Abstract
Background
Pediatric nasolacrimal duct obstruction (PNDO) requires therapeutic intervention after conservative procedures failed. As resilient treatment guidelines for the treatment are missing, the aim of this study was to evaluate the advantages of two different intervention techniques in children with PNDO.
Methods
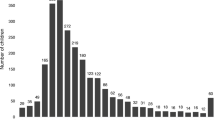
Between January, 2006 and June, 2014, 233 children (0-208 months) were treated either with conventional probing by ophthalmologists only (Group I) or with endonasal endoscopic interdisciplinary approach (Group II). The clinical outcome was analyzed.
Results
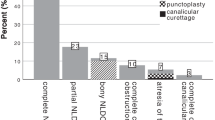
The overall success rate of Group I was 93.4% compared to 98.4% of Group II (P<0.05). 50% of all interventions (n=62) of Group II required further surgical procedures in addition to probing/irrigation, particularly with regard to children <6 and >24 months.
Conclusions
Endoscopic control in treatment of PNDO allows exact identification of the stenosis and appropriate surgical intervention with an improved clinical outcome. Endonasal endoscopic surgical techniques should be the standard PNDO treatment.
Similar content being viewed by others
References
MacEwen CJ, Young JD. Epiphora during the first year of life. Eye 1991;5:596–600.
Pediatric Eye Disease Investigator Group. Resolution of congenital nasolacrimal duct obstruction with nonsurgical management. Arch Opthalmol 2012;130:730–734.
Young JD, MacEwen CJ, Ogston SA. Congenital nasolacrimal duct obstruction in the second year of life: a multicentre trial of management. Eye 1996;10:485–491.
Dotan G, Nelson LB. Congenital nasolacrimal duct obstruction: common management policies among pediatric ophthalmologists. J Pediatr Ophthalmol Strabismus 2015;52:14–19.
Miller AM, Chandler DL, Repka MX, Hoover DL, Lee KA, Melia M, et al. Office probing for treatment of nasolacrimal duct obstruction in infants. J AAPOS 2014;18:26–30.
Weber R, Draf W, Kolb P. Endonasal microsurgical treatment of lacrimal duct stenoses. Indications, technique and results. HNO 1993;41:11–18. [In German]
Horn IS, Tittmann M, Fischer M, Otto M, Dietz A, Mozet C. Endonasal nasolacrimal duct surgery: a comparative study of two techniques. Eur Arch Otorhinolaryngol 2014;271:1923–1931.
Mozet C, Horn IS, Otto M, Dietz A. Nasolacrimal duct obstruction in children. Children and Adolescents Medicine 2013;13:107–114. [In German]
Pediatric Eye Disease Investigator Group. A randomized trial comparing the cost-effectiveness of 2 approaches for treating unilateral nasolacrimal duct obstruction. Arch Ophthalmol 2012;130:1525–1533.
Cakmak SS, Yildirim M, Sakalar YB, Keklikci U, Alakus F. Is it necessary to accompany probing with endoscopy in cases of congenital nasolacrimal canal obstruction? Int J Pediatr Otorhinolaryngol 2010;74:1013–1015.
Paul TO, Shepherd R. Congenital nasolacrimal duct obstruction: natural history and the timing of optimal intervention. J Pediatr Ophthalmol Strabismus 1994;31:362–367.
Schnall BM. Pediatric nasolacrimal duct obstruction. Curr Opin Ophthalmol 2013;24:421–424.
Wallace EJ, Cox A, White P, MacEwen CJ. Endoscopic-assisted probing for congenital nasolacrimal duct obstruction. Eye 2006;20:998–1003.
Kouri AS, Tsakanikos M, Linardos E, Nikolaidou G, Psarommatis I. Results of endoscopic assisted probing for congenital nasolacrimal duct obstruction in older children. Int J Pediatr Otorhinolaryngol 2008;72:891–896.
Kominek P, Cervenka S, Matousek P, Pniak T, Zelenik K. Primary pediatric endonasal dacryocystorhinostomy-a review of 58 procedures. Int J Pediatr Otorhinolaryngol 2010;74:661–664.
Saeed BM, Tawalbeh M. Pediatric endoscopic DCR: the outcome in 50 patients. Indian J Otolaryngol Head Neck Surg 2014;66:276–280.
Author information
Authors and Affiliations
Corresponding author
Additional information
Funding: None.
Ethical approval: The study was performed in accordance with the Declaration of Helsinki. Informed consent was obtained from all patients prior to surgery.
Competing interest: The authors have no conflicts of interest to declare.
Contributors: Fischer M and Mozet C ideated the study, analyzed the data, and wrote the paper. Horn IS and Pirlich M collected and analyzed the data, and revised the paper. Otto M and Dietz A revised the paper.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Fischer, M., Horn, IS., Otto, M. et al. Pediatric nasolacrimal duct obstruction-benefit of a combined therapeutic approach. World J Pediatr 13, 427–432 (2017). https://doi.org/10.1007/s12519-017-0041-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12519-017-0041-6