1985) Psychophysics in glaucoma. A modified concept of the disease. In: Greve EL, Leydhecker W, Raitta C (eds) Second European Glaucoma Symposium, Helsinki 1984. Dr W Junk, Dordrecht, pp 11–17
Chauhan BC, LeBlanc RP, Shaw AM, Chan AB, McCormick TA (1997) Repeatable diffuse visual field loss in open-angle glaucoma. Ophthalmology 104:532–538
Heijl A, Lindgren G, Olsson J (1987) A package for the statistical analysis of visual fields. Doc Ophthalmol Proc Ser 49:153–168
Heijl A, Lindgren G, Olsson J, Åsman P (1989) Visual field interpretation with empiric probability maps. Arch Ophthalmol 107:204–208. doi:10.1001/archopht.1989.01070010210024
Langerhorst CT (1988) Automated perimetry in glaucoma: fluctuation behavior and general and local reduction of sensitivity. Kugler & Ghedini, Amsterdam
Langerhorst CT, Van den Berg TJTP, Greve EL (1989) Is there general reduction of sensitivity in glaucoma? Int Ophthalmol 13:31–35
Funkhouser AT (1991) A new diffuse loss index for estimating general glaucomatous visual field depression. Doc Ophthalmol 77:57–72. doi:10.1007/BF00154878
Funkhouser A, Flammer J, Fankhauser F, Hirsbrunner H-P (1992) A comparison of five methods for estimating general glaucomatous visual field depression. Graefes Arch Clin Exp Ophthalmol 230:101–106
Vingrys AJ, Zele AJ (2005) Robust indices of clinical data: meaningless means. Invest Ophthalmol Vis Sci 46:4353–4357
Gonzalez de la Rosa M, Gonzalez-Hernandez M, Diaz-Aleman T (2009) Linear regression analysis of the cumulative defect curve by sectors and other criteria of glaucomatous visual field progression. Eur J Ophthalmol 19:416–424
Åsman P, Heijl A (1992) Glaucoma hemifield test. Automated visual field evaluation. Arch Ophthalmol 110:812–819
Åsman P, Wild JM, Heijl A (2004) Appearance of the pattern deviation map as a function of change in area of localized field loss. Invest Ophthalmol Vis Sci 45:3099–3106
Artes PH, Nicolela MT, LeBlanc RP, Chauhan BC (2005) Visual field progression in glaucoma: total versus pattern deviation analyses. Invest Ophthalmol Vis Sci 46:4600–4606
Bebie H, Flammer J, Bebie TH (1989) The cumulative defect curve: separation of local and diffuse components of visual field damage. Graefes Arch Clin Exp Ophthalmol 227:9–12. doi:10.1007/BF02169816
Marín-Franch I, Swanson WH (2013) The visualFields package: A tool for analysis and visualization of visual fields. J Vis 13(4):1–12. doi:10.1167/13.4.10
R Core Team (2013) R: A language and environment for statistical computing. R Foundation for Statistical Computing,, Vienna, Austria. URL http://www.R-project.org/. Accessed 3 Mar 2014
Marín-Franch I (2013) visualFields: Statistical methods for visual fields, version 0.4
Blumenthal EZ, Sapir-Pichhadze R (2003) Misleading statistical calculations in far-advanced glaucomatous visual field loss. Ophthalmology 110:196–200
Bengtsson B, Heijl A (2008) A visual field index for calculation of glaucoma rate of progression. Am J Ophthalmol 145:343–353. doi:10.1016/j.ajo.2007.09.038
Cleveland WS (1993) Visualizing data. Hobart Press, Summit, NJ
Acknowledgements
We thank Mitchell W Dul for useful discussions and for providing data and clinical evaluation of healthy controls and patients with glaucoma. This work was supported by NIH grant R01EY007716.
None of the authors have conflicts of interests
Author information
Authors and Affiliations
Corresponding author
Appendixes
Appendixes
Appendix A: review of TD-rank curves
Figure 5 shows three TD maps obtained with visualFields for the 24–2 visual field test grid and SITA Standard. The TD maps correspond to a healthy eye (Fig. 5a), a glaucomatous eye (Fig. 5b), and (Fig. 5c) the healthy eye in Fig. 5a with artificial damage added to the lower hemifield. The TD-rank curves for the TD maps in Fig. 5a, b are shown in Fig. 5d. For its display, the TD values in Fig. 5a, b were ranked and plotted against their rank position; this is the TD-rank curve — also known as the Bebié cumulative defect curve [22]. The TD-rank curve for the artificial visual field in Fig. 5c is not shown to preserve clarity.
TD maps and TD-rank curves. Three TD maps (consisting of TD values on top of circles with corresponding color-coded probability categories for a a healthy eye and b a glaucomatous eye obtained using the 24–2 visual field test grid and SITA Standard. The visual field in c is the same as for the healthy eye in a after artificially adding a lower-field defect (sensitivities equal to zero at all locations). In d, the TD-rank curves are shown for the visual fields in a and b, but not c for clarity. The solid curve shows the mean normal TD-rank curve. The vertical arrows denote the TD at rank positions 7 and 14. The dashed curves in c and d are the 95 % confidence limits for the normal TD-rank curve. The color codes at each percentile category in the TD probability maps and the empirical TD-rank curves are shown in the bottom middle
The TD-rank curves have been used to derive algorithms for the estimation of the height of the hill of vision [15, 16, 18], some defined from direct visual inspection [15]. From a visual inspection of the TD-rank curve for the glaucomatous visual field in Fig 5b, we see that part of the curve is roughly parallel with the mean normal TD-rank curve (black solid curve). The difference between TD-rank curves in the portion that they go in parallel may be taken as an estimate of the difference in height from mean normal (many times called diffuse loss when height is lower than the age-corrected mean normal height). At around rank position 34, the curve is no longer parallel to the mean normal one and the distance from mean normal of the remaining 18 points is greater. We may then “conclude” that the remaining 18 locations had focal loss.
Appendix B: the general sensitivity estimator
The key to the estimation of the height of the hill of vision is the reconstruction of the “normal part” of the TD-rank curve for patients with a partially damaged visual field. Here, we propose to select only the TD values that are within normal limits and infer what is the most likely rank position they were in before the visual field was damaged at all. To illustrate why the rank positions need to be recalculated, an artificial visual field was generated (see Fig. 5c) from the visual field for a healthy subject (see Fig. 5a). The artificial visual field in Fig. 5c was obtained by assigning sensitivities of 0 dB to all locations in the lower hemifield of the healthy visual field in Fig. 5c. Similar artificial visual fields have been analyzed elsewhere [20].
For the healthy visual field in Fig. 5a, the average of the 52 TD values is 0.0 dB, and so is the average of the mean normal TD values (black curve in Fig. 5d). That is, the height of the hill of vision for this visual field is the same as that for the age-corrected mean normal hill of vision. If we estimated the height with the GH estimator [11, 20] we would obtain a height of 0.2 dB above mean normal: 2.0 dB for the seventh largest TD value in the visual field in Fig. 5a minus 1.8 dB for the seventh largest TD value from the mean normal visual field (the value of the black curve in Fig. 5d marked with a vertical arrow).
Consider the artificial visual field in Fig. 5c. The GH estimator for the artificially damaged visual field is 0.7 dB. That is 1.1 dB below mean normal height, an overestimation as the true height of the visual field was equal to mean normal. Since rank positions change as defects appear, it makes sense to assume that the TD value in rank 7 in Fig. 5c was actually around rank 14 before half of the visual field in Fig. 5c became blind. If we take rank 14 of the mean normal visual field as reference (1.1 dB, marked with an arrow in Fig. 5d), then we would estimate the height as 0.3 dB below mean normal, which is a closer estimate to the true height than the GH estimate. The GHr estimator that we introduce here is based on the re-calculation of TD rank positions of all within normal limits (above percentile 5 and below percentile 95). To continue with our example in Fig. 5c, the number n of TD values within normal limits is 23.
Computationally, a unique solution to the re-calculation of the rank positions can be achieved by meeting two conditions. First, the spacing between recalculated rank positions must be equal and, second, the mid point of the recalculated ranks must equal the mid point of the ranks for the mean normal TD rank. For the 24–2 visual field test grid, for which there are N = 52 TD values (after excluding the blind spot and the location above it), such a mid point is 53/2 = 26.5. The distance between recalculated ranks must be (N – 1)/(n + 1), so that the recalculated rank positions r i , for i = 1, …, n, are
where c is a constant obtained from the second condition that the mid point of the recalculated ranks must equal the mid point of the mean normal TD rank curve, thus,
Following this approach, for our example with a blind lower hemifield, the recalculated rank positions would be r i = (17/8) i + 1. The value of the mean normal TD-rank curve at those (non-integer) locations can be obtained by linear interpolation. The height estimated with the GHr estimator was 0.1 dB above mean normal, the closest estimate in this example.
Rights and permissions
About this article
Cite this article
Marín-Franch, I., Swanson, W.H. & Malinovsky, V.E. A novel strategy for the estimation of the general height of the visual field in patients with glaucoma. Graefes Arch Clin Exp Ophthalmol 252, 801–809 (2014). https://doi.org/10.1007/s00417-014-2602-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-014-2602-x