Abstract
Purpose
To evaluate B-scan echography for the assessment of lacrimal sac (LS) in pediatric epiphora secondary to congenital nasolacrimal duct obstruction (CNLDO), and to verify its predictive role in functional efficacy of nasolacrimal duct probing.
Patients and Methods
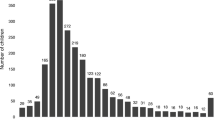
Thirty-nine eyes of 23 consecutive children, treated with a single probing for persistent CNLDO-related epiphora, were retrospectively studied. These cases were investigated both collectively and considering two sub-groups: group A (ten patients [20 eyes] ≤13 months) and group B (13 patients [19 eyes] >13 months. Fluorescein dye disappearance test at 10 minutes (FDDT-10) and ultrasound examination of LS were performed before and after probing. An echographic LS scoring system (grade 0 = no LS enlargement; grade 1 = slight longitudinal LS enlargement; grade 2 = longitudinal and slight transverse LS enlargement; grade 3 = marked longitudinal and transverse LS enlargement) was introduced as a predictor of probing efficacy, estimating FDDT-10 modification between pre- and post-operative checks.
Results
Echographic LS evaluation was easily practicable without sedation. In the total cluster and in both age sub-groups, post-probing FDDT-10 decreased with respect to pre-probing value (p < 0.001). Post-probing LS score improved with respect to pre-probing check within the total cluster and group A (p < 0.05). Strong correlation between pre-probing LS alteration and functional probing failure was present in each studied cluster (all p values <0.0001). Within group B, a greater gain of post-probing FDDT-10 was more frequent in patients with a better pre-probing LS score, as well as in younger children (both p values <0.0001).
Conclusions
In children with CNLDO-related epiphora, B-scan echography of the LS can represent a reliable and useful examination for a better understanding of the functional prognosis after probing treatment.



Similar content being viewed by others
References
MacEwen CJ, Young JD (1991) Epiphora during the first year of life. Eye 5:596–600
Robb RM (2001) Congenital nasolacrimal duct obstruction. Ophthalmol Clin North Am 14:443–446. doi:10.1016/S0896-1549(05)70242-X
MacEwen CJ (2006) Congenital nasolacrimal duct obstruction. Compr Ophthalmol Update 7:79–87
Pashby RC, Hurwitz JJ (1996) Pediatric lacrimal disease. In: Hurwitz JJ (ed) The lacrimal system. Lippincott-Raven, Philadelphia, pp 237–244
Piest KL, Katowitz JA (1991) Treatment of congenital nasolacrimal duct obstruction. Ophthalmol Clin North Am 4:201–209
Nucci P, Capoferri C, Alfarano R, Brancato R (1989) Conservative management of congenital nasolacrimal duct obstruction. J Pediatr Ophthalmol Strabismus 26:39–43
Young JD, MacEwen CJ, Ogston SA (1996) Congenital nasolacrimal duct obstruction in the second year of life: a multicentre trial of management. Eye 10:485–491
Schellini SA, Ferreira Ribeiro SC, Jaqueta E, Padovani CR, Padovani CR (2007) Spontaneous resolution in congenital nasolacrimal obstruction after 12 months. Semin Ophthalmol 22:71–74. doi:10.1080/08820530701331784
Young JD, MacEwen CJ (1997) Managing congenital lacrimal obstruction in general practice. BMJ 315:293–296
Pediatric Eye Disease Investigator GroupRepka MX, Chandler DL, Beck RW, Crouch ER 3rd, Donahue S, Holmes JM, Lee K, Melia M, Quinn GE, Sala NA, Schloff S, Silbert DI, Wallace DK (2008) Primary treatment of nasolacrimal duct obstruction with probing in children younger than 4 years. Ophthalmology 115:577–584
el-Mansoury J, Calhoun JH, Nelson LB, Harley RD (1986) Results of late probing for congenital nasolacrimal duct obstruction. Ophthalmology 93:1052–1054
Katowitz JA, Welsh MG (1987) Timing of initial probing and irrigation in congenital nasolacrimal duct obstruction. Ophthalmology 94:698–705
Sturrock SM, MacEwen CJ, Young JD (1994) Long term results after probing for congenital nasolacrimal duct obstruction. Br J Ophthalmol 78:892–894. doi:10.1136/bjo.78.12.892
Paul TO, Shepard R (1994) Congenital nasolacrimal duct obstruction: natural history and the timing of optimal intervention. J Pediatr Ophthalmol Strabismus 31:362–367
Zwaan J (1997) Treatment of congenital nasolacrimal duct obstruction before and after the age of 1 year. Ophthalmic Surg Lasers 28:932–936
Kushner BJ (1998) The management of nasolacrimal duct obstruction in children between 18 months and 4 years old. J AAPOS 2:57–60. doi:10.1016/S1091-8531(98)90112-4
Robb RM (1998) Success rates of nasolacrimal duct probing at time intervals after 1 year of age. Ophthalmology 105:1307–1310. doi:10.1016/S0161-6420(98)97038-5
Mannor GE, Rose GE, Frimpong-Ansah K, Ezra E (1999) Factors affecting the success of nasolacrimal duct probing for congenital nasolacrimal duct obstruction. Am J Ophthalmol 127:616–617. doi:10.1016/S0002-9394(98)00432-2
Honavar S, Vasudha EP, Rao GN (2000) Outcome of probing for congenital nasolacrimal duct obstruction in older children. Am J Ophthalmol 130:42–48. doi:10.1016/S0002-9394(00)00388-3
Kashkouli MB, Kassaee A, Tabatabaee Z (2002) Initial nasolacrimal duct probing in children under age 5: cure rate and factors affecting success. J AAPOS 6:360–363. doi:10.1067/mpa.2002.129041
Maheshwari R (2005) Results of probing for congenital nasolacrimal duct obstruction in children older than 13 months of age. Indian J Ophthalmol 53:49–51
Casady DR, Meyer DR, Simon JW, Stasior GO, Zobal-Ratner JL (2006) Stepwise treatment paradigm for congenital nasolacrimal duct obstruction. Ophthal Plast Reconstr Surg 22:243–247. doi:10.1097/01.iop.0000225750.25592.7f
Wallace EJ, Cox A, White P, MacEwen CJ (2006) Endoscopic-assisted probing for congenital nasolacrimal duct obstruction. Eye 20:998–1003. doi:10.1038/sj.eye.6702049
Zilelioğlu G, Hoşal BM (2007) The results of late probing in congenital nasolacrimal duct obstruction. Orbit 26:1–3. doi:10.1080/01676830600972807
Kashkouli MB, Beigi B, Parvaresh MM, Kassaee A, Tabatabaee Z (2003) Late and very late initial probing for congenital nasolacrimal duct obstruction: what is the cause of failure? Br J Ophthalmol 87:1151–1153. doi:10.1136/bjo.87.9.1151
Wobig JL (1985) Lacrimal probing complications. Ophthal Plast Reconstr Surg 1:75–76. doi:10.1097/00002341-198501000-00013
Milder B (1980) Complications in lacrimal surgery. In: Waltman SR, Krupin T (eds) Complications in ophthalmic surgery. Lippincott, New York, pp 233–251
Baker JD (1985) Treatment of congenital nasolacrimal system obstruction. J Pediatr Ophthalmol Strabismus 22:34–36
MacEwen CJ, Young JD, Barras CW, Ram B, White PS (2001) Value of nasal endoscopy in the diagnosis and management of children with congenital epiphora. Br J Ophthalmol 85:314–318. doi:10.1136/bjo.85.3.314
Petersen RA, Robb RM (1978) The natural course of congenital obstruction of the nasolacrimal duct. J Pediatr Ophthalmol Strabismus 15:246–250
Tost F, Bruder R, Clemens S (2002) 20-MHz ultrasound of presaccular lacrimal ducts. Ophthalmologe 99:25–28. doi:10.1159/000071571
Ostendorf M, Tost F (2003) Imaging the lacrimal canaliculus with 20-MHz ultrasonography: a normal diagnosis (Part 1). J Fr Ophtalmol 26:1031–1034
Tost F, Bruder R, Ostendorf M (2003) High-frequency ultrasonography applied to disorders of the lacrimal canaliculi (Part 2). J Fr Ophtalmol 26:1035–1038
Hewick SA, Fairhead AC, Culy JC, Atta HR (2004) A comparison of 10 MHz and 20 MHz ultrasound probes in imaging the eye and orbit. Br J Ophthalmol 88:551–555. doi:10.1136/bjo.2003.028126
Stupp T, Pavlidis M, Busse H, Thanos S (2004) Presurgical and postsurgical ultrasound assessment of lacrimal drainage dysfunction. Am J Ophthalmol 138:764–771. doi:10.1016/j.ajo.2004.06.018
MacEwen CJ, Young JD (1991) The fluorescein disappearance test (FDT): an evaluation of its use in infants. J Pediatr Ophthalmol Strabismus 28:302–305
Bowyer JD, Holroyd C, Chandna A (2001) The use of the fluorescein disappearance test in the management of childhood epiphora. Orbit 20:181–187. doi:10.1076/orbi.20.3.181.2620
Zappia RJ, Milder B (1972) Lacrimal drainage function: 2. The fluorescein dye disappearance test. Am J Ophthalmol 74:160–162
Dutton JJ (1989) Standardized echography in the diagnosis of lacrimal drainage dysfunction. Arch Ophthalmol 107:1010–1012
Jedrzynski MS, Bullock JD (1994) Lacrimal ultrasonography. Ophthal Plast Reconstr Surg 10:114–120. doi:10.1097/00002341-199406000-00008
Korchmaros I, Szalay E (1978) Cannula-probing combined with nasal procedure for dacryocystitis neonatorum. Acta Ophthalmol (Copenh) 56:357–362
Singh Bhinder G, Singh Bhinder H (2004) Repeated probing results in the treatment of congenital nasolacrimal duct obstruction. Eur J Ophthalmol 14:185–192
O’Donnell BA, Adenis JP, Linberg JV, Rose GE, Sullivan TJ, Wobig JL (2001) The failed probing. Clin Experiment Ophthalmol 29:276–280. doi:10.1046/j.1442-9071.2001.00433.x
Marr JE, Drake-Lee A, Willshaw HE (2005) Management of childhood epiphora. Br J Ophthalmol 89:1123–1126. doi:10.1136/bjo.2005.069286
Kassoff J, Meyer DR (1995) Early office-based vs late hospital-based nasolacrimal duct probing. A clinical decision analysis. Arch Ophthalmol 113:1168–1171
Becker BB (1992) Tricompartment model of the lacrimal pump mechanism. Ophthalmology 99:1139–1145
Pavlidis M, Stupp T, Grenzebach U, Busse H, Thanos S (2005) Ultrasonic visualization of the effect of blinking on the lacrimal pump mechanism. Graefes Arch Clin Exp Ophthalmol 243:228–234. doi:10.1007/s00417-004-1033-5
Acknowledgements
We thank Ms. Graziella Ferraresi for her logistic support, and the parents of the babies for their cooperation.
Financial Support and/or Relationship
None.
Conflict of Interest
No conflicting relationship exists for any author.
Author information
Authors and Affiliations
Corresponding author
Additional information
The authors have full control of all primary data, and they agree to allow Graefe’s Archive for Clinical and Experimental Ophthalmology to review their data upon request.
Rights and permissions
About this article
Cite this article
Steindler, P., Mantovani, E., Incorvaia, C. et al. Efficacy of probing for children with congenital nasolacrimal duct obstruction: a retrospective study using fluorescein dye disappearance test and lacrimal sac echography. Graefes Arch Clin Exp Ophthalmol 247, 837–846 (2009). https://doi.org/10.1007/s00417-008-1022-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-008-1022-1