Abstract
Background
Whether specific imaging aspects can be used to identify cryptogenic stroke (CS) patients with high risk of underlying atrial fibrillation (AF) remains unclear. The purpose of this study was to evaluate brain-imaging features in CS patients and their utility as AF predictors.
Methods
The Nordic Atrial Fibrillation and Stroke study was a prospective observational study of CS and transient ischemic attack patients undergoing 12-month cardiac-rhythm monitoring, biomarker and clinical assessments. In this imaging sub-study, brain magnetic resonance imaging and computed tomography scans from 106 patients were assessed for acute and chronic ischemic lesions in relation to AF occurrence and included in a score to predict AF. Receiver operating characteristics (ROC) curve was used to evaluate the discriminative ability of the score and for its dichotomization for predictive model.
Results
Age, periventricular white-matter hyperintensities (PVWMH), acute lesion size, and vessel occlusion were significantly associated with AF. Acute and chronic cortical infarcts as well as chronic cerebellar infarcts were numerically more frequent in the AF group than the non-AF group. A score consisting of six features (0–6 points) was proposed (age ≥ 65 years, chronic cortical or cerebellar lesions, acute cortical lesions, PVWMH ≥ 2 in Fazekas scale, vessel occlusion, and acute lesion size ≥ 10 mm). Area under ROC curve was 0.735 and a score of ≥ 3 points was a predictor of AF.
Conclusions
The suggested score was shown to identify CS patients with an increased risk of underlying AF.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Brain imaging findings are key elements in stroke diagnostics assessing the stroke etiology [1, 2]. Recognition of specific patterns and characteristics of ischemic lesions suggesting an embolic origin from atrial fibrillation (AF) would be beneficial for patients with cryptogenic stroke (CS). Large proportion of patients have underlying paroxysmal AF [3] and such recognition would have therapeutical implications. However, AF is difficult to uncover by standard follow-up after stroke. While the use of insertable cardiac monitors (ICMs) has been proven to be the most effective method for AF detection [4], their use is still not common in CS diagnostics. Establishing specific imaging criteria could therefore be helpful to select patients for prolonged cardiac-rhythm monitoring with ICMs. Several imaging characteristics have been demonstrated to be associated with AF such as acute cortical lesions [5], larger lesions [6], and lesions affecting multiple arterial territories [7]. Notwithstanding, studies with prolonged cardiac-rhythm monitoring showed mixed results and they focused mainly on acute lesions, while chronic lesions and white-matter hyperintensities (WMH) assessment was much less frequent.
The purpose of this study was to evaluate whether acute and chronic imaging features were associated with AF detected by ICMs during 12 months of continuous cardiac-rhythm monitoring in patients with CS, and whether a scoring system based on imaging and clinical findings could be used as a predictor of underlying AF.
Methods
The Nordic Atrial Fibrillation and Stroke (NOR-FIB) study was a prospective observational study of AF incidence in CS and cryptogenic transient ischemic attack (TIA) patients observed with ICMs for 12 months, performed from January 2017 to September 2021. In this single-center retrospective analysis, analyzed data were collected from patients included at one of the participating centers, Østfold Hospital Trust. Eligible patients with confirmed acute ischemia underwent a diagnostic work-up as depicted in Fig. 1 to conclude with CS or cryptogenic TIA. TIA and stroke diagnoses were used to describe the clinical presentations of the acute neurological symptoms defined as the resolution of symptoms within 24 h for TIA and the persistence of symptoms beyond 24 h for stroke. This time based definition was used to see whether patients with AF had higher tendency towards TIA and rapid resolution of symptoms than clinical stroke patients. This could address whether there are differences in the stability of embolus between AF patients and the rest of the cohort. In short, all patients including TIA patients had an acute lesion on cerebral imaging, and underwent diagnostic investigations containing general blood samples, 12-lead ECG, minimum of 24-h Holter monitoring, transthoracic echocardiography, transoesophageal echocardiography in patients ≤ 65 years of age to exclude shunting mainly from patent foramen ovale (PFO), ultrasound and computed tomography or magnetic resonance angiography to evaluate extra- and intracranial arteries, and thrombophilia screening in patients < 50 years of age. The study design and rationale have been published earlier [8] as well as the data comprising main results and ECG evaluation [9], blood biomarkers [10], and other possible underlying causes of CS beside AF after completion of one year of cardiac-rhythm monitoring [11]. CS or cryptogenic TIA were defined as an acute ischemic stroke without a determined etiology despite a thorough protocolled evaluation excluding patients with a definite etiology and source of embolism such as PFO or valvular diseases and those without adherence to participation in the study [8].
Patient flow-chart of the Nordic Atrial Fibrillation and Stroke study. CTA computed tomography angiography, ECG electrocardiography, MRA magnetic resonance angiography, TEE transoesophageal echocardiography, TTE transthoracic echocardiography [Modified from Ratajczak-Tretel et al. 2019 [8]]
Cardiac-rhythm monitoring
Patients included in the study had a Medtronic Reveal LINQ™ inserted within 14 days after index stroke. They obtained a CareLink monitor that enabled transmission of stored data to the CareLink Network. Two cardiologists and two neurologists (Corelab) were responsible for a weekly screening of transmitted data to CareLink for potential AF or atrial flutter (Fig. 1). Weekly evaluation secured an early AF detection and triggered a change of secondary prevention from antiplatelet agents to anticoagulants. A minimum of 2-min episode was required to establish an AF diagnosis based on the device-detection algorithm.
Imaging analysis
As a part of the diagnostic protocol of the study, all included patients were subjected to cerebral imaging with computed tomography (CT) and/or 1.5 or 3 Tesla magnetic resonance imaging (MRI) as well as computed tomography angiography (CTA) of extra- and intracranial arteries within 14 days from symptom onset (Fig. 1). CT perfusion was done in a subset of patients. Brain CT was done routinely as the initial-imaging strategy whereas MRI was done as follow-up imaging. Brain CT-images were reconstructed to 3 mm slice thickness in the transversal plane. CTA images were reconstructed to 0.9 mm axial slices (coronal and sagittal images were made available with multiplane reformatting). For MRI the slice thickness was 4 or 5 mm according to the type of the machine and software version that was used. The following MRI sequences were obtained: Axial T2, sagittal T1, sagittal 3D FLAIR (three planes made available with multiplane reformatting), and axial diffusion. All examinations were evaluated by the same senior neuroradiologist (D.O.S.) who was blinded to clinical data and other radiological examinations. The IntelliSpace Portal v. 10 (Phillips, Eindhoven, the Netherlands) was used for the storage and the evaluation of images. MRI was chosen as the primary imaging modality for the analysis. If MRI was missing, CT and / or control CT were assessed. Acute, subacute, and chronic lesions together with the extent of white-matter lesions were recorded. Acute and subacute lesions on CT were defined as areas of hypoattenuation with associated parenchymal swelling [12]. On MRI, acute lesions were defined as having high signal intensity on diffusion-weighted imaging (DWI) and low signal intensity in apparent diffusion coefficient (ADC) maps. Subacute lesions on MRI were defined as high density signal on DWI without corresponding signal on ADC maps [13]. Due to low occurrence of subacute lesions on MRI, acute and subacute lesions were evaluated together as acute lesions in further assessments. Chronic lesions on CT were defined as areas with low density with negative mass effect [12] and on MRI as areas of low signal intensity in the presence of gliosis and cystic encephalomalacia on FLAIR images [13, 14]. To distinguish silent brain infarctions from dilated Virchow-Robin spaces and leukoaraiosis, additional criteria were used such as a lesion size of minimum 3 mm [15], specific shape, and localization [16]. All lesions were attributed to either right or left anterior circulation (internal carotid artery territory) or posterior circulation (vertebrobasilar territory) [17]. Localization of lesions was categorized as cortical, subcortical, or localized in basal ganglia, thalamus, cerebellum, and brainstem, but one lesion could affect several structures. The size of the largest acute lesion in each patient was measured as the maximum lesion diameter in axial plane on CT or on B1000 on MRI. The infarction volume, measured on B1000 sequence, was calculated as the sum of manually drawn areas in all slices affected by infarction multiplied by the slice thickness and spacing [volume = SUM of all affected areas x (slice thickness + spacing)] [18]. Acute lesions were defined as scattered if two or more lesions were localized in the same territory and as multi-territorial if at least two different arterial territories had acute lesions. The presence of fetal type of posterior communicating artery (PCOM) was noted to secure a true multi-territorial localization [19]. The amount of white-matter T2 hyperintense lesions was evaluated according to Fazekas scale dividing the white matter in periventricular and deep-white matter [20]. Each region was given a grade depending on the size and confluence of lesions: periventricular white-matter hyperintensities (PVWMH) (0 absent, 1 “caps” or pencil-thin lining, 2 smooth “halo”, 3 irregular PVWMH extending to deep-white matter) and deep-whitewhite-matter hyperintensities (DWMH) (0 absent, 1 puncate foci, 2 beginning confluence of loci, 3 large confluent areas) [20]. The scale was further dichotomized into two categories: 0 to 1 and 2 to 3 [21] as the latter category represents moderate to severe leukoaraiosis. An intracranial large-vessel occlusion (LVO) was defined as the involvement of the internal carotid artery terminus (ICA-T), the middle cerebral artery (MCA) mainstem with or without involvement of a bifurcation branch (M1), the basilar artery (BA), or the vertebral artery (VA). A medium vessel occlusion (MeVO) was defined as an isolated proximal occlusion of the MCA bifurcation branch (M2), isolated occlusions of the M3 branch, isolated occlusion of the posterior cerebral artery (PCA), and isolated occlusion of the anterior cerebral artery (ACA) A1 or A2 segments, as well as the posterior inferior cerebellar artery (PICA), the anterior inferior cerebellar artery (AICA), and the superior cerebellar artery (SCA) [22].
Statistical evaluation
Statistical Package for Social Science (IBM SPSS Inc., version 26 for Windows) was used for statistical analysis. A p value < 0.05 was considered significant. Censoring of the data was performed at the time of death, dropout, or fulfilment of the study. Two patients died and did not complete the 12 months of electrocardiographic (ECG) follow-up and their AF status was assigned based on the status at dropout from the study. Differences in patient characteristics were tested using Chi-square test or Fisher’s exact test for categorical variables, and t test or Mann–Whitney U test for continuous variables. Prevalences of imaging aspects (frequency and percentages) were calculated for each group and logistic regression was used to estimate the probability of AF given each imaging aspect. Logistic regression results were presented as odds ratios and p values. A score consisting of the most common AF-related features in terms of patient characteristics and imaging findings and the combination of the ones with the highest discriminative ability was proposed and calculated for the patients with complete data on each feature. Receiver operating characteristic (ROC) curve was constructed for the proposed score and an optimal cut-off value dividing the population was defined in terms of optimal sensitivity and specificity. Sensitivity, specificity, positive predictive value, and negative predictive value were computed for the chosen cut-off value used for the dichotomization of the score. The dichotomized score was used as a predictor in a logistic regression model to evaluate its effect on the probability of AF. Furthermore, Kaplan–Meier curve and log-rank test were used to assess the association between the time to AF detection and proposed score.
Results
One hundred and six patients were included in this imaging sub-study (Fig. 2). ICMs were inserted at a median of 8 (7–11) days from the index stroke. AF or atrial flutter were detected in 31 patients (29.2%) during 12 months of continuous ECG follow-up, at a median of 12 (6–93) days. Patient characteristics are shown in Table 1. Patients with AF were significantly older, i.e., age ≥ 65 years was significantly associated with AF (p < 0.001). Furthermore, the AF group had significantly lower tobacco consumption and a higher pre-stroke CHA2DS2-VASC score than the non-AF group. The most prevalent stroke symptoms were numbness, weakness, and dysphasia. The latter was significantly more often seen in the AF than the non-AF group (p = 0.026).
One hundred and four patients (98.1%) underwent brain CT and 99 patients (93.4%) brain MRI. CT perfusion was done in 43 patients (40.6%). The number of patients included in the analysis and the imaging techniques used are shown in Fig. 2. Evaluated imaging (Fig. 2) was performed for CTA at a median of 1 (0 − 5) days, for MRI at a median of 2 (1 − 3) days, and for CT or control CT within 1 day from the onset of symptoms. Almost half of the included patients had verified chronic ischemia on brain imaging (Table 2), although only 22.6% had known history of previous stroke or TIA (Table 1) (only one patient with solely TIA). Within the group of patients with chronic lesions, patients with AF had more often prior clinical stroke or TIA than those without AF (57.1% vs 27.8%, p = 0.052). Chronic lesions were almost equally distributed in the studied population between anterior and posterior circulation, while acute lesions were predominantly located in the anterior circulation. Approximately 1 out of 3 patients had Fazekas scale > 1.
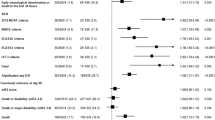
Patients with AF had more acute ischemic lesions with diameter ≥ 10 mm (OR 3.52 95% CI 1.11 − 11.18), and more often MeVO (OR 3.73 95% CI 1.23 − 11.32) than patients without AF. After Fazekas scale categorization, PVWMH score ≥ 2 was associated with almost three times higher odds of AF than lower score (OR 2.93 95% CI 1.23 − 6.95) (Table 3). Multi-territorial ischemic lesions were slightly more frequent in patients without AF (Table 3). However, there were no significant differences in acute and chronic lesions between the groups. (Table 3). Additional three patients had a vessel occlusion detected, though these were evaluated as chronic occlusions and were therefore not included in calculations.
Based on the patient characteristics and imaging analyses, a score for AF detection was constructed consisting of characteristics that were more common in the AF group than the non-AF group, the combination of which reached the highest discriminative ability. The score consisted of six features, each contributing 1 point to the total score (range 0–6 points); chronic cortical or cerebellar lesions, acute cortical lesions, acute lesion size ≥ 10 mm, PVWMH score ≥ 2, vessel occlusion, and age ≥ 65 years. (Table 4). A score of three points was chosen as an optimal cut-off value to divide the population (Fig. 3A). The AUC for the proposed score was 0.735 (0.634 − 0.836). Including symptoms of dysphasia slightly improved its discriminative ability, (AUC 0.752 vs 0.735), as well as inclusion of only MeVO (AUC 0.753 vs 0.735). The chosen cut-off gave a sensitivity of 93.3% (95% CI 77.9 − 99.2%), a specificity of 47.9% (95% CI 36.1 − 60.0%), a PPV of 42.4% (95% CI 30.3 − 55.2%), and an NPV of 94.6% (95% CI 81.8 − 99.3%). Patients with score ≥ 3 points had 12.9 times higher the odds of AF 95% CI (2.86 − 58.15) in comparison to the patients with a lower score. In this population, the AF-detection rates reached 42.4%, while in the population with lower scores this was only 5.4% (only two patients with AF). Based on the log-rank test, score ≥ 3 points was associated with higher cumulative hazard of AF as well as its earlier detection, p < 0.001 (Fig. 3B). The proportions of patients for each score value are shown in Fig. 3C, grouped by AF status. Including dysphasia in the proposed score increased the AUC but changed the cut-off value to 4 points, resulting in a lower sensitivity and NPV, 83.3% and 90.0% respectively. For score including MeVO only, the sensitivity and NPV were the same as for the proposed score with all-vessel occlusions.
Panel A shows the Receiver operating characteristics (ROC) curve for the proposed AF prediction score and the optimal cut-off value (circle). Panel B shows the Kaplan–Meier curve for subgroups of patients defined by the dichotomized score, cumulative hazard of atrial fibrillation (AF) in these groups, and association with the time to first verified episode of AF. Panel C shows the number of patients with each score value (height of the bars), grouped by the AF status. The proportion (%) of AF-positive patients for each score is given above each bar
Discussion
In our study, CS and cryptogenic TIA patients with AF detected by ICMs within 12-month follow-up had more often PVWMH, acute ischemic lesions with diameter ≥ 10 mm, and MeVO than patients without AF. Other previously described imaging findings believed to predict AF such as acute cortical and multi-territorial stroke or LVO were not significantly associated with AF in the studied population. However, the combination of specific imaging and clinical features showed a good ability to predict AF in patients with CS and cryptogenic TIA.
The effectiveness and usefulness of prolonged cardiac-rhythm monitoring for AF detection in CS patients have been shown in multiple studies and meta-analyses [3, 4, 23], but only a few of them focused on brain imaging and its utility in AF prediction (Table 5). In a recent meta-analysis, bilateral and multi-territorial lesions on MRI in patients with acute ischemic stroke were associated with cardioembolic stroke [24]. In our study, neither of these characteristics were significantly different between patients with and without AF which is in line with the results from other CS studies using prolonged cardiac-rhythm monitoring (Table 5). Acute cortical lesions represent another imaging characteristic shown to be predictive of AF in multiple studies [5, 21, 25]. In our cohort, this trend was also observed, however this was not statistically significant. These results are similar to other studies (Table 5) except for a study by Kass-Hout et al. that found association between cortical lesions and underlying AF [26]. In terms of the size of acute lesions, several cut-off values for lesion diameter have been used in studies with prolonged cardiac monitoring such as 5 mm [27] or 20 mm [28] and studies proposing scoring systems with a diameter over 4 cm [6]. The total size and volume of acute ischemic lesions in our study was lower than size and volume seen in a general AF-stroke population which most likely reflects the inclusion of patients with low disability and mild to moderate strokes in CS studies with prolonged monitoring [28,29,30]. In our population, we chose a diameter of 10 mm as it divided the population best and performed well as a part of the proposed score.
Only a few CS studies described ischemic lesions [27, 28, 30]. No significant association was found between chronic lesions and AF detection in our study. Bernstein et al. found that the presence of any chronic lesion was associated with AF [27], and Favilla et al. found an association particularly for cortical or cerebellar stroke [31]. Even though not significant, patients with AF in our study had more often chronic cortical and cerebellar lesions than those without AF particularly when both localizations were affected. The importance of the evaluation of chronic lesions was also emphasized by the fact that the frequency of chronic lesions in our cohort was two times higher than the frequency of clinical stroke or TIA cases. Simultaneously, clinical stroke or TIA were more often seen in patients with AF than those without. WMH is also a feature that is not often analyzed as it has mostly been related to small vessel disease rather than AF. Presence of any degree of WMH was not associated with AF in our study, but if categorized to PWMH and DWMH [21], more advanced PWMH (score ≥ 2) was predictive of AF. Results from other studies are inconclusive in terms of the differences between PWMH and DWMH in relation with AF [32, 33], and the general contribution and role of AF in WMH development [34]. Nevertheless, several CS studies with prolonged cardiac monitoring [27, 28, 30] as well as population studies found a strong association with AF [32, 35].
Large and medium vessel occlusions have been shown to be predictive of AF in several studies [29, 36, 37]. In our population, vessel occlusion was numerically more frequent in AF than non-AF group. Particularly, MeVO was significantly associated with AF, and patients with MeVo had almost four times increased odds of AF. However, there were also some patients with probable chronic occlusions that were not included in the calculations. In the proposed score both proximal and distal vessel occlusions were included to make the score more applicable for clinical use. Most studies with prolonged monitoring did not focus on vessel occlusions. Sudacevschi et al. did not find association between occlusions or stenosis detected on MRI and AF [30]. However, Doijiri et al. found both LVO and M2 and M3 occlusions to be an independent predictor of AF [38].
Generally, our study showed similar results to other comparable studies. The main differences with other studies were shorter cut-offs for AF duration at 30 s [28, 31, 39] or even shorter [31], later initiation and shorter length of monitoring (Table 5), and also inclusion of patients with PFO [28, 39] that had been shown to have another lesion pattern than AF-related stroke [40].
Based on the results from our and previous studies, individual imaging findings alone are likely not robust enough for AF prediction. Development of reliable scores consisting of several imaging criteria as well as clinical characteristics could be helpful in recognizing patients with underlying AF and secure wider availability of ICMs for CS patients. Our suggested score was comparable to other clinical scores in terms of predictive ability for AF with AUC of 0.735 [41] with sensitivity and NPV over 90% for three or more features resulting in 12 times higher probability of AF than in those with less but it needs further validation in another CS cohort. Proposed aspects are also feasible in terms of evaluation by physicians treating CS patients. At 12-month follow-up, other possible etiologies were discovered such as malignancy or antiphospholipid syndrome that could also present with characteristics similar to AF such as multi-territorial stroke [42]. However, this represents a normal-CS population that also consists of other diagnoses beside AF which can be revealed after some time [11]. Consequently, no patients were excluded from the analysis, even if a probable etiology was revealed after 1 year of follow-up only.
Strengths and limitations
All patients included in the study underwent very thorough diagnostic work-up before the diagnosis of CS was made. Furthermore, all patients were followed extensively for underlying AF for a period of 12 months and continuous cardiac-rhythm monitoring was initiated early after the index stroke. A large number of radiological parameters, including specifications on the extension of WMH and the size of acute lesions, were evaluated by an experienced neuroradiologist blinded to clinical data. Furthermore, lesions were attributed to all affecting structures, not just one. In addition, fetal PCOM was noted in all patients to correctly identify multi-territorial stroke.
One of the limitations is that only the largest ischemic lesions were measured due to the large number of acute lesions that were mainly very small in size and present in only few CT or MRI slices. However, all the consequent lesions were smaller in size and categorization of patients based on a specific diameter and volume cut-off unified the data and was performed also in other studies [27, 28]. Some studies found that even patients with AF can have small subcortical lesions, although lacunar stroke was an exclusion criterion in our cohort since the etiology in these patients was determined. A large proportion of AF patients in our study had lesions affecting subcortex, however particular measurements of solely subcortical lesions were not performed. Another limitation is that only one neuroradiologist performed the blinded assessments without an additional evaluator.
Conclusion
Combining imaging and clinical characteristics in a prediction score consisting of 6 features (age ≥ 65 years, chronic cortical or cerebellar lesions, acute cortical lesions, PVWMH ≥ 2, vessel occlusion, and acute lesion size ≥ 10 mm) performed well to discriminate between AF- and non-AF patients. The presence of three or more features predicted underlying AF in this cryptogenic stroke and TIA population.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Adams HP, Bendixen BH, Kappell LJ, Biller J, Love BB, Gordon DL et al (1993) Classification of subtype of acute ischemic stroke : definitions for use in a multicenter clinical trial. Stroke (1970) 24(1):35–41
Hart RG, Diener H-C, Coutts SB, Easton JD, Granger CB, O’Donnell MJ et al (2014) Embolic strokes of undetermined source: the case for a new clinical construct. Lancet Neurol 13(4):429–438
Noubiap JJ, Agbaedeng TA, Kamtchum-Tatuene J, Fitzgerald JL, Middeldorp ME, Kleinig T et al (2021) Rhythm monitoring strategies for atrial fibrillation detection in patients with cryptogenic stroke: A systematic review and meta-analysis. IJC Heart Vasc 34:100780
Sposato LA, Cipriano LE, Saposnik G, Ruiz Vargas E, Riccio PM, Hachinski V (2015) Diagnosis of atrial fibrillation after stroke and transient ischaemic attack: a systematic review and meta-analysis. The Lancet Neurology 14(4):377–387
Li SY, Yang XM, Zhao XQ, Liu LP, Wang YL, Jiang Y et al (2019) Newly detected atrial fibrillation is associated with cortex-involved ischemic stroke. Chin Med J 132(17):2053–2058
Muscari A, Bonfiglioli A, Faccioli L, Ghinelli M, Magalotti D, Manzetto F et al (2017) Usefulness of the MrWALLETS Scoring System to Predict First Diagnosed Atrial Fibrillation in Patients With Ischemic Stroke. Am J Cardiol 119(7):1023–1029
Novotny V, Thomassen L, Waje-Andreassen U, Naess H (2017) Acute cerebral infarcts in multiple arterial territories associated with cardioembolism. Acta Neurol Scand 135(3):346–351
Ratajczak-Tretel B, Lambert AT, Johansen H, Halvorsen B, Bjerkeli V, Russell D et al (2019) Atrial fibrillation in cryptogenic stroke and transient ischaemic attack – the nordic atrial fibrillation and stroke (NOR-FIB) study: rationale and design. Eur Stroke J 4(2):172–180
Ratajczak-Tretel B, Tancin Lambert A, Al-Ani R, Arntzen K, Bakkejord GK, Bekkeseth H et al (2023) Atrial fibrillation in cryptogenic stroke and TIA patients in the nordic atrial fibrillation and stroke (NOR-FIB) study: main results. Eur Stroke J 8(1):148–156
Tancin Lambert A, Ratajczak-Tretel B, Al-Ani R, Arntzen K, Bakkejord GK, Bekkeseth HMO et al (2023) Biomarkers predictive of atrial fibrillation in patients with cryptogenic stroke. Insights from the nordic atrial fibrillation and stroke (NOR-FIB) study. Eur J Neurol 30(5):1352–1363
Ratajczak-Tretel B, Lambert AT, Al-Ani R, Arntzen K, Bakkejord GK, Bekkeseth HMO et al (2023) Underlying causes of cryptogenic stroke and TIA in the nordic atrial fibrillation and stroke (NOR-FIB) study - the importance of comprehensive clinical evaluation. BMC Neurol 23(1):115
Bell DJ. Ischaemic stroke. 2022 [Available from: https://radiopaedia.org/articles/ischaemic-stroke?lang=gb.
Allen LM, Hasso AN, Handwerker J, Farid H (2012) Sequence-specific MR imaging findings that are useful in dating ischemic stroke. Radiographics 32(5):1285–1297
De Cocker LJL, Lövblad K-O, Henikse J (2017) MRI of Cerebellar Infarction. Eur Neurol 77(3–4):137–146
Bokura H, Kobayashi S, Yamaguchi S (1998) Distinguishing silent lacunar infarction from enlarged Virchow-Robin spaces: a magnetic resonance imaging and pathological study. J Neurol 245(2):116–122
Liu J. Perivascular spaces. 2022 [Available from: https://radiopaedia.org/articles/perivascular-spaces?lang=gb.
Smithuis R. Vascular territories. 2008 [Available from: https://radiologyassistant.nl/neuroradiology/brain-ischemia/vascular-territories.
Enriquez BAB, Nome T, Nome CG, Tennøe B, Lund CG, Beyer MK et al (2023) Predictors of outcome after endovascular treatment for tandem occlusions: a single center retrospective analysis. BMC Neurol 23(1):82
Zampakis P, Panagiotopoulos V, Petsas T, Kalogeropoulou C (2015) Common and uncommon intracranial arterial anatomic variations in multi-detector computed tomography angiography (MDCTA). What radiologists should be aware of. Insights Imag 6(1):33–42
Fazekas F, Chawluk JB, Alavi A, Hurtig HI, Zimmerman RA (1987) MR signal abnormalities at 1.5 T in Alzheimer’s dementia and normal aging. AJR Am J Roentgenol 149(2):351–356
Liu R, Yang X, Li S, Jiang Y, Wang Y, Wang Y (2017) Novel composite scoring system to predict unknown atrial fibrillation in acute ischemic stroke patients. Brain Res 1674:36–41
Saver JL, Chapot R, Agid R, Hassan A, Jadhav AP, Liebeskind DS et al (2020) Thrombectomy for Distal, Medium Vessel Occlusions: A Consensus Statement on Present Knowledge and Promising Directions. Stroke (1970) 51(9):2872–2884
Tsivgoulis G, Palaiodimou L, Triantafyllou S, Köhrmann M, Dilaveris P, Tsioufis K et al (2022) Prolonged cardiac monitoring for stroke prevention: A systematic review and meta-analysis of randomized-controlled clinical trials. Eur Stroke J 8(1):106–116
Sharobeam A, Churilov L, Parsons M, Donnan GA, Davis SM, Yan B (2020) Patterns of infarction on MRI in patients with acute ischemic stroke and cardio-embolism: a systematic review and meta-analysis. Front Neurol 11:606521
Rizos T, Bartsch AJ, Johnson TD, Dittgen F, Nichols TE, Malzahn U et al (2017) Voxelwise distribution of acute ischemic stroke lesions in patients with newly diagnosed atrial fibrillation: Trigger of arrhythmia or only target of embolism? PLoS ONE [Electronic Resource] 12(5):e0177474
Kass-Hout O, Kass-Hout T, Parikh A, Hoskins M, Clements SD Jr, Rangaraju S et al (2018) Atrial Fibrillation Predictors on Mobile Cardiac Telemetry in Cryptogenic Ischemic Stroke. The Neurohospitalist 8(1):7–11
Bernstein RA, Di Lazzaro V, Rymer MM, Passman RS, Brachmann J, Morillo CA et al (2015) Infarct Topography and Detection of Atrial Fibrillation in Cryptogenic Stroke: Results from CRYSTAL AF. Cerebrovasc Dis 40(1–2):91–96
Vollmuth C, Stoesser S, Neugebauer H, Hansel A, Dreyhaupt J, Ludolph AC et al (2019) MR-imaging pattern is not a predictor of occult atrial fibrillation in patients with cryptogenic stroke. J Neurol 266(12):3058–3064
Arsava EM, Bas DF, Atalar E, Has AC, Oguz KK, Topcuoglu MA (2015) Ischemic stroke phenotype in patients with nonsustained atrial fibrillation. Stroke 46(3):634–640
Sudacevschi V, Bertrand C, Chadenat ML, Tarnaud C, Pico F (2016) Predictors of Occult Atrial Fibrillation in One Hundred Seventy-One Patients with Cryptogenic Transient Ischemic Attack and Minor Stroke. J Stroke Cerebrovasc Dis 25(11):2673–2677
Favilla CG, Ingala E, Jara J, Fessler E, Cucchiara B, Messe SR et al (2015) Predictors of finding occult atrial fibrillation after cryptogenic stroke. Stroke 46(5):1210–1215
de Leeuw FE, de Groot JC, Oudkerk M, Kors JA, Hofman A, van Gijn J et al (2000) Atrial fibrillation and the risk of cerebral white matter lesions. Neurology 54(9):1795–1801
Mayasi Y, Helenius J, McManus DD, Goddeau RP Jr, Jun-O’Connell AH, Moonis M et al (2018) Atrial fibrillation is associated with anterior predominant white matter lesions in patients presenting with embolic stroke. J Neurol Neurosurg Psychiatry 89(1):6–13
Gurol ME (2018) Atrial fibrillation and FLAIR/T2 white matter hyperintensities on MRI. J Neurol Neurosurg Psychiatry 89(1):1–2
Nakanishi K, Jin Z, Homma S, Elkind MSV, Rundek T, Schwartz JE et al (2019) Night-time systolic blood pressure and subclinical cerebrovascular disease: the Cardiovascular Abnormalities and Brain Lesions (CABL) study. Eur Heart J Cardiovasc Imaging 20(7):765–771
Chang A, Ricci B, Grory BM, Cutting S, Burton T, Dakay K et al (2019) Cardiac Biomarkers Predict Large Vessel Occlusion in Patients with Ischemic Stroke. J Stroke Cerebrovasc Dis 28(6):1726–1731
Kalinin MN, Khasanova DR, Ibatullin MM (2017) The hemorrhagic transformation index score: a prediction tool in middle cerebral artery ischemic stroke. BMC Neurol 17(1):177
Doijiri R, Yamagami H, Morimoto M, Iwata T, Hashimoto T, Sonoda K et al (2020) Paroxysmal Atrial Fibrillation in Cryptogenic Stroke Patients With Major-Vessel Occlusion. Front Neurol 11:580572
Makimoto H, Kurt M, Gliem M, Lee JI, Schmidt J, Muller P et al (2017) High Incidence of Atrial Fibrillation After Embolic Stroke of Undetermined Source in Posterior Cerebral Artery Territory. J Am Heart Assoc 6(12):29
Stecco A, Quagliozzi M, Soligo E, Naldi A, Cassarà A, Coppo L et al (2017) Can neuroimaging differentiate PFO and AF-related cardioembolic stroke from the other embolic sources? Clinical-radiological correlation on a retrospective study. Radiol Med 122(6):412–418
Ratajczak-Tretel B, Lambert AT, Al-Ani R, Arntzen K, Bakkejord GK, Bekkeseth HMO et al (2023) Prediction of underlying atrial fibrillation in patients with a cryptogenic stroke: results from the NOR-FIB study. J Neurol 270(8):4049–4059
Yang W, Kang DW, Kim JM, Jung KH, Lee SH (2022) Neuroimaging features of antiphospholipid antibody-related stroke compared with atrial fibrillation-related stroke. Sci Rep 12(1):11686
Gaillard N, Deltour S, Vilotijevic B, Hornych A, Crozier S, Leger A et al (2010) Detection of paroxysmal atrial fibrillation with transtelephonic EKG in TIA or stroke patients. Neurology 74(21):1666–1670
Bhatt A, Majid A, Razak A, Kassab M, Hussain S, Safdar A (2011) Predictors of occult paroxysmal atrial fibrillation in cryptogenic strokes detected by long-term noninvasive cardiac monitoring. Stroke Res Treat 2011:172074
Rabinstein AA, Fugate JE, Mandrekar J, Burns JD, Seet RC, Dupont SA et al (2013) Paroxysmal atrial fibrillation in cryptogenic stroke: a case-control study. J Stroke Cerebrovasc Dis 22(8):1405–1411
Acknowledgements
We gratefully honor the late Professor David Russell for his contribution and leadership in this research.
Funding
Open access funding provided by Østfold Hospital Trust. NOR-FIB is an investigator driven academic study, supported by Oslo University Hospital, Norwegian Health Association, South-Eastern Norway Regional Health Authority, Østfold Hospital Trust and the European Cerebrovascular Research Infrastructure (ECRI). Devices were partly provided by Medtronic.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
DA has received honoraria and consultation fees from Actelion, Amgen, AstraZeneca, BMS, Bayer, Boehringer Ingelheim, MSD, Novartis, Pharmacosmos, Philips, Pfizer, Roche Diagnostics, Sanofi, Takeda, and Vifor Pharma, and research funding (to the institution) from BMS/Pfizer, Bayer, Roche Diagnostics and Medtronic. AHA has received travel support, and honoraria for advice or lecturing from Bayer, Boehringer Ingelheim, BMS, Abbvie, Teva, Novartis, Roche, Pfizer, and Teva, research grant from Boehringer Ingelheim, and partial financial support from Medtronic and BMS for operating costs in ongoing clinical studies. ATL and BRT have received travel funding from Medtronic and are funded by a PhD fellowship from Helse Sør-Øst (South-Eastern Norway Regional Health Authority).
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lambert, A.T., Sætre, D.O., Ratajczak-Tretel, B. et al. Imaging features for the identification of atrial fibrillation in cryptogenic stroke patients. J Neurol 271, 5343–5356 (2024). https://doi.org/10.1007/s00415-024-12397-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-024-12397-y